Foods That May Fight Uc
Some research shows that certain nutrients may help fight the irritation and swelling in your gut caused by UC. Scientists have studied how linoleic acid affects people with the condition. Although everyone needs this “good” fat, donât overdo it, since there is some evidence it may play a role in inflammation if you get too much.
Other studies show that an omega-3 fatty acid called EPA may fight inflammation. This is another âgoodâ fat that blocks certain chemicals in your body called leukotrienes. Fish oil is a good source of EPA. In some studies, folks with UC saw some benefits when they took high doses. Many people, though, didn’t like the fishy taste. There is also some evidence that adding fish oil to aminosalicylates may be helpful, but this isnât proven. DHA is another omega-3 found in fish oil that can fight inflammation and is used by some people with UC.
Some research also shows that yogurt with gut-healthy bacteria, called probiotics, eases inflammation. Scientists are still studying how they may help people with UC and similar conditions. Some people also believe that a diet low in FODMAPs — a type of highly-fermentable carbs found in meats, fruits, dairy, and lots of other foods — may help ease UC symptoms. But the evidence is unclear if it does. And without close monitoring, any diet that restricts certain foods may lead to poor nutrition and other problems.
Show Sources
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
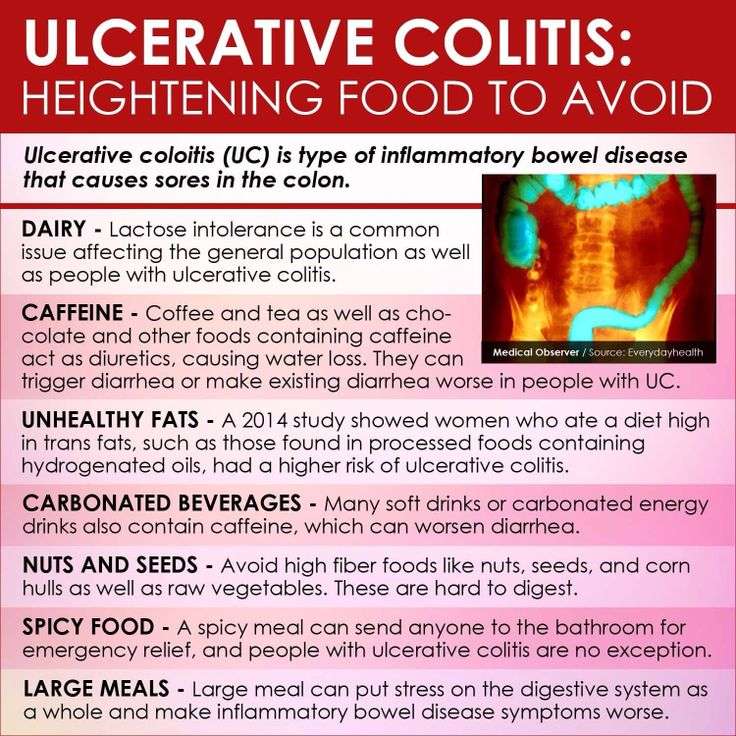
What Foods Should I Avoid
Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.
Also Check: Is Oatmeal Ok To Eat With Ulcerative Colitis
Ulcerative Colitis: This Is Why You’re Here Right
- Why did you get Ulcerative Colitis? The short answer is that scientists still don’t know. Genetics are a major risk factor, but some people without a family history develop the condition
- Ulcerative Colitis is caused by an autoimmune response from your body
- Your symptoms may include:
- GI: loose and urgent bowel movements, bloody stool, abdominal pain and cramps, persistent diarrhea
- Non-GI: appetite loss, weight loss, nausea, low energy, anemia
- There are flares and periods of remission throughout disease course UC is different from other types of colitis because tiny ulcers form, causing long term inflammation
The Nutritional Impact Of Uc
Changes in diet and nutrition are one part of a multifaceted approach for treating ulcerative colitis and other IBD conditions. Your doctor also will likely prescribe medication. In more severe cases, surgery may be needed, to repair or remove damaged portions of the colon.
Malnutrition, dehydration, and weight loss are major health risks of UC. When the colon becomes inflamed and ulcerated, its less able to absorb fluids and nutrients needed to help sustain your body.
Diarrhea, a symptom of UC, also increases loss of fluids and nutrients, such as sodium, potassium, magnesium, phosphorus, and zinc.
In severe cases, people with UC may need IV fluids to replace these lost nutrients and fluids.
Other UC symptoms, such as abdominal pain and nausea, can further rob you of nutrition as they reduce your appetite, so you consume fewer calories and nutrients.
You May Like: How To Treat A Diabetic Foot Ulcer On The Sole
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
Watch out for items that can be troublemakers if you have UC, including:
Create A Plan That Works For You
If you have UC, informed dietary choices can make a big difference. Nutrition takes on special importance, especially since the disease can make it harder for your body to absorb calorie and nutrients. Choosing nutrient-rich foods is important.
Avoiding trigger foods is also key. They can make your symptoms worse. They can even keep your body from properly absorbing calories and nutrients from the foods you eat.
New research in mice shows that emulsifiers in processed foods like lecithin, polysorbate, and gums, weaken the intestinal mucous lining and negatively alter gut bacteria. This can potentially lead to more intestinal inflammation, flare-ups, and symptoms. More research is necessary to confirm these findings in humans, but the research findings are compelling enough for those with inflammatory bowel disease to consider reducing how much processed foods they eat.
For these reasons and more, a well-balanced diet is important. It can help minimize your symptoms and lower your risk of complications from UC.
Recommended Reading: New Biologic Drugs For Ulcerative Colitis
You May Like: Va Disability For Ulcerative Colitis
Seek Out A Professional
Creating a diet plan isnt easy, which is why its always a good idea to get professional help. Meeting, even just once, with a dietitian, can be a revelation in terms of diet and answering that question what do I eat? Our understanding of IBD and diet is always evolving, so fine-tuning a flare-up diet plan is an ongoing process, and checking in with a dietitian will be helpful.
Many people with IBD restrict foods when in a flare-up, but more calories are needed to prevent losing too much weight. A physician can help you understand weight loss and how much is too much.
Go Mediterranean During Remission
With UC, you’ll likely eat differently depending on whether you’re in remission or having a flare. During remission, the Mediterranean diet is ideal because of its focus on low-fat, anti-inflammatory foods. “People who follow a Mediterranean diet are less likely to experience flare ups,” says Mary Wirtz, R.D.N., a clinical dietician at the Mayo Clinic in Rochester, MN. One reason: “The diet avoids foods high in sugar and added fat, which we know can lead to inflammation.” Choose fish like salmon and tuna, rich in omega-3 fatty acids, as well as olive oil, whole grains, and fresh fruits and vegetables.
Read Also: Medications For Ulcers Over The Counter
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Green Banana & Applesauce
Both green bananas and cooked and cooled apples are high in soluble fibers and resistant starches which help to slow down transit and soak up excess moisture which can be helpful if diarrhea is a concern. According to theUniversity of Wisconsin Health, applesauce is helpful for ulcerative colitis and are a rich source of vitamins and minerals like potassium.
You May Like: How To Know If A Stomach Ulcer Is Bleeding
Common Supplements Recommended For Ibd Patients
Your healthcare provider may recommend that you take vitamin or mineral supplements, especially if you are experiencing nutritional deficiencies. We can help you learn about supplements that are commonly recommended for IBD patients.
This information can help you learn which vitamins and minerals are important to maintain your nutrition, along with the various foods you may want to try as part of your IBD-friendly diet.
Your body is unique. What works for one patient, will not work for everyone. Check with your healthcare providers before starting any supplements, as you will need proper dosing.
Foods Rich In Sulfur And Sulfites
Foods like beer, wine, shellfish, some dried fruits, white bread, and cured meats containsulfur, producing excess gas in the colon. Even without these foods, UC patients produce more hydrogen sulfide than usual, and they have difficulty breaking the gas down due to inflammation of the colonic wall. Hence, ingesting more foods with sulfur causes more damage to the colon.
You May Like: Is Ulcerative Colitis Considered A Disability
Fermented Foods Can Help Balance Gut Bacteria
Fermented foods like kefir, kombucha, and sauerkraut contain active probiotics, considered good bacteria, which can be helpful for some people with digestive problems, according to the Brigham and Womens Health Crohns and Colitis Center. Probiotic foods add good bacteria to the digestive tract, which can improve the health of the whole body, says Kelly Kennedy, RDN, staff nutritionist with Everyday Health.
According to a study published in August 2018 in the journal Frontiers of Microbiology, live probiotics in the gut can help regulate the immune system, too. Since UC is an autoimmune disease, people living with the condition may benefit from extra immune support.
Fermented foods are great by themselves kombucha tea, for example or as a garnish to any healthy dish, like kimchi over rice.
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
Recommended Reading: Holistic Cure For Ulcerative Colitis
Ulcerative Colitis Nutrition Must
Nutrition is vital in managing ulcerative colitis symptoms, andpeople with this condition must follow a balanced diet and consume enough nutrients.
Foods to eat if you have ulcerative colitisinclude the following.
#1: Protein
Inflammation caused by ulcerative colitis increases your body’s protein requirements. Protein deficiency can damage your body’s ability to heal and may lead to muscle loss.
There are many foods rich in protein, including:
Following are some tips for identifying food triggers and staying on track.
It Can Be Challenging To Differentiate Between Crohn’s And Ulcerative Colitis
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
|
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
You May Like: What Does Ulcerative Colitis Look Like
Tips For Meal Prepping
Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
Also Check: Simponi Dose For Ulcerative Colitis
Ingredients To Avoid If You Have Uc
When you experience a UC flare-up, you should avoid foods that may worsen symptoms such as frequent bowel movements, diarrhea, bloody stools, and stomach pain, as well as fatigue, loss of appetite, and weight loss.
Limiting sugar is especially important during a time of active diarrhea, as sugar can make this worse, says Kennedy. Id recommend avoiding added sugars at all costs and switching to unsweetened applesauce instead.
If youre thinking about using artificial sweeteners, that may not be such a wise choice, either.
Artificial sweeteners are controversial, with some people feeling that they could possibly be a trigger food for those with IBD, Kennedy explains. It would be a personal choice to include them in a colitis-friendly diet.
Although the evidence is thin, a review published in September 2021 in the journal Frontiers in Nutrition, suggest that artificial sweeteners might trigger inflammation-causing changes to the gut bacteria, which could be problematic for people with conditions like IBD.
People with UC may also be more sensitive to gluten, a protein thats found in grains such as wheat, rye, and barley. The symptoms of gluten intolerance include bloating and diarrhea.
There isnt an ideal frequency for indulging in sweets, but moderation is key. When youre not dealing with a flare, Kennedy says you may be able to indulge a little, but the main goal is to try to limit the chances of triggering UC symptoms.
Vitamin And Mineral Supplementation
Nutritional supplements are great for patients with inflammatory bowel disease who may need a bit of extra help preventing a nutritional deficiency.
Your healthcare providers may also recommend a vitamin and/or mineral supplementation plan if your tests show you already have a nutritional deficiency.
You may be able to get all your necessary vitamins and minerals from eating a well-balanced, nutrient-rich diet. But flares, severe symptoms, surgeries, and other complications may make it difficult for some patients with Crohns disease or ulcerative colitis to get enough nutrients from food alone.
Check with your doctor or other healthcare providers before taking any supplements, including over-the-counter medications, herbs, and other complementary therapies.
-
Some supplements can cause gastrointestinal symptoms, including nausea and diarrhea.
-
Check the labels on your supplements for lactose, artificial colors, sugar alcohols, or preservatives, all which can aggravate your IBD, especially when you are in a flare.
-
Most supplements should not be taken on an empty stomach.
Video Length00:02:00
Vitamin and Mineral Supplementation in IBD Often times, when you have Crohn’s disease or ulcerative colitis, you may need to take vitamins or minerals to prevent or make up for a nutritional deficiency. Watch and listen this video to learn more about common vitamin and mineral supplements for IBD patients.
Don’t Miss: How Do You Get Ulcers In Your Stomach