Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin< 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
Symptoms Of Pressure Ulcers
The parts of the body most at risk of developing pressure ulcers are those that are not covered by a large amount of body fat and are in direct contact with a supporting surface, such as a bed or a wheelchair.
For example, if you are unable to get out of bed, you are at risk of developing pressure ulcers on your:
- shoulders or shoulder blades
- knees, ankles, heels or toes
If you are a wheelchair user, you are at risk of developing pressure ulcers on:
- the back of your arms and legs
- the back of your hip bone
Treatment For Pressure Sores
There are a variety of treatments available to manage pressure sores and promote healing, depending on the severity of the pressure sore. These include:
- regular position changes
- special mattresses and beds that reduce pressure
- being aware of the importance of maintaining healthy diet and nutrition
- dressings to keep the sore moist and the surrounding skin dry. There is no advantage of one type of dressing over another.
- saline gauze dressing may be used if ointments or other dressings are unavailable.
- light packing of any empty skin spaces with dressings to help prevent infection
- regular cleaning with appropriate solutions, depending on the stage of the sore
- there is no advantage of one particular type of antiseptic or antibiotic treatment over another
- specific drugs and chemicals applied to the area, if an infection persists
- surgery to remove the damaged tissue that involves thorough debridement of the wound, the removal of underlying or exposed bone, and filling the empty space
- operations to close the wound, using skin grafts if necessary
- continuing supportive lifestyle habits such as eating a healthy and nutritious diet, as suggested by the nutritional staff.
You May Like: Ulcerative Colitis And Blood In Urine
Skin Breakdown And Decubitus Ulcers
Pressure ulcer formation is a serious health problem in debilitated and immobilized patients. After a stroke, patients are at particular risk for pressure ulcers because they have numerous factors contributing to skin breakdown. Abnormal sensation, contracture, malnutrition, immobility, and muscle and soft-tissue atrophy often develop and may be complicated by advanced age. Prevention of pressure ulcers, rather than treatment of developing ulcers, should be the focus of care. Preventive measures include frequent repositioning keeping skin clean and dry maintaining an adequate level of nutrition and, especially in high-risk patients, using pressure-relief mattresses.132 After pressure ulcers have formed, in addition to strictly observing the preventive and pressure relieving measures previously noted, treatments include meticulous wound care with a variety of agents and possibly surgical reconstruction.
Lawrence C. Vogel, … M.J. Mulcahey, in, 2012
What Complications Might Come With Pressure Ulcers
Pressure ulcers can be painful and become infected, and infection may spread from the skin , to blood , muscle or bone. Treatment may require antibiotics, usually at home but sometimes in hospital. In very rare cases, chronic pressure ulcers can cause skin cancer. It’s important to recognise pressure ulcers early and to act quickly to prevent complications.
Also Check: Best Things To Eat With Ulcerative Colitis
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
How Are Bedsores Treated
Specific treatment of a bedsore is discussed with you by your healthcare provider and wound care team and based on the severity of the condition. Treatment may be more difficult once the skin is broken, and may include the following:
- Removing pressure on the affected area
- Protecting the wound with medicated gauze or other special dressings
- Keeping the wound clean
- Removing the damaged, infected, or dead tissue
- Transplanting healthy skin to the wound area
- Negative pressure wound therapy
Healthcare professionals will watch the bedsore closely. They will document size, depth, and response to treatment
Also Check: What Does A Stomach Ulcer Feel Like Symptoms
Other Tips For Preventing Pressure Ulcer
1. Check the skin daily for any signs or symptoms of pressure ulcers. The patients can take the help of Bedside Wound Care Services for this. 2. Maintain a healthy and balanced diet that contains sufficient and enough protein with good sources of vitamins and minerals.3. Quit smoking. People who smoke are more prone to develop pressure ulcers due to the damage caused to blood circulation. 4. For repositioning, wheelchair push-ups are good where the person can raise their body off the seat by pushing on the arms of the chair. The use of cushions or special mattresses is also prescribed to release pressure and ensure a well-positioned body. Avoid doughnut cushions as they can put pressure on surrounding tissues.5. Ensure regular pressure ulcer dressings to avoid any type of infection and effective wound healing.
How Can I Tell If I Have A Pressure Sore
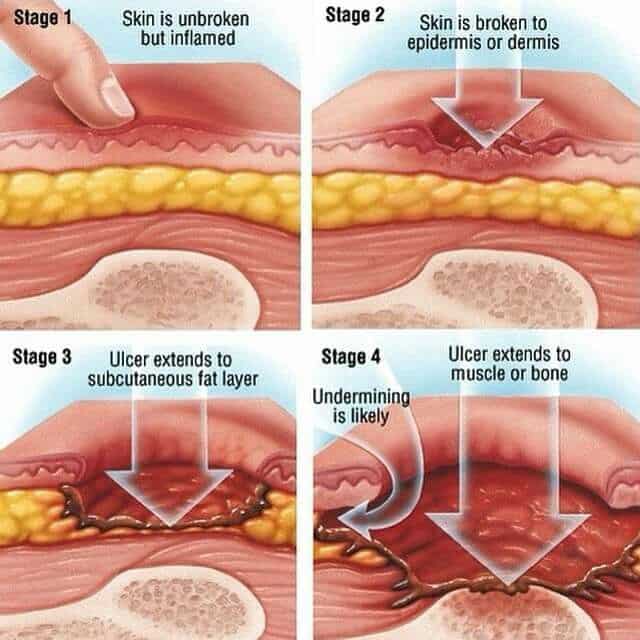
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
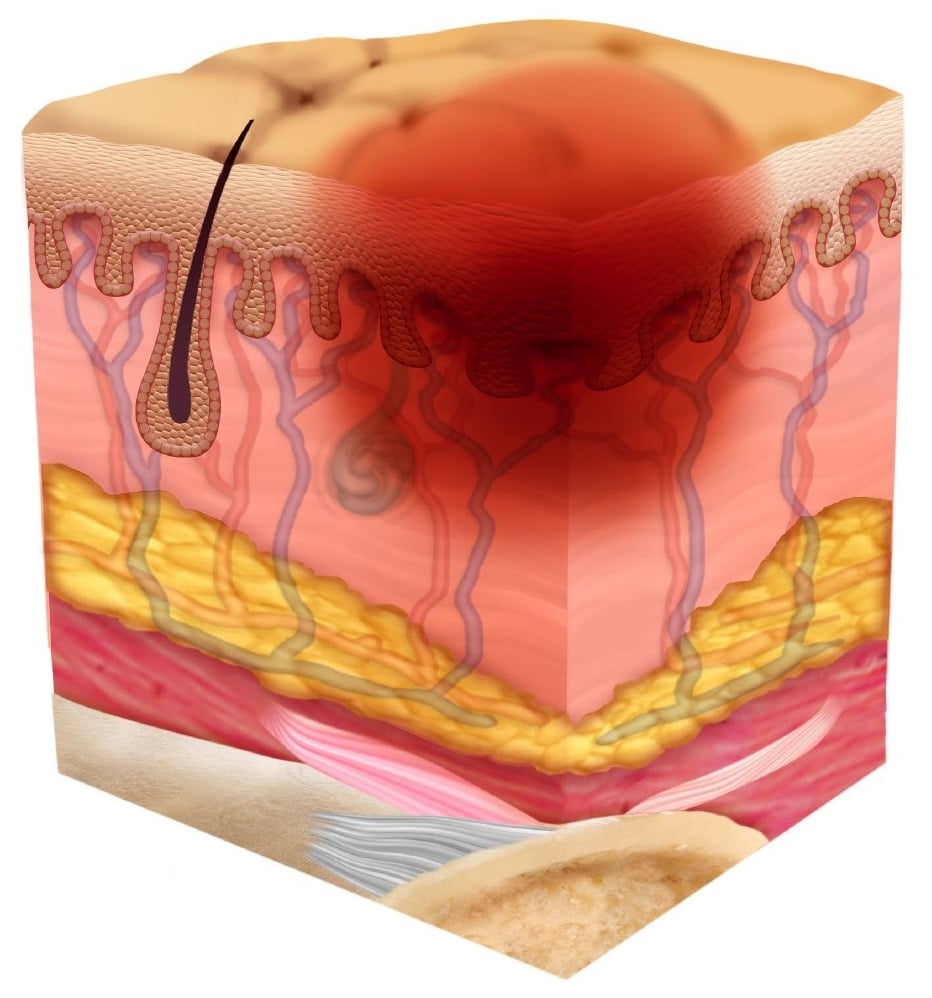
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
Related Factsheets
Healing time:
You May Like: Can I Eat Eggs With Ulcerative Colitis
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
- Use positioning devices to prevent prolonged pressure bony prominences.
- Keep the head of the bed as low as possible to reduce risk of shearing.
- Keep sheets dry and wrinkle free.
Family And Individual Level
Healthcare professionals can have an impact on an individual level by:
- recognising the important role individuals, families and carers have in preventing and managing pressure ulcers
- engaging individuals, carers and families in what to look for and how pressure ulcers can be prevented
- using appropriate literature with visual images to explain how quickly pressure ulcers can develop
- educating the individuals and caregivers about the causes, assessment and management of pressure ulcers
- using appropriate terminology recognising and informing patients that pressure ulcers are another term for bed sores
- encouraging individuals to move independently whenever possible
- directing individuals to appropriate healthcare professionals if they suspect a pressure ulcer is forming or is present
- looking out for skin discolouration or soreness, particularly in areas where bones are close to the skin
- repositioning or turning patients frequently at least every 2 hours for those patients who need help
- using moving and handling aids to help reposition individuals who require assistance moving
- performing regular skin inspections to check areas at risk and document pressure areas at least once a day
- checking that patients with pressure ulcer risk factors are registered with a GP and receive primary health care support to minimise the risks
- providing holistic health assessments for people at risk of developing pressure ulcers
Don’t Miss: How To Treat Duodenal Ulcer
Who’s Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 older people are more likely to have mobility problems and skin that’s more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body
- medical conditions that affect blood supply, make skin more fragile or cause movement problems such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis and Parkinson’s disease
When To Get Medical Advice
If you’re in hospital or a care home, tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer. It’ll probably continue to get worse if nothing is done about it.
You should be regularly monitored and offered advice and treatment to reduce the risk of pressure ulcers, but sometimes they can develop even with the highest standards of care.
If you’re recovering from illness or surgery at home, or you’re caring for someone confined to bed or who is a wheelchair user, contact your GP surgery if you think you or the person you’re caring for might have a pressure ulcer.
Get medical advice immediately if there is:
- red, swollen skin
- pus coming from the pressure ulcer or wound
- cold skin and a fast heartbeat
- severe or worsening pain
- a high temperature
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
Don’t Miss: Things To Eat With An Ulcer
How Can Pressure Ulcers Be Treated
It is important to watch out for early signs of pressure ulcers and to contact your doctor if you notice any changes to the skin. Ulcers are best managed early on, and your doctor will assess whether your pressure ulcer can be managed at home, if you need a referral to a wound specialist or if you require treatment at hospital.
Use healthdirects Service Finder tool to locate your nearest GP or nurse clinic.
Wound dressings can enhance healing. Your healthcare team will select the most appropriate treatment and dressing, depending on your specific pressure ulcer. There are 6 classes of dressings:
- alginate absorbent fibre dressings
Depending on the type of pressure ulcer, a bandage may also be applied to keep the dressing in place or support the injured area.
To promote healing and recovery, it is important to eat a balanced diet that includes protein, carbohydrates, fats and sufficient fluids.
Other treatments may include antibiotics if the ulcer becomes infected, or debridement a procedure used to clean the wound and remove any damaged tissue.
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
You May Like: Artificial Sweeteners And Ulcerative Colitis
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
Enhancing Healthcare Team Outcomes
The main goal is to prevent a decubitus ulcer by decreasing the pressure acting on the affected site. This goal requires an interprofessional team, including primary care providers, wound care specialists, surgeons, specialty-trained wound nurses, physical therapists, and nurses aides. Nurses provide care, monitor patients, and notify the team of issues. Nurses aides are often responsible for turning and repositioning patients. Air-fluidized or foam mattresses should be used, frequent postural changes, provision of adequate nutrition, and treatment of any underlying systemic illnesses. Debridement should take place to remove dead tissue that serves as the optimum medium for the growth of bacteria. Hydrogels or hydrocolloid dressing should be used, which aid in wound healing. Tissue cultures are necessary, so the most directed antibiotic can be administered, which can involve the pharmacist and the latest antibiogram data. The patient should be kept pain-free by giving analgesics. They should try to increase physical activity if possible, which a nurse’s aide, medical assistant, or rehab nurse can facilitate. Frequent follow-ups are an absolute necessity and a team approach to patient education and management involving the wound care nurse and wound care clinician will lead to the best results. These interprofessional activities can help drive better outcomes for patients with decubitus ulcers.
Read Also: H Pylori And Stomach Ulcers
Causes Of Pressure Sores
Pressure sores happen if you cant move around and so stay in one position for a long time. We normally move about constantly, even in our sleep. This stops pressure sores developing.
People who are unable to move around tend to put pressure on the same areas of the body for a long time. If you are ill, bedridden or in a wheelchair, you are at risk of getting pressure sores.
A number of things can increase your risk of pressure sores, including:
- being unable to move around easily due to old age or illness
- weight loss – you may have less padding over bony areas
- sliding down in a bed or chair – pressure on the skin cuts off blood supply because the skin is being pulled in different directions
- friction or rubbing of the skin, for example against sheets
- moist skin – for example, due to sweating or incontinence
- other medical conditions, such as diabetes
- having a previous pressure ulcer
Treating And Preventing Pressure Ulcers
Treatment for pressure ulcers includes the use of dressings, creams and gels designed to speed up the healing process and relieve pressure. Surgery is sometimes recommended for the most serious cases.
For some people, pressure ulcers are an inconvenience that require minor nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning or gangrene.
Read more about the complications of pressure ulcers.
Pressure ulcers can be unpleasant, upsetting and challenging to treat. Therefore, a range of techniques is used to prevent them developing in the first place. These include:
- regularly changing a person’s position
- using equipment to protect vulnerable parts of the body such as specially designed mattresses and cushions
Read about treating pressure ulcers and preventing pressure ulcers for more information.
Unfortunately, even with the highest standards of care, it’s not always possible to prevent pressure ulcers in particularly vulnerable people.
Read Also: Ulcerative Colitis And Anxiety Attacks
What Increases The Risk Of Developing Pressure Ulcers
People who are confined to a bed or chair for example due to stroke, spinal injury or dementia are at greater risk of developing extensive pressure ulcers. Other risk factors include:
- immobility being confined to bed after an illness or surgery, or due to paralysis
- diabetes and other health conditions that can affect blood supply