Do I Need To Follow A Specific Diet If I Have Ulcerative Colitis
There is no specific diet for ulcerative colitis and you will only make short term modifications to your diet to preserve or promote your nutritional status or to improve symptoms. It is important to note that dietary changes can only help to improve symptoms and will not reduce inflammation in your bowel.
Read Also: How To Treat Sacral Pressure Ulcer
When Is Surgery Necessary For Ulcerative Colitis
There are two main reasons you might have to undergo surgery:
- If youre unable to tolerate or have stopped responding to your UC medications
- If you develop colon cancer
The standard surgery to treat UC is a proctocolectomy, which removes both your colon and your rectum, which collectively is known as your large intestine, Dr. Taleban said. The most common type of proctocolectomy procedure is the J-pouch surgery, where the small bowel is used to make a pouch which is then connected to the anus so a patient can pass stool as before.
Steamed Or Broiled Fatty Fish
Youâll want to steer clear of fried foods, since they can make stomach problems worse. But fish like sardines, salmon, and mackerel are great choices if you broil or steam them. Thatâs because theyâre rich in omega-3 fatty acids, which fight inflammation. They can also help you get protein and vitamin D.
Recommended Reading: Bed To Prevent Pressure Ulcers
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
What Should I Eat During A Flare
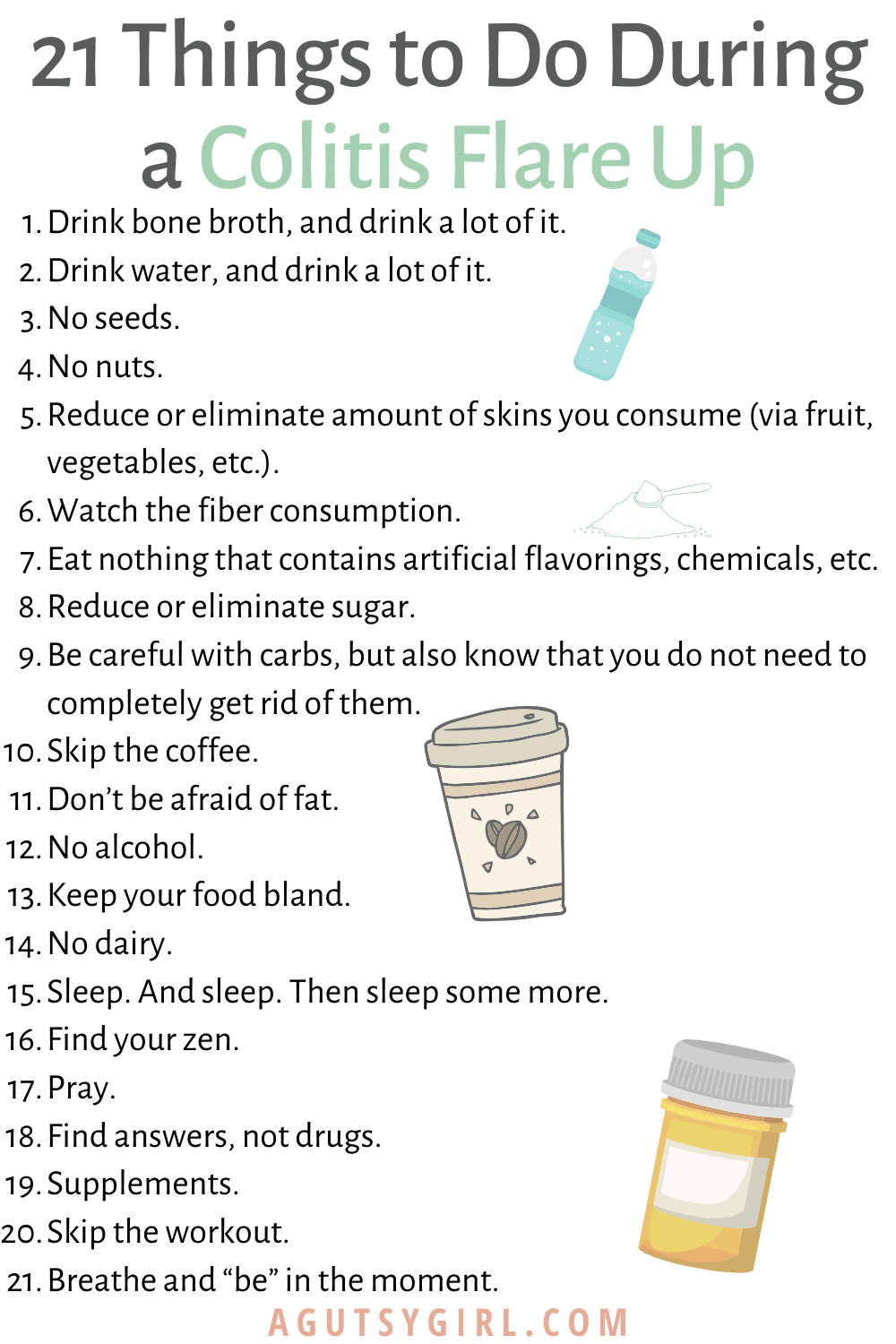
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Also Check: How To Treat Sacral Pressure Ulcer
What Do Colon Spasms Feel Like
It is usual for people who have colon spasms to have sudden, intense abdominal discomfort, particularly in the lower abdomen and on the left side. The degree to which each spasm hurts might change from one episode to the next. Symptoms of bloating or gas. These symptoms might appear at any moment of the day, notwithstanding the diet that one follows.
Can Certain Foods Really Cause Inflammation
The link between what we eat and chronic inflammation in the body isnt fully understood. What is known is that there does seem to be some connection.
Lets jump into the science: The liver produces something called C-reactive protein as a response to inflammation in the body. In short, higher levels of CRP mean more inflammation, and certain foods have been shown to increase levels of CRP in the blood.
Now, the specifics of what foods cause this increase is somewhat up for debate, but its possible that things like processed sugar can trigger the release of inflammatory messengerslike CRPa sign that they may potentially be contributing to an inflammatory state.
On the other hand, foods like fruits and vegetables may help fight oxidative stress, which is a trigger for inflammation. Certain diets, like the Mediterranean diet, already include many foods that are considered to be anti-inflammatory such as whole grains, legumes, a rainbow assortment of fruits and vegetables, and fish.
You May Like: Medical Nutrition Therapy For Diabetic Foot Ulcer
Foods To Eat During Ulcerative Colitis Flares
A bland diet is best during periods of active ulcerative colitis, when you may experience abdominal discomfort, blood in your stool, loss of appetite, fatigue, weight loss, vomiting, nausea, abdominal pain, and diarrhea. A safer diet during flares might include dry toast, applesauce, and white rice. Although some foods are more likely to be safe for those with UC, individual experiences can vary, especially during flares.
Here are some safer foods to try during ulcerative colitis flares:
- Low-fiber refined grains, such as oatmeal, potatoes, and sourdough bread
- Well-cooked vegetables that are easier to digest
- Vegetable broth, which can be added to grains like rice for additional nutrients
- Fruits or vegetables that contain more soluble fiber than insoluble fiber, such as bananas, carrots, and apples
- Bland protein, such as nut butters, eggs, tofu, and chicken
Diarrhea specifically raises concerns for loss of nutrients, such as potassium, sodium, magnesium, and phosphorus, through bodily fluids. If you choose to drink an electrolyte beverage, choose low sugar versions such as G2, Propel, or BodyArmor Lyte. You can also cut regular Gatorade or BodyArmor with water, diluting it by half.
Uc And Lactose Intolerance
People with UC often think they have lactose intolerance, which means they cant properly digest the sugar in milk and milk products, because some symptoms are similar. But UC doesnât make you more likely to have lactose intolerance. Your doctor can do a simple test to find out.
If you can, keep milk and dairy products in your diet. They are a very good source of calcium and vitamin D, which keep your bones healthy. Using steroids such as prednisone for a long time can thin your bones and make it harder for your body to absorb calcium, raising your chance of having osteoporosis.
If dairy products cause you discomfort, see if you can eat them in small amounts. Or try a lactase supplement to break down the lactose in dairy products.
If you just cant stomach dairy products, your doctor may want you to take calcium and vitamin D supplements. Watch a video on how dairy affects ulcerative colitis.
You May Like: Can Tylenol Cause Stomach Ulcers
Also Check: Turning Patients Every 2 Hours To Preventing Pressure Ulcers
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Best And Worst Foods For Ulcerative Colitis
-
Ulcerative colitis is an inflammatory bowel disease that can affect your appetite and the way your body absorbs nutrients. Certain foods seem to trigger uncomfortable symptoms, at least in some individuals. Diet is an important factor in the management of this chronic disease, but theres no one-size-fits-all ulcerative colitis diet. The best and worst foods for ulcerative colitis may depend on whether or not youre experiencing an ulcerative colitis flare. It will take time and experimentation to figure out which foods you can tolerate and which you should avoid.
You May Like: How To Cure Ulcerative Proctitis
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
You Could Develop Chronic Fatigue
When you have active inflammation, your body is running a marathon, Bonthala says. You waste a lot of energy. Research backs this up: A study published in the March 2020 issue of the Journal of Crohns and Colitis found that people who were in remission reported less fatigue than people with active ulcerative colitis or Crohns disease, another type of IBD.
Recommended Reading: What Foods Irritate An Ulcer
Signs And Symptoms Of Ulcerative Colitis
The most common UC symptom is bloody diarrhea or pus in the stool. Besides, other symptoms include:
- Sudden and frequent need to poop
- Cramping bowel pain
- Canker sores
- Pain or bleeding with bowel movements
Although ulcerative has no cure, knowing what to eat with colitis can effectively mitigate the on-and-off cycle of these symptoms, and can aid in the reduction of inflammation and risk of flare.
What Foods Should I Eat When My Ulcerative Colitis Is In Remission
You should try and maintain a diverse and nutrient-rich diet even when you are in remission and your symptoms have reduced or gone away completely. Keep a food diary and introduce new foods slowly, so you understand which ones trigger your symptoms. Keep well hydrated with water, broth, tomato juice, or rehydration solutions, and avoid making large changes in your diet without your doctors advice. Eat foods such as:
- Fiber-rich foods such as oat bran, beans, barley, nuts, and whole grains, unless your doctor has advised you to stick with a low fiber diet or you have an ostomy or intestinal narrowing
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Fruits and vegetables of all colors remove the peel and the seeds if they trigger your symptoms
- Calcium-rich foods found in collard greens, yogurt, kefir, and milk
- Probiotic foods such as yogurt, kimchi, miso, sauerkraut, or tempeh.
Read Also: What Do I Take For An Ulcer
General Guidelines When Ulcerative Colitis Is In Remission
Some members of MyCrohnsAndColitisTeam find they can eat a wider variety of foods safely during remission periods when ulcerative colitis is not as active and symptoms are absent or mild. Still, every individual is different, and purportedly beneficial foods may trigger symptoms. Trial and tracking is the only way to know for sure.
If it is safe for you, these guidelines may help you stay your healthiest during remission:
- Get 25 grams to 35 grams of fiber per day to promote bowel regularity and reduce inflammation.
- Consume plenty of lean meats, which are a good source of B vitamins. Include fatty fish, tofu, and nut and seed butters.
- Include probiotic foods such as yogurt, tempeh, kefir, kimchi, miso, and sauerkraut.
While some members find kefir too sour for their liking, others report experiencing benefits from trying the fermented drink. Kefir has been helping me over the past week, wrote one. Been trying kefir the past few days. Will keep you posted. So far less pain, said another.
Back Up: What Is Ulcerative Colitis Exactly
Ulcerative colitis is a type of inflammatory bowel disease that causes ulcers and sores in the lower quarter to third of your digestive tract. Typically, these ulcers are found in your rectum or in the inner lining of your lower intestine . This can cause bloody diarrhea, the most common symptom of ulcerative colitis, but you might also experience things like abdominal cramping, constipation, and a general sense of fatigue. Weight loss and a loss of appetite can also crop up, per the U.S. National Library of Medicine.
Diana Whitehead, M.D., director of the Inflammatory Bowel Disease Center at the Greater Baltimore Medical Center, explains that though ulcerative colitis has a strong genetic component, symptoms are often set off by a triggering event that activates inflammation in the lower intestine. Basically, your immune system is not doing what it should do, which is to protect you, but its gone kind of into overdrive, Dr. Whitehead says. In other words, even though the exact causes of ulcerative colitis arent fully understood, experts consider it to be an autoimmune condition thats set off by this overreaction in the gut.
You May Like: Do Probiotics Help Stomach Ulcers
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
Don’t Miss: Best Way To Heal Stomach Ulcers
Fruit Or Vegetable Juices
After a flare of Crohnâs disease or ulcerative colitis, you may not feel like eating much. But you need calories and nutrients, so start your diet again slowly. Fruit or vegetable juices are great when you donât have much of an appetite. They give you vitamins plus hydration without weighing you down. Just choose one without pulp — the fiber could cause cramping or bloating. You may want to water down your juice if itâs high in sugar, since too much of the sweet stuff could trigger diarrhea.
Find Ways To Chill Out

All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Recommended Reading: List Of Foods To Avoid With Ulcerative Colitis
What Foods Are Best For Colitis
- Fish: salmon, tilapia, flounder Pork primals and other lean slices Chicken breasts and thighs Eggs provide a supplementation for a number of necessary nutrients, including omega-3 fatty acids.
- They are often simple for the body to process.
- And last, for diets based on plants: Soy Tofu that is firm If you have ulcerative colitis, see our comprehensive list of foods that are safe to consume.
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Read Also: Ulcerative Colitis And Mental Health