How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Bleeding In Ulcerative Colitis
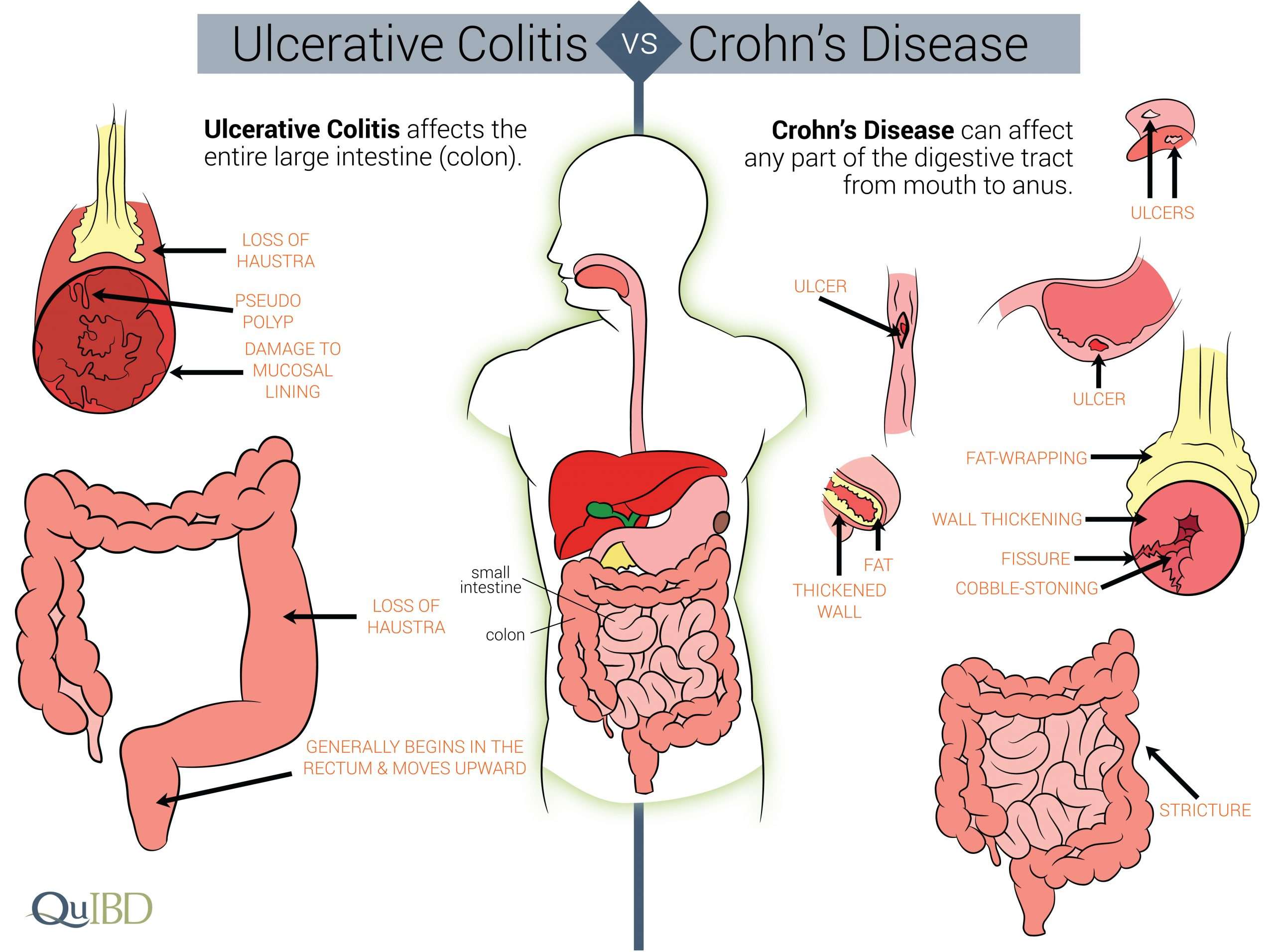
Bleeding from the rectum is more common in ulcerative colitis than it is in Crohn’s disease.
Ulcerative colitis often involves the rectum. Because the rectum is at the end of the large intestine, blood from this source is quite visible in or on the stool.
Bleeding also occurs with ulcerative colitis because this form of IBD attacks the lining of the large intestine. The ulcers that form in the mucosa of the large intestine tend to bleed.
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Read Also: How Do You Know If You Have A Stomach Ulcer
Some Doctors May Use The Following Table To Classify Your Symptoms*:
*A patient does not need to have all of these factors to be considered in a specific category of disease
Ulcerative colitis symptoms are considered moderate when you experience between 4-6 stools per day which include a moderate amount of blood. Severe UC is when you experience 6-10 per day with a severe amount of blood when passing.
If youre concerned about any of your symptoms, talk to your doctor immediately.
Tips For Healthy Ulcerative Colitis Poop
There are several different approaches to UC treatment. Medications, diet, and other lifestyle changes can all help improve bowel symptoms in UC.
The foremost treatment for ulcerative colitis inflammation and related stool changes is medication. These include:
- Aminosalicylates such as Asacol or Azulfidine , to reduce inflammation
- Corticosteroids such as prednisone and Entocort EC , to reduce inflammation
- Immunomodulators such as Imuran or cyclosporine, to reduce your immune system response
- Biologic therapies such as Remicade or Simponi , to neutralize proteins made by the immune system and reduce inflammation
Your diet also plays a role in your bowel habits. After all, what goes in, must go through and come out. The following diet modifications may help reduce bowel symptoms:
- Avoid your individual trigger foods.
- Limit dairy products.
- Drink plenty of water throughout the day.
- Eat small meals.
Stress is another factor that can contribute to changes in the stool. The brain-gut connection may play a role in inflammation of the GI tract. Managing your stress levels might be able to decrease diarrhea and other changes in your stool.
In addition, participating in regular physical activity is healthy for the GI tract. Exercise helps with the movement of stools, which can be especially helpful for constipation.
Also Check: Venous Leg Ulcer Dressing Treatment
What To Do When Uc Symptoms Are Abnormal Or Severe
What do you do once youve determined that the symptoms you’re experiencing don’t fit into your realm of “normal?” If your abnormal symptoms are manageable, meaning that you might feel icky, but can still somewhat function, call your GI doctor.
If your particular doctor is unavailable, call the on-call GI doctor. Let them know what you’re experiencing and ask them to get back to you as your symptom isn’t normal. You can always leave a message with a nurse or contact your GI through an online portal if you can’t get ahold of them on the phone.
In cases when your symptoms are severe , go to the emergency room. That means if you’re unable to walk, move, or speak due to pain or cramping, or if you’re incoherent, the emergency room is your best bet. However, in cases where you might be seeing more blood than usual, or your pain level is slightly elevated, there’s not much an emergency room can do for you, and, more often than not, they may send you home. Always defer to your GI doctor, unless what you’re experiencing is causing severe dehydration, bleeding, or pain.
The Crohn’s and Colitis Foundation says you should seek immediate medical attention if you have:
-
Heavy, persistent diarrhea
-
Bleeding from the rectum and blood clots in your stool
-
Constant pain
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
Read Also: What Can You Do For An Ulcer In Your Mouth
When Symptoms Get Severe
In some cases, UC can in some cases cause life-threatening complications including severe bleeding, perforated colon, and severe dehydration. If any of these conditions are present, its a medical emergency and the person should get immediate medical attention. UC can also cause an increased risk of colon cancer and blood clots in the veins and arteries.
When Should I Go To The Emergency Department
You should always have bleeding from the anus checked out by a doctor as it could be a sign of something serious.
Seek urgent medical attention if:
- the bleeding is very heavy
- you have signs of shock like rapid, shallow breathing, dizziness, nausea or confusion
- you have black or dark red poos
- your vomit contains blood or what looks like coffee grounds
- you faint
- you have a severe pain in your rectum
- you have heavy rectal bleeding along with bad stomach pains, a fever, weakness, nausea or you cannot have a bowel motion
Don’t Miss: Signs Of Having An Ulcer
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Read Also: Stomach Ulcer Foods To Eat
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Health Problems Affecting Other Parts Of The Body
Some people with ulcerative colitis also have inflammation in parts of the body other than the large intestine, including the
- joints, causing certain types of arthritis
- skin
- liver and bile ducts, causing conditions such as primary sclerosing cholangitis
People with ulcerative colitis also have a higher risk of blood clots in their blood vessels.
Don’t Miss: Prednisone For Ulcerative Colitis Reviews
Anxiety And Control Over Activities
Participants acknowledged a large amount of anxiety resulting from a pattern of their symptoms controlling their lives and the resulting effects of their disease on their quality of life.
Ive got a full-blown flareup, and uh, I try and schedule things around when Ive got to go to the bathroom in a half hour, so lets not start this meeting or lets get this meeting over, um, excuse me, Ive gotta go.
if I dont go in the morning, then its in the back of my head, Ok, whens it going to hit? But if I go in the morning, right after I get up, I have no worries the rest of the day.
You end up planning your whole life around what your gut is doing.
I mean, you plan your life around it .
When it started, I just had to stay home because so often I couldnt handle it and it had absolutely no control, and when you teach, you cannot have that in the classroom.
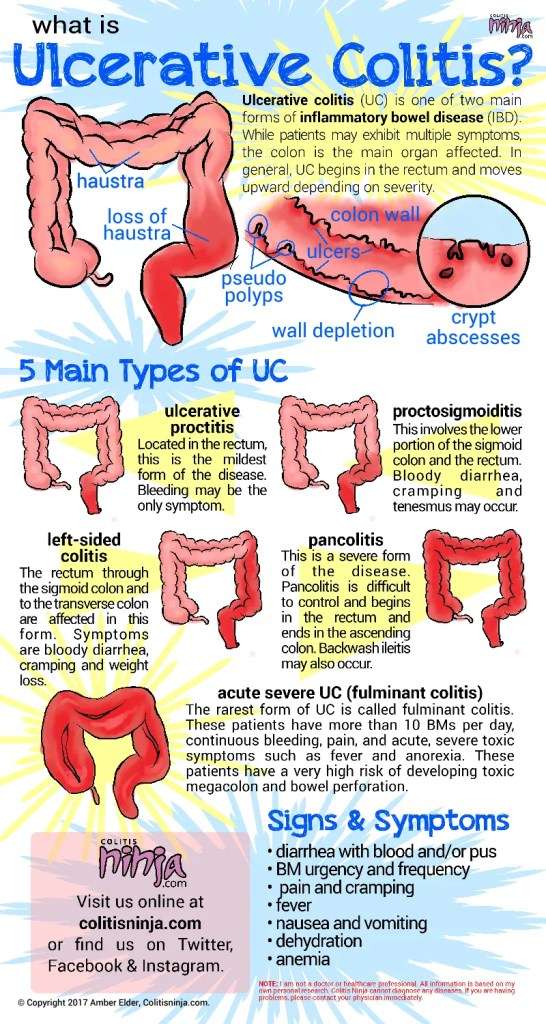
How Does Ulcerative Colitis Affect Your Stool
Changes in stools are directly related to how UC affects your colon and rectum. In UC, the immune system attacks healthy cells in the digestive tract. The attack increases white blood cells in your colon and rectum, and repeated attacks lead to chronic inflammation.
Inflammation causes your colon to contract and empty frequently, which is why you may experience frequent diarrhea and urgent bowel movements.
When inflammation destroys the cells lining your colon, sores or ulcers can develop. These ulcers can bleed and produce pus, resulting in bloody diarrhea.
Some people with UC also have constipation, but this isnt as common as diarrhea. Constipation typically occurs when inflammation is limited to the rectum. This is known as ulcerative proctitis.
Other symptoms related to ulcerative colitis include abdominal pain, painful bowel movements, fatigue, anemia, weight loss, and fever.
Read Also: Best Things To Eat With Ulcerative Colitis
The Ability To Differentiate Gas From Liquid Or Solid In The Rectum When Urgency Occurs
Participants can be greatly affected by a loss of the ability to differentiate rectal urgency due to gas from rectal urgency due to stool, mucus, or blood. They usually lose this ability during a flare, and need to go to the toilet anytime they have urgency, to avoid the risk of incontinence.
If I do have gas, I dont dare let it pass because all sorts of other stuff could come with it.
When Im having a flare, I cant tell if its gas or not. Gas can carry some other stuff with it. When theres a flareup, I think gas counts because theres no such thing as just gas.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
You May Like: How Do You Know If You Have Ulcerative Colitis
What Causes Blood In Stool
Seeing bright red blood in stool is no laughing matter, especially when its your own poop.
Sometimes it can mean something serious is going on. Other times it may be minor and nothing to lose sleep over.
Either way, bloody stool can be quite alarming, and most experts agree its not something to just ignore.
Are you wondering, Why is my poop black? Many people dont realize that black stool is also a form of bloody stool.
Its true, blood in stool can result in black poop or bright red blood in poop. The color is actually very important to note, since different colors can point toward various internal sources of bleeding.
Bloody stools can also be a symptom of bleeding from the anus or rectal bleeding.
Of course, if you are having an excessive amount of blood loss, head straight for emergency medical care. If you are not having life-threatening blood loss or other symptoms in addition to blood in stool, then there are some natural ways to help yourself.
You want to first address root causes of your bloody stools. Read on to find out some of those possible causes, as well as natural remedies to address each one.
How To Diagnose And Treat Anemia When You Have Ulcerative Colitis
Screening for anemia can be done with a simple blood test. While doctors should be routinely checking UC patients for anemia, some research suggests this doesnt always happen.
The same study from Inflammatory Bowel Diseases found that while 56 percent of people with UC develop anemia, only a little over one-third of them have had iron replacement therapy recommended.
Treatment varies depending on the severity of the deficiency. You may need to take iron supplements or vitamin B12 supplements or receive the nutrients intravenously. Some supplements may cause GI symptoms, such as abdominal cramps, so you may need to work with your doctors to try several types until you find one thats tolerable, Dr. Philpott says. In serious cases, you may need a blood transfusion.
Once iron deficiency is treated properly, energy levels can improve dramatically.
Treating the UC itself is also necessary. If we dont treat the disease, the patient is going to keep losing blood, Philpott says. Its kind of like trying to refill a pail that has a hole in it.
Though theres not much else you can do to prevent the condition if you have UC, if you think you may be anemic, speak to your doctor right away about not only testing and treatment but also getting your UC symptoms under control. Treating UC can help resolve the colon inflammation that causes bleeding and, thus, anemia, according to Dr. Friedman.
You May Like: Vsl 3 And Ulcerative Colitis
Can I Manage Or Prevent Rectal Bleeding
If you have rectal bleeding, there are a number of things you can do to help manage the condition.
If you have constipation causing haemorrhoids, you can help ease it by:
- drinking plenty of water, unless you have an existing medical condition that means this is not possible
- eating fibre-rich foods, such as bran cereals, fruit, vegetables and wholegrain bread
- avoiding processed foods, such as white bread and cheese
- keeping active and mobile to reduce the risk of getting constipated
- going to the toilet when you have the urge
If your doctor has confirmed that you have an anal fissure, you can ease the discomfort by:
- very carefully wiping the anal area after going to the toilet and using soft, moist toilet paper or baby wipes, rather than dry toilet paper
- patting the area around your bottom rather than rubbing it
- having warm baths a few times a day
- seeing your pharmacist for topical creams to reduce the pain
- making sure you eat a healthy diet with plenty of fibre, and drinking plenty of fluids to keep your stool as soft and well-formed as possible
- trying not to strain when passing a stool
Do not apply creams and lotions to the area that were not prescribed by your doctor or pharmacist because this can cause more trauma.