How The Intervention Might Work
Findings from research based on animal models suggest that acute wounds heal more quickly if the wound surface is kept moist in order to prevent the formation of a hard scab or eschar. A moist environment is also thought to provide optimal conditions for promoting autolytic debridement, which is sometimes considered to be an important part of the healing pathway . It has been suggested that alginate dressings may control bleeding, manage exudate, promote autolytic debridement, provide a moist wound healing environment and promote healing .
Signs And Causes Of Venous Ulcers
Venous ulcers are non-healing or slow-healing wounds that form as a result of blood pooling in the legs and feet. This happens when the walls or valves in the veins of the lower extremities dont work effectively. This is called venous insufficiency.
Venous ulcers are more common in women and older people. Several factors increase your risk of developing venous ulcers, including:
- Long periods of immobility, such as bed rest
Dressings For Venous Leg Ulcers
You May Like: List Of Foods To Avoid With Ulcerative Colitis
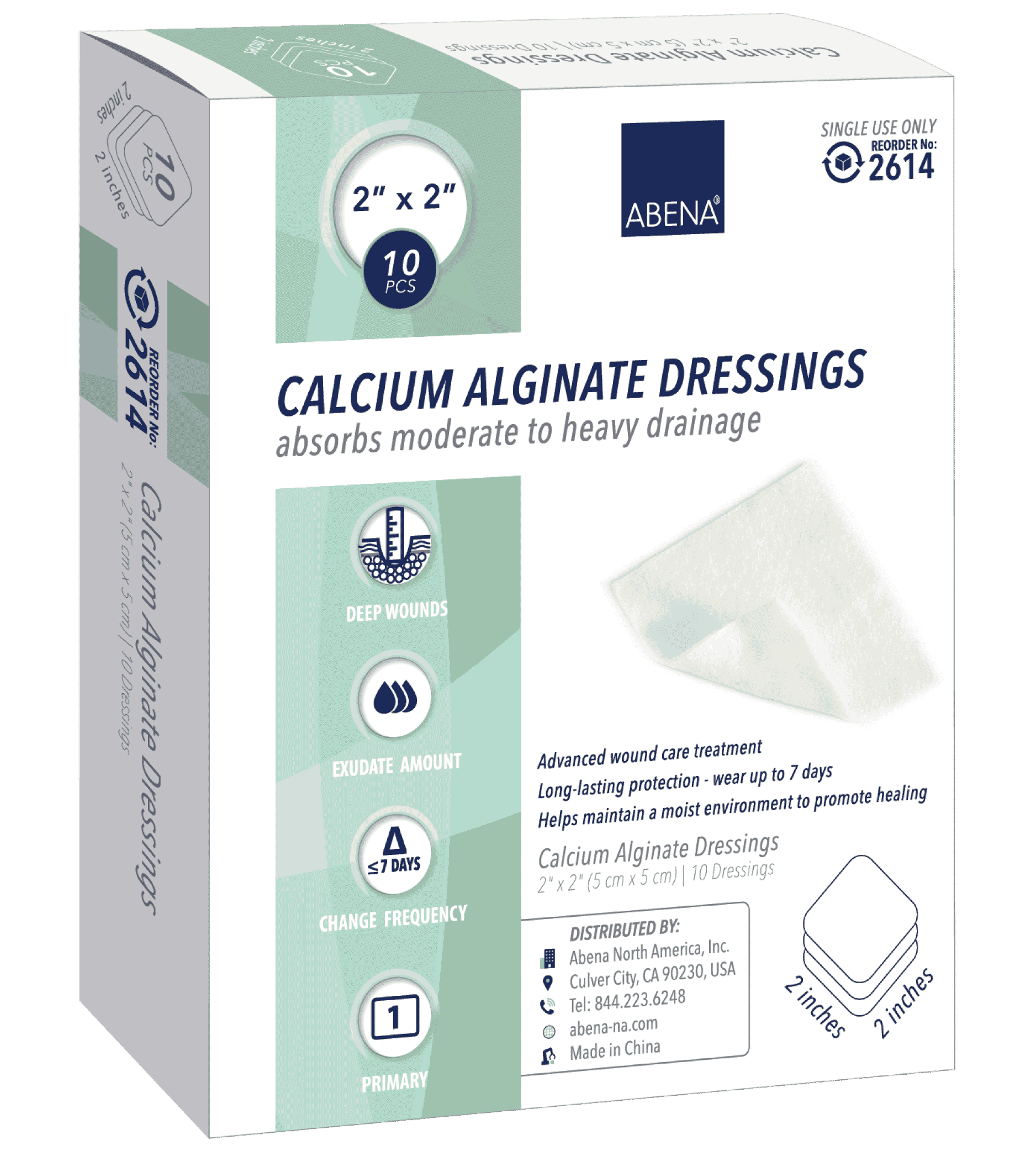
When To Use Calcium Alginate Dressing
These Calcium alginate wound dressing is versatile in nature and has numerous applications. They work best on wet wounds, which produce a lot of exudate and sloughy wounds that have dead tissues. These dressings are effective on:
- Diabetic wounds
- Refractory decubiti
They have hemostatic properties for which they are used on bleeding wounds.These wound dressings should not be applied on heavily necrotic and dry wounds. This wound dressing requires exudate to form a gel-like covering and initiate healing. If the wound is dry, the dressing will stick to it and can be painful while being removed.
Can Leg Ulcers Be Prevented

To prevent and promote healing of ulcers:
- Avoid injury, particularly when pushing a supermarket trolley. Consider protective shin splints.
- Walk and exercise for at least an hour a day to keep the calf muscle pump working properly.
- Lose weight if you are overweight.
- Check your feet and legs regularly. Look for cracks, sores or changes in colour. Moisturise after bathing.
- Wear comfortable well-fitting shoes and socks. Avoid socks with a tight garter or cuff. Check the inside of shoes for small stones or rough patches before you put them on.
- If you have to stand for more than a few minutes, try to vary your stance as much as possible.
- When sitting, wriggle your toes, move your feet up and down and take frequent walks.
- Avoid sitting with your legs crossed. Put your feet up on a padded stool to reduce swelling.
- Avoid extremes of temperature such as hot baths or sitting close to a heater. Keep cold feet warm with socks and slippers.
- Consult a chiropodist or podiatrist to remove a callus or hard skin.
- Wear at least Grade 2 support stockings if your doctor has advised these. This is particularly important for the post-thrombotic syndrome, leg swelling or discomfort, and for long-distance flights.
- Have a vascular ultrasound assessment and consult a vascular surgeon to determine whether any vein treatment should be carried out.
- Horse chestnut extract appears to be of benefit for at least some patients with venous disease.
Read Also: What Is Good For Mouth Ulcers
Symptoms Of Venous Insufficiency Ulcers
Whe a venous ulcer begins to develop, stasis dermatitis may be present causing scaling and erythema of the lower extremities. Hemosiderin staining may also occur, causing the presence of brownish or yellow patches underneath the skin. Other skin changes may include the appearance of dark red or purple as a result of blood leaching into the surrounding tissue. Venous ulcers will present with shallow but large wounds with irregular margins that typically develop on the lower leg or ankle. The base of the ulcer is typically red, can result in a significant amount of exudate depending on the level of infection, and will ooze venous blood when manipulated. Typically the wound will be relatively painless, with any pain resulting from subsequent infection or edema. Often the entire leg will become swollen, and the skin will become more firm and reddish brown in color, otherwise known as stasis dermatitis. Elevation of the limb will help to relieve discomfort and swelling.
Figure 1: Venous ulcer with obesity as cofactorFigure 2: Large superficial venous ulcer
Description Of The Intervention
Compression therapy is now considered to be the cornerstone of venous leg ulcer management . Primary wound contact dressings are usually applied underneath compression devices. A range of other interventions may be used concurrently with compression, including debriding agents , vasoactive drugs , fibrinolytic therapy , physical therapies , and topical applications .
Primary wound contact dressings are applied beneath compression devices with the aim of aiding healing, providing comfort, controlling exudate and helping to prevent bandages and stockings from adhering to the wound bed. The ideal conditions required for wound healing in terms of dressing application are proposed as follows: maintenance of a moist wound environment without risk of maceration avoidance of toxic chemicals, particles or fibres in the dressing fabric minimisation of number of dressing changes and maintenance of an optimum pH level .
Several types of wound dressing are available and costs vary . For example, there can be a sixfold difference in the UK unit price of a 9.5 cm x 9.5 cm nonadherent dressing compared with a 10 cm x 10 cm calcium alginate dressing .
Examples of alginate dressings currently available in the UK include Algosteril® and Tegaderm® Alginate . Appendix 2 provides a description of all wound dressings categorised by the British National Formulary .
Read Also: Can You Develop Ulcerative Colitis
The Role Of The Pharmacist In Educating Patients About Vsus
Since pharmacists are often perceived as one of the most accessible healthcare professionals, they have a critical role in the treatment and care of patients at risk of, or with, VSUs. This includes effective patient counseling and education, especially with regard to therapy for VSUs, proper use of medications used to treat VSUs, and reminders about preventive measures to decrease reoccurrence of VSUs. Since the incidence of VSUs is common in elderly and diabetic patient populations, pharmacists play a key role in identifying those patients at greater risk of developing VSUs. Pharmacists should also seize every possible opportunity to remind patients about the critical importance of adhering to therapy to enhance therapeutic outcomes and prevent further complications.
Pharmacists can also reinforce patient education with regard to the preventive measures for VSUs such as staying vigilant about oneâs overall health and adhering to the goals of therapy. Patients should be reminded of the importance of routine wound care and follow-up with their primary healthcare provider, monitoring the ulcer for signs of infection, and immediately seeking medical attention if the wound shows signs of worsening or not healing. Patients at risk for VSUs should be aware that with early diagnosis and implementation of and adherence to therapy, the condition can be effectively treated and healed to avoid complications.
What Does Clinical Experience Tell Us
Our experience with the use of calcium alginate fibres in our clinics suggests that their interest is not limited to the indications traditionally given in the literature.
We use this dressing in any situation where we want to simulate a physiological scab to promote healing. More than one will be surprised by this statement, because many of you will have in mind the axiom: scabs must always be removed. Undoubtedly, the scab must be removed if either there is underlying pus when pressing or attempting to move the scab, or the crust is too thick and makes pressure on the wound bed or is easily detached. But wouldn´t acute wounds close with the formation of a scab that ends up coming off on its own, and if we remove it early healing may be delayed? Dont forget that scabs are deposits of dry exudate and cellular debris that, in the absence of infection, behave like a protective layer that maintains optimal micro environmental conditions for healing.
Now we are going to talk about two applications in which daily clinical observation indicates that calcium alginate fibres are interesting:
If we use portable negative pressure therapy devices to promote graft attachment in complicated locations or situations , we also tend to cover the grafted lesion with alginate sheets before placing the device.
Recommended Reading: Is Ulcerative Colitis Considered An Autoimmune Disease
Venous Leg Ulcers: 6 Things To Know When Treating Venous Disease
Lower extremity venous disease affects millions of Americans and may ultimately lead to open, draining wounds that adversely affect quality of life. However, there are exciting developments in early diagnosis, prevention and treatment of venous leg ulcers . On the treatment side, there are more choices now than ever before in compression products, which is greatly improving the patient experience. But proper treatment also comes from a better understanding of venous leg ulcers, and better understanding comes from more education. Luckily, were here to help provide education and support for you and your team, so here are six things to know when treating VLUs.
You May Like: Can Ulcers In The Colon Be Cancerous
Avoid Sitting Or Standing For Long Hours
Being stationary for long hours leads to pooling of blood in the legs and development of venous leg ulcers.
Walking or moving the legs at regular intervals improves blood circulation and aids in pushing the blood in the veins up to the heart. Even moving the legs slightly helps in the circulation of blood.
Also Check: Icd 10 Unstageable Pressure Ulcer
How Are Leg Ulcers Treated
At Cleveland Clinic, patients are treated by a team of world-class experts in the Lower Extremity Wound Clinic in the Department of Vascular Medicine. This Clinic includes doctors, nurses and other medical specialists.
These experts work together to determine the cause of the ulcer and develop an individualized treatment program.
The goals of treatment are to relieve pain, speed recovery and heal the wound. Each patients treatment plan is individualized, based on the patients health, medical condition and ability to care for the wound.
Treatment options for all ulcers may include:
- Antibiotics, if an infection is present
- Anti-platelet or anti-clotting medications to prevent a blood clot
- Topical wound care therapies
- Prosthetics or orthotics, available to restore or enhance normal lifestyle function
Venous Ulcer Treatment
Venous ulcers are treated with compression of the leg to minimize edema or swelling. Compression treatments include wearing compression stockings, multi-layer compression wraps, or wrapping an ACE bandage or dressing from the toes or foot to the area below the knee. The type of compression treatment prescribed is determined by the physician, based on the characteristics of the ulcer base and amount of drainage from the ulcer.
The type of dressing prescribed for ulcers is determined by the type of ulcer and the appearance at the base of the ulcer. Types of dressings include:
- Moist to moist dressings
Recommended Reading: How To Treat A Diabetic Ulcer
Where Should Care Be Carried Out
Patients with venous leg ulcers are best managed in the community for two reasons:
-
Maintenance of independence and mobility is important in this elderly population
-
The number of patients would overwhelm hospital services.,
However, direct access to appropriate specialised hospital services is essential for the investigation of underlying vascular disease and for microbiology, histopathology, and dermatology. Having said that, leg ulcer services provided in hospitals often fail to appreciate how many patients with leg ulcers simply refuse to come to hospital, let alone consent to venous investigation or surgery., Few community patients are prepared to be referred for assessment of their underlying venous disease.,,
Rates of healing have been shown to be improved and costs to be reduced when a coordinated service using research based protocols was introduced.,,, Responsibility for patient care should not be removed from community nurses they should be provided with resources and training aimed at delivering an appropriate, high quality service in specialist leg ulcer clinics. Evidence from our own research in two large health authorities in the United Kingdom showed that standards could be maintained only with close supervision when a leg ulcer service was continued without the direct involvement of a leg ulcer nurse specialist, healing rates declined and costs increased.
Don’t Miss: Signs You Have A Stomach Ulcer
Diagnosis And Treatment Of Venous Ulcers
LAUREN COLLINS, MD, and SAMINA SERAJ, MD, Thomas Jefferson University Hospital, Philadelphia, Pennslyvania
Am Fam Physician. 2010 Apr 15 81:989-996.
Patient information: See related handout on venous ulcers, written by the authors of this article.
Venous ulcers, or stasis ulcers, account for 80 percent of lower extremity ulcerations.1 Less common etiologies for lower extremity ulcerations include arterial insufficiency prolonged pressure diabetic neuropathy and systemic illness such as rheumatoid arthritis, vasculitis, osteomyelitis, and skin malignancy.2 The overall prevalence of venous ulcers in the United States is approximately 1 percent.1 Venous ulcers are more common in women and older persons.36 The primary risk factors are older age, obesity, previous leg injuries, deep venous thrombosis, and phlebitis.7
Venous ulcers are often recurrent, and open ulcers can persist from weeks to many years.810 Severe complications include cellulitis, osteomyelitis, and malignant change.3 Although the overall prevalence is relatively low, the refractory nature of these ulcers increase the risk of morbidity and mortality, and have a significant impact on patient quality of life.11,12 The financial burden of venous ulcers is estimated to be $2 billion per year in the United States.13,14
Composition Of Alginate Dressings
Early use of alginate dressing consisted of fibers of calcium alginate formed into a loose fleece. Recently, this structure has been improved by entangling the fibers so that the dressing is stronger when it becomes soaked with blood or exudate. Alginate dressings can absorb 15-20 times their own weight in exudate and are manufactured in a range of products including flat sheets, ropes, and ribbons. Rope and ribbon dressings are used to pack cavity wounds, while flat sheets are used on surface wounds. Some products are self-adhesive but an appropriate secondary dressing is often used to keep the alginate in place and contain excess exudate.
Sodium alginate is used in some products in order to improve gelling. Other products improve stability by using freeze-dried alginate. The nature of the gel depends on the M, G, and MG groups contained in the alginate. Alginate dressing with high M groups have ribbon-like, flat molecular appearances and form a quicker, softer and more elastic gel. G-rich alginate dressing creates a more chain-like and buckled gel that forms more slowly. G-rich alginate dressings are easy to remove intact, while M-rich alginate dressings tend to dissolve, although they can be removed with irrigation using saline. Note: These dissolving alginates should never be put into a sinus tract or tunneling wound.
Don’t Miss: Mouth Ulcers Treatment Home Remedies
What Happens After Unna Boot Therapy
Once the wound has healed, we often perform vascular studies to determine if there are additional opportunities to help speed recovery.
Depending on your condition, we may help you consider modern vein treatments like Closurefast RFA, Venaseal and Varithena, which when combined with a comprehensive treatment plan can help wounds close quicker and stay closed for longer when indicated.
Have a Wound or Venous Stasis Ulcerthat May Need Treatment?
At Inovia Vein Specialty Centers, we focus on managing issues related to venous insufficiency including venous stasis ulcers, varicose veins, DVTs and more.
What Is Lower Extremity Venous Disease
As blood flows into the veins of the LE, valves within the veins prevent a backflow of blood. The valves play an important role in the development of venous disease. The valves allow for a one-way upward blood flow back to the heart. It adds extra stress by traveling against gravity.
When the valves become weak or incompetent, blood flows back into the veins, creating increased pressure in the venous system. This pressure distends or stretches the walls of the veins, causing the blood to pool. Chronic pressure from swelling on the venous system causes the heme in the red blood cells to leak into the skin. This is called hemosiderin deposits or staining. The LE becomes reddish-brown in color.
Dont Miss: How To Test For Ulcerative Colitis
Don’t Miss: How Does Someone Get Ulcerative Colitis
What Is A Venous Leg Ulcer
venousulcerlegvenous leg ulcers
. Consequently, what causes a venous leg ulcer?
The cause of venous ulcers is high pressure in the veins of the lower leg. The veins have one-way valves that keep blood flowing up toward your heart. When these valves become weak or the veins become scarred and blocked, blood can flow backward and pool in your legs.
Secondly, what are the first signs of a leg ulcer? Symptoms of leg ulcers
- pus in the affected area.
- pain in the affected area.
- increasing wound size.
- generalized pain or heaviness in the legs.
Also Know, what does an ulcer look like on the leg?
They are large, shallow ulcers with uneven edges that drain or weep a lot. Youll likely see swelling in your leg, with red, itchy skin around the wound. You may also experience tightness in your calves, as well as aching, throbbing or a feeling of heaviness in your legs.
How do you treat a leg ulcer?
Treatment for leg ulcers
Cleveland Clinic Heart Vascular & Thoracic Institute Vascular Medicine Specialists And Surgeons
Choosing a doctor to treat your vascular disease depends on where you are in your diagnosis and treatment. The following Heart, Vascular & Thoracic Institute Sections and Departments treat patients with all types of vascular disease, including blood clotting disorders:
Section of Vascular Medicine: for evaluation, medical management or interventional procedures to treat vascular disease. In addition, the Non-Invasive Laboratory includes state-of-the art computerized imaging equipment to assist in diagnosing vascular disease, without added discomfort to the patient. Call Vascular Medicine Appointments, toll-free 800-223-2273, extension 44420 or request an appointment online.
Department of Vascular Surgery: surgery evaluation for surgical treatment of vascular disease, including aorta, peripheral artery, and venous disease. Call Vascular Surgery Appointments, toll-free 800-223-2273, extension 44508 or request an appointment online.
You may also use our MyConsult second opinion consultation using the Internet.
The Heart, Vascular & Thoracic Institute also has specialized centers and clinics to treat certain populations of patients:
Dont Miss: Bland Diet Recipes For Ulcers
Don’t Miss: Is Ibs And Ulcerative Colitis The Same