How Patients Become Anemic
As with Emily, the most common reason UC patients develop anemia is because of bleeding, Dr. Hou says. This bleeding is ultimately caused by inflammation in the colon, when the body’s immune system “overreacts” to a trigger, perhaps one in the environment or a food additive. Inflammation causes ulcers to form, and they, in turn, may bleed.
Another way patients may become anemic is because when they feel sick, they limit what they’re eating, which can reduce iron intake, Dr. Hou says. Finally, in what he terms a “third strike,” even though a UC patient is eating well, they may not absorb iron sufficiently because of inflammation in their colon and throughout their entire body.
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with Crohns disease and ulcerative colitis and their loved ones. More than 140,000 members come together to ask questions, give advice, and share their stories with others who understand life with Crohns and colitis.
Do you have anemia with IBD? More than 5,900 members report having anemia, and more than 17,000 report blood in the stool or rectal bleeding as symptoms. Share your experience in the comments below or start a conversation by posting on MyCrohnsAndColitisTeam.
A Pathway To Better Health
Echoing an opinion shared by the Crohn’s & Colitis Foundation, and as a member of its Houston Leadership Board, Dr. Hou agrees that more could be done to identify and manage anemia in the IBD patient population. The foundation even developed what’s called the IBD Anemia Care Pathway, which includes current guidelines for clinical management. Dr. Hou calls this a “practical approach that’s not too complicated.”
He and others who treat IBD understand that a patient having a flare that already involves pain and nausea doesn’t want to take iron pills that may cause more pain and nausea.
“If a patient is inflamed and anemic, we don’t want to waste time with oral iron that they may be unlikely to absorb and may not tolerate well,” he says. “We can make them more comfortable with IV iron in a couple of quick doses and without long, drawn-out side effects.”
Also Check: Ulcer Pain Relief At Night
Red Blood Cell Size Factor
Red blood cell size factor is the result of the square root of the product of Mean corpuscular volume multiplied by the Mean Reticulocyte Volume and seems to be a suitable parameter for the study of bone marrow erythropoietic activity, as it provides a very good level of agreement with reticulocyte hemoglobin content . There is evidence of a significant correlation between RSF and CHr with excellent diagnostic performance of RSF compared with CHr in diagnosing of the type of anemia. A significant correlation between RSF and reticulocyte hemoglobin equivalent in the diagnosis of inefficient erythropoiesis has also been observed.
RSF was found significantly positively correlated with Tsat and negatively with sTfR in a recent study of 100 patients with IBD. RSF was significantly lower in patients with IDA compared with patients with other causes of anemia and patients without anemia. Low RSF was among the best markers for diagnosis of ID with a sensitivity of 83% and a specificity of 82%. On the contrary, concerning disease activity, RSF was not significantly different between active and non-active disease and no significant correlation between RSF and CRP levels was found. Based on these data RSF seems to be a sensitive real time parameter for the early detection of the impaired erythropoietic mechanisms in IBD patients.
Rice Water To Fight Ulcerative Colitis
One cup of rice water as soon as you wake up and another before bed will help control ulcerative colitis and its symptoms.
Ingredients
Preparing this drink is very simple.
Dont Miss: Difference Between Ulcerative Colitis And Crohns Disease Ppt
Also Check: Is Sweet Potato Good For Ulcerative Colitis
Other Causes Of Inflammation That May Lead To Anemia
While anemia of inflammation typically develops slowly, anemia of critical illness is a type of anemia of inflammation that develops quickly in patients who are hospitalized for severe acute infections, trauma, or other conditions that cause inflammation.
In some cases, older adults develop anemia of inflammation that is not related to an underlying infection or chronic disease. Experts think that the aging process may cause inflammation and anemia.
Ways To Manage Symptoms And Flares Of Ulcerative Colitis
A flare of ulcerative colitis can be painful and embarrassing not only for you, but for those around you. Once you have one flare, are you going to have more? That anxiety can make you feel even worse and trigger one. Lets investigate 6 ways to manage symptoms and flares of ulcerative colitis.
Read Also: Skin Graft Diabetic Foot Ulcer
It’s Important To Treat Uc Symptoms
At the core, the disease needs treatment to prevent blood loss. If you think you might be anemic, my best advice is to speak to a doctor right away. You may not only need to get UC or Crohn’s symptoms under control, but you might also need to increase iron levels. Soothing the inflammation will resolve anemia.
Over the years of living with UC, I’ve had to learn that tending to the garden of my body is of utmost priority. I cannot take care of others if I don’t first take care of myself. Now, older and wiser, I understand my body better. That if left untreated, anemia causes the heart to pump harder to distribute oxygen.
Who wants their heart to work harder? This gardener now understands that tending to my gut is also tending to all other aspects of my body.
So, be good to yourself. Your heart will thank you.
Iron Deficiency An Accomplice In Other Ibd Sequelae
Iron is a vital element involved in gas exchange, mitochondrial function, DNA repair, free radical production in immunity, and a host of other cellular functions . Chronic IDA also means chronic hypoxia, which in combination could elicit a maladaptive response in the context of chronic inflammation.
Iron deficiency is known to be associated with thrombocytosis, which is perhaps an evolutionary response to compensate for blood loss . Thrombocytosis is also a feature of IBD, occurring in response to inflammation. However, iron therapy in patients with IBD reduces platelet number as well as platelet activity, indicating that iron deficiency itself is a contributor .
In cancer patients, where thrombotic events are a significant cause of morbidity and mortality, high platelet counts are a risk factor for venous thromboembolism . Likewise, IBD patients are at considerable risk for thrombotic events, and risk increases when disease activity is highest . Anaemia also correlates with disease activity, so both IDA and inflammation may be playing contributory roles in the pathogenesis of thrombotic events in IBD.
In our research, we have discovered that IDA alone can increase both arterial and venous thrombotic tendency in animal models. Animal models of IBD are more susceptible to thrombosis, and haematologic examination of these models also show significant anaemia . The increased thrombotic tendency in IBD may be the combined effect of both inflammation and iron deficiency.
You May Like: Best Dressing For Pressure Ulcers
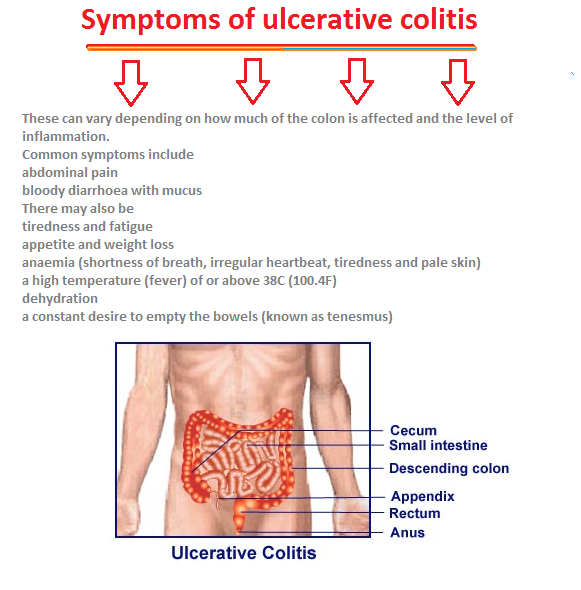
Diarrhea And Rectal Bleeding
People with ulcerative colitis often experience watery diarrhea as well as frequent and sudden urges to have a bowel movement. For some people, the urge to have a bowel movement may occur so suddenly that it significantly disrupts their daily life. Some people need to have a bowel movement more than 10 times per day.
You may notice blood, pus, or mucus in your stools. You may also experience rectal bleeding if youre having a flare-up. Blood comes from ulcers along the surface of your rectum.
If you have uncontrollable diarrhea or notice blood in your stool, you should see a doctor. Diarrhea caused by ulcerative colitis can lead to medical emergencies like severe dehydration, a perforated colon, or .
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
You May Like: Ulcerative Colitis Left Side Pain
What Pain Relief Medicines Are Used In Inflammatory Bowel Disease
There are a variety of pain relief medicines available which can help to control pain in Crohns disease and ulcerative colitis.
Paracetamol
Paracetamol is a commonly used over-the-counter painkiller you can buy without a prescription. It can be used to help with mild to moderate pain, and can also help to control a high temperature. Paracetamol can be used by adults and children and is available in a variety of forms, including:
- Tablets, capsules and caplets
- Oral suspension
Paracetamol works by blocking the production of chemicals in your body called prostaglandins, making your body less aware of any pain. It also reduces your temperature by acting on the part of your brain responsible for controlling it.
Paracetamol is often combined with other medicines, including other types of painkillers. Always check any additional medicines are also safe for you to use.
It is generally considered safe to take paracetamol if you have inflammatory bowel disease, however if you need to take paracetamol for longer than three days, or have a new pain, you should speak to your IBD team.
Two paracetamol tablets every four hours, up to four times a day is considered a safe dose for adults. Side effects are uncommon with paracetamol.
You should read the patient information leaflet in your medicine packet to check if paracetamol is suitable for you. Do not take more than the maximum dose in a 24 hour period as an overdose of paracetamol can be very dangerous.
How To Pin A Boutonniere On A Vest

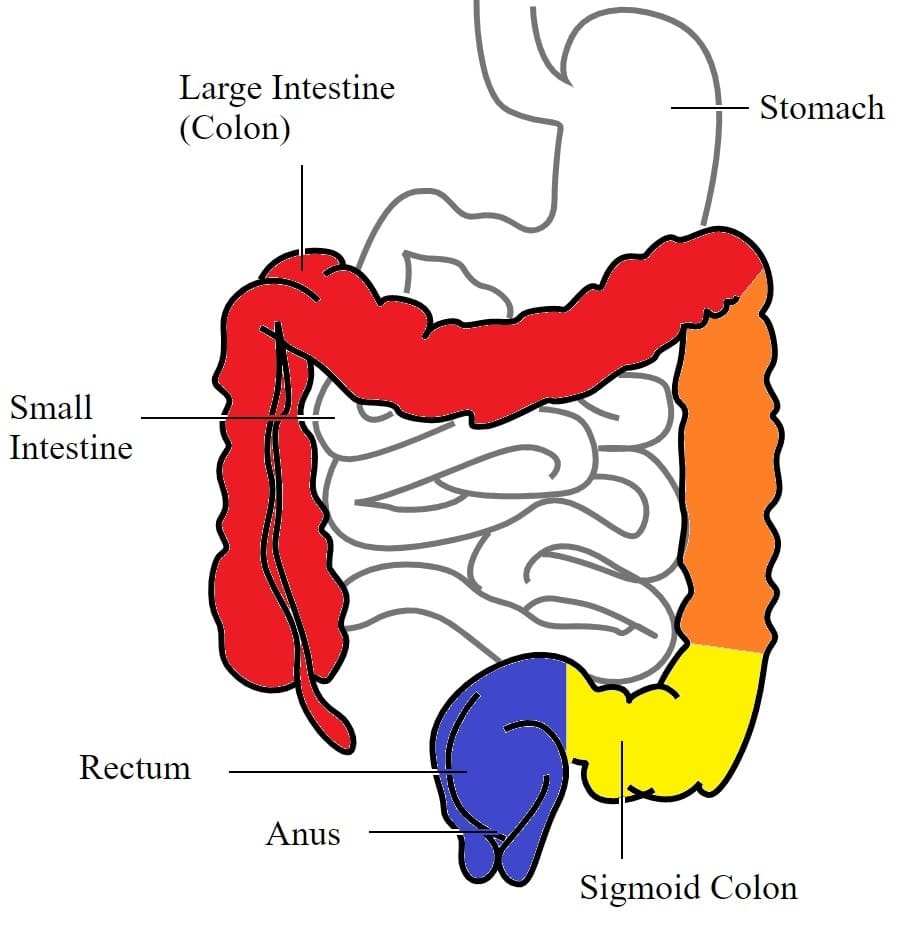
disease are Crohns disease and ulcerative colitis. Ulcerative colitis typically appears in the linings of the large intestine. It causes swelling and ulcers to form in affected regions. In extreme cases, this can cause a whole to appear in the tracks of the large intestines. In these cases, immediate emergency surgery is required.
Ulcerative colitis is a type of inflammatory bowel disease that causes inflammation in the large intestine. Here, find out what it involves and how to treat it. … Long COVID‘s cardiovascular implications Tools. General Health. Drugs A-Z Health Hubs Health Tools. BMI Calculators and Charts .
Ulcerative Colitis. Ulcerative colitis is a disease that causes inflammation and sores, called ulcers, in the lining of the rectum and colon. It is one of a group of diseases called inflammatory bowel disease. UC can happen at any age, but it usually starts between the ages of 15 and 30. It tends to run in families.
Microscopic colitis is a type of inflammatory bowel disease, a chronic condition of inflammation in your colon. It causes frequent, watery diarrhea and other gastrointestinal symptoms. Diet and medication can help manage flare-ups when they occur. Appointments 216.444.7000. Appointments & Locations.
Albert Williamson-Taylor, 63, has suffered ulcerative colitis for the past 30 years. All previous treatments have failed or had limited impact on his painful condition. Experts say the drug.
Read Also: Holistic Treatment For Ulcerative Colitis
Why Are People With Ibd At Risk
People who have inflammatory bowel disease are at risk for anemia. One reason for this is the poor absorption of vitamins and minerals that can occur because of inflammation or diarrhea. If the intestines can’t absorb enough iron, folate, vitamin B12, and other nutrients, the body won’t have what it needs to create more red blood cells.
Another reason for anemia in people who have IBD is the blood loss that can occur with Crohn’s disease and ulcerative colitis. A continual loss of blood, especially in amounts that can’t be easily replenished by the body, can result in anemia.
The good news is that many cases of anemia can be treated effectively. When IBD is gotten into remission and the bleeding lessens, that will help with anemia significantly. Iron supplements or even iron infusions may also be used to treat anemia in some cases.
What To Eat During A Flare
All of the diets above are intended to be temporary and followed during a flare-up. Working with a dietitian can help prevent deficiencies in certain micronutrients, which is common with IBD.
During a flare its helpful to eat four to six small meals per day rather than fewer larger meals. Its also very important to drink fluids because diarrhea can occur with a flare and cause dehydration.
Read Also: Best Natural Remedies For Stomach Ulcers
Crohns Disease And Anemia
Crohns disease can cause inflammation anywhere in the digestive tract. Most nutrient absorption happens in the small intestine. Active Crohns disease in the small intestine affects the bodys nutrient absorption sites.
The small intestine includes three parts: the duodenum, jejunum, and ileum. Most iron gets absorbed in the duodenum. Some iron is also absorbed in the jejunum and ileum.
If these areas are inflamed, iron cant be absorbed normally. This can lead to anemia. About 70 percent of people with Crohns disease require surgery to remove affected areas in the digestive tract. Surgery can put the disease into remission to reduce future blood loss.
Active disease comes back within 5 years in 33 percent of people who have surgery for Crohns disease. This can cause anemia if iron levels drop again.
Percentage Of Hypochromic Red Cells
Percentage of hypochromic red cells is defined as cells with intracellular hemoglobin of < 28 g/dl. In the healthy population, the percentage of hypochromic red cells does not exceed 2.5% and values greater than this are indicative of iron deficient erythropoiesis. Percentage of hypochromic red cells is the concentration of hemoglobin in individual cells rather than the mean, as happens with mean cell hemoglobin or mean cell hemoglobin concentration . It is a more sensitive marker because small changes in the number of red cells with inadequate hemoglobin can be measured before there is any change in the MCHC. Some sophisticated instruments can report this parameter but it has been argued that, as mature red cells have a longer lifespan, the percentage of hypochromic red cells integrates information from over too long a period and may be less sensitive than reticulocyte hemoglobin in diagnosing functional IDA or monitoring anemia treatment. Some studies report that the percentage of hypochromic red cells is sensitive enough for the measurement of functional IDA. Additionally, the utility of the test is limited as the percentage of hypochromic red blood cells is dependent on the total number of red blood cells, which may vary with the length of storage time. Currently, there are no studies investigating the role of this parameter in IBD.
Also Check: Budesonide Vs Prednisone For Ulcerative Colitis
Anaemia Due To Treatment
Apart from folate deficiency, therapy with sulphasalazine or 5-aminosalicylic acid has been related to a minor degree of haemolysis or aplasia. More importantly, both 6-mercaptopurine and azathioprine have a direct myelosuppressive effect. The risk of developing leucopenia or aplasia is high in individuals with low thiopurine methyltransferase activity. The enzyme activity of TPMT is genetically determined and genotyping has been suggested as a means of detecting patients at risk. In clinical practice, however, concerns have been raised about the predictive accuracy of this test.
There are many other less common causes of anaemia in IBD which are best dealt with by those who see them more frequently, such as the local haematologist .
Aetiology of inflammatory bowel disease associated anaemia
Limit Intake Of Animal Products
Especially meats/red meats. I have read in many articles that because many people have low stomach acidity and poor digestion, meats tend to rot in our guts, thus producing pus and contributing to inflammation . This rotting can produce more intestinal gas and overall slower digestion. I personally try to limit my meat intake to 1-2 meals per week !
You May Like: Best Mattress For Pressure Ulcers
Iron Loss In Inflammatory Bowel Disease
Iron deficiency anaemia can be considered a gastroenterological condition. The leading causes of iron deficiency in the developed world are menstruation and blood loss associated with gastrointestinal disease. In the latter case, blood loss in the stomach or intestine cannot be matched by duodenal iron absorption, creating a negative iron balance. This imbalance is often seen in IBD, leading to anaemia. While our understanding of IBD has grown over the past decades, the prevalence of IBD associated anaemia has changed only little: one third of IBD patients still have haemoglobin levels below 12 g/dl.
Anaemia is a consistent clinical feature of IBD
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Don’t Miss: Causes Of Ulcers In Horses