Where It Starts: The Hospital Bed
When preventing pressure sores in hospitals, hospital beds themselves are determining factors. This is where XSENSORs ForeSite Intelligent Surface system comes in.
The system works using either a mattress overlay or an integrated mattress for hospital beds, embedded with thousands of sensor cells that continuously monitor patient body surface pressures. A bedside monitor displays real-time pressure images and clearly identifies parts of the body under sustained elevated pressure. A turn clock tracks the time between patient repositioning, and alerts staff to adjust their rotation.
This, ultimately, leads to every medical professionals goal: quality patient care and positive patient outcomes. With the support of XSENSORs technology, medical staff can focus on patient care where it is most needed, putting their energy into essential clinical activities, and not into preventative efforts that are unnecessary such as waking sleeping patients to rotate them, if they arent truly at risk of developing pressure sores.
Through providing caregivers with consistent information, XSENSORs ForeSite IS increases the integrity in continuity of care, helps avoid pressure ulcers from forming and may improve healing time for existing wounds to also reduce the length of hospital stays due to pressure ulcers.
The system comes with:
Donât Miss: How To Soothe Mouth Ulcers
How Often Is Repositioning Necessary
Even though it’s often recommended that people be repositioned every two hours, there’s no single recommendation that works for everyone. Some people can lie in the same position for quite a long time without getting ulcers, while others need to switch much more often. Research has not yet found out how often someone should change position to get the best preventive effect.
Unnecessarily moving someone too much for no good reason can also have disadvantages. For instance, repositioning every two hours at night may wake the person each time and keep them from getting a good nights sleep. Changing position can also be very painful for people who have wounds or joint conditions. Frequent repositioning is physically demanding for caregivers or family members too. It’s therefore important to observe how often someones position really needs to be shifted. It can then help to make a note every time they are repositioned.
What Other Kinds Of Aids Are Available
Another thing that can help prevent damage to the skin is sheepskin mattress covers. Some people find sheepskin unpleasant, though, because it can make your skin very warm after a while.
Pressure ulcers often occur on peoples heels. So heels are often elevated using pillows, or special heel protectors made out of animal skin or foam are used. But there is no proof that these actually prevent pressure ulcers. Some people find the heel protectors uncomfortable and choose not to wear them. There are also concerns that they could increase the risk of falling if people get up and walk around while wearing them.
There hasn’t been much research on aids such as special positioning cushions or special cushions for people to sit on either.
Don’t Miss: Best Wound Care For Stage 2 Pressure Ulcer
Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
Treating And Preventing Pressure Ulcers
Treatment for pressure ulcers includes the use of dressings, creams and gels designed to speed up the healing process and relieve pressure. Surgery is sometimes recommended for the most serious cases.
For some people, pressure ulcers are an inconvenience that require minor nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning or gangrene.
Read more about the complications of pressure ulcers.
Pressure ulcers can be unpleasant, upsetting and challenging to treat. Therefore, a range of techniques is used to prevent them developing in the first place. These include:
- regularly changing a person’s position
- using equipment to protect vulnerable parts of the body such as specially designed mattresses and cushions
Read about treating pressure ulcers and preventing pressure ulcers for more information.
Unfortunately, even with the highest standards of care, it’s not always possible to prevent pressure ulcers in particularly vulnerable people.
Also Check: Ulcerative Colitis Biologics Side Effects
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Additional Information
Tools
Practice Insights
The Hospital As A Place Of Risk For Pressure Ulcers Patients
It has already been briefly mentioned in the introduction to this blog: pressure ulcers also occur in hospitals. Nurses and doctors can use their medical knowledge to combat pressure ulcers through a so-called pressure ulcer prevention protocol. Attention should be paid to the presence of preventive and curative means. Thus pressure ulcers can be prevented and cured. And as a wise Dutch saying goes prevention is better than cure.
Read Also: Which Of The Following Are Classic Features Of Ulcerative Colitis
Management Of Pressure Ulcers
When a pressure ulcer develops, nursings patient safety goal is to assist the health care team in closing the ulcer as quickly as possible. Nursing is also concerned with preventing further ulcer deterioration, keeping the ulcer clean and in moisture balance, preventing infections from developing, and keeping the patient free from pain.
Many aspects of managing pressure ulcers are similar to prevention . Clearly, the health care team has to address the underlying causes or the pressure ulcer will not close. In 1994, AHRQ published clinical practice guidelines on treating pressure ulcers. Much of the evidence related to treating pressure ulcers was based on Level C evidence, requiring one or more of the following: one controlled trial, results of at least two case series/descriptive studies in humans, or expert opinion. Although the AHRQ document was published 13 years ago, it provides the foundation for treating pressure ulcers. The document identified specific indices . The following section supplements this document.
Do Organizational Members Understand Why Change Is Needed
Readiness requires both the capability to make changes and the motivation to make the change. That motivation may be helped along by external factors, such as Federal or State mandates. But it is most likely to be strong and enduring if based on a clear understanding of the concerns behind the planned change at all levels of the organization.
There are many potential reasons to implement a pressure ulcer prevention program. While we offer general reasons and statistics in the box below, local reasons or cases may be more tangible and compelling. For example:
- Has your facility experienced a significant increase or spike in pressure ulcer rates?
- Is your facility responding to changes in CMS reimbursement policy?
- Have there been any notable adverse events that were pressure-ulcer related?
- Has your facility been the target of a legal action related to a pressure ulcer?
- Do staff members have personal experience of a family member affected by a pressure ulcer?
While those who have initiated a focus on pressure ulcer prevention may clearly understand the needed changes and the reasons for them, there may be great variation across the organization in levels of knowledge and motivation in this area. Others in your hospital may have different reasons, so it is important to define the issues and reasons for change. This process will help make the case for why a pressure ulcer prevention initiative is needed now.
Action Steps
Tools
Resources
Additional Information
Also Check: Wound Treatment For Diabetic Foot Ulcers
Sample Size And Sampling Procedure
The sample size was determined by using a single population proportion formula with the assumption of 54.4% Proportion , 95% confidence level and 5% margin of error. Since the source of the population was less than 10,000 , a correction formula was used. Using 10% nonresponse the final sample size obtained was 220. Then, the number of participants in each selected hospital to take a similar proportion of participants were determined using the proportionate population sampling.
What Role Do Diet And Skin Care Play
Some people who are hardly able to move don’t get very hungry or thirsty. In order for them to stay in good physical condition, though, it’s important to make sure they get enough to eat and drink. Eating too little or a very unbalanced diet and hardly having anything to drink may weaken their skin even more. Some people take dietary supplements, but there’s hardly any research on whether these products can help prevent pressure ulcers.
It’s important to keep the skin from getting too dry, but also to prevent it from being exposed to constant moisture either one increases the likelihood of damage to the skin. There’s not yet enough good research to be able to say whether regular use of creams or lotions can prevent pressure ulcers.
Don’t Miss: Ulcerative Colitis And Leg Pain
What Are The Symptoms Of Bedsores
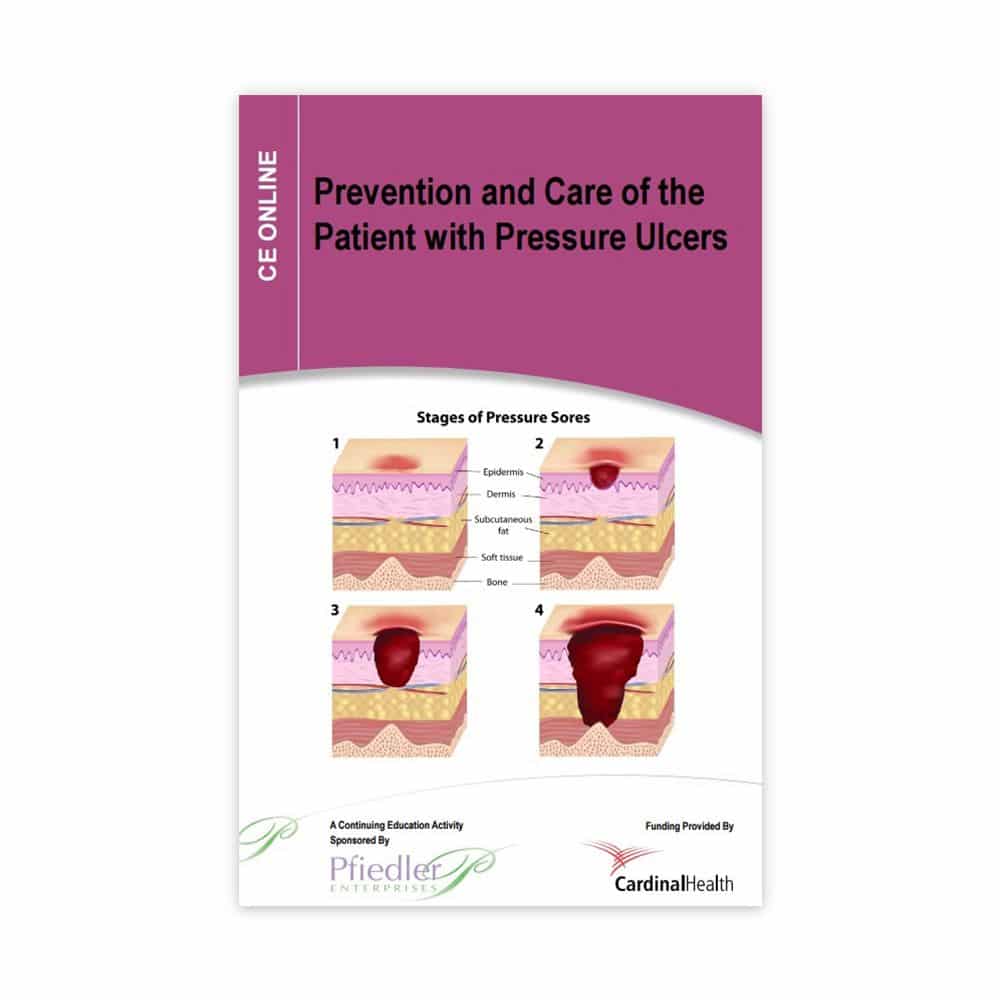
Bedsores are divided into 4 stages, from least severe to most severe. These are:
- Stage 1. The area looks red and feels warm to the touch. With darker skin, the area may have a blue or purple tint. The person may also complain that it burns, hurts, or itches.
- Stage 2. The area looks more damaged and may have an open sore, scrape, or blister. The person complains of significant pain and the skin around the wound may be discolored.
- Stage 3. The area has a crater-like appearance due to damage below the skin’s surface.
- Stage 4. The area is severely damaged and a large wound is present. Muscles, tendons, bones, and joints can be involved. Infection is a significant risk at this stage.
A wound is not assigned a stage when there is full-thickness tissue loss and the base of the ulcer is covered by slough or eschar is found in the wound bed. Slough may be tan, grey, green, brown, or yellow in color. Eschar is usually tan, brown or black.
Sociodemographic Characteristics Of Nurses

The total number of eligible nurses was 220 of these, 212 were volunteered to participate in the study, a response rate of 96.3%. Most of them were males . The mean age among the study participants was 28.2±5.2 years. Majority of study participants were a diploma holder in nursing, 71.2% had 510years of clinical experience in the nursing profession. One hundred sixty of the participants attended education on PU almost half of them got PU education at University/ college education. One hundred fifty-six did not read articles about pressure ulcer, while, 138 of the participants had no exposure to PU training as illustrated in .
Table 1 Demographic characteristics of the nurses
Don’t Miss: Best Vitamins For Ulcerative Colitis
Which Hospitals Do The Hac Reduction Program Apply To
As set forth under Section 1886 of the Social Security Act, the HAC Reduction Program applies to all subsection hospitals .
Some hospitals and hospital units, such as the following, are exempt from the HAC Reduction Program:
- Critical access hospitals
- Prospective Payment System-exempt cancer hospitals
- Veterans Affairs medical centers and hospitals
- Short-term acute care hospitals located in U.S. territories
- Religious nonmedical health care institutions
Note: For a full description of subsection hospitals, refer to the Social Security Act on the Social Security Administrations website at .
Family And Individual Level
Healthcare professionals can have an impact on an individual level by:
- recognising the important role individuals, families and carers have in preventing and managing pressure ulcers
- engaging individuals, carers and families in what to look for and how pressure ulcers can be prevented
- using appropriate literature with visual images to explain how quickly pressure ulcers can develop
- educating the individuals and caregivers about the causes, assessment and management of pressure ulcers
- using appropriate terminology recognising and informing patients that pressure ulcers is another term for bed sores
- encouraging individuals to move independently whenever possible
- directing individuals to appropriate healthcare professionals if they suspect a pressure ulcer is forming or is present
- looking out for skin discolouration or soreness, particularly in areas where bones are close to the skin
- repositioning or turning patients frequently at least every 2 hours for those patients who need help
- using moving and handling aids to help reposition individuals who require assistance moving
- performing regular skin inspections to check areas at risk and document pressure areas at least once a day
- checking that patients with pressure ulcer risk factors are registered with a GP and receive primary health care support to minimise the risks
- providing holistic health assessments for people at risk of developing pressure ulcers
Donât Miss: Foods You Can Eat With An Ulcer
Recommended Reading: Safe Desserts For Ulcerative Colitis
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Study Analysis Quality And Risk Of Bias
Study quality was assessed using the evidencebased librarianship Critical Appraisal checklist.19 This tool assessing validity, applicability, and relevance of included studies was based on four domains of research: population, data collection, study design, and results. The overall validity of the studies was determined based on the Yes scores 75% or No/Unclear scores 25%. Two researchers rated the articles, and discrepancies were resolved by agreement.
Also Check: Could I Have A Stomach Ulcer
The Implications Of Pressure Injuries
Its no secret that pressure injuries can become incredibly serious, from deep tissue damage all the way to sepsis, resulting in death. Developing pressure sores can lead to skin damage and infection, causing injuries that are, in many cases, preventable. They also place a significant legal strain on hospitals. According to the Agency for Healthcare Research and Quality, there are more than 17,000 lawsuits filed related to pressure ulcers a year, and the pressure ulcers themselves cost between $9.1 billion and $11.6 billion a year in fees.
With unnecessary patient suffering and legal issues both at stake, its important to create a culture of urgency within hospitals to reduce pressure sore cases among patients. By becoming quickly aware of the issues and monitoring skin from the beginning, this is much easier to do.
Key Aspects Of Pressure Ulcer Prevention
Standard practices aimed at preventing pressure ulcers include:
- Risk assessment to identify at risk patients in combination with a skin assessment)
- Skin and tissue assessment to look for signs of early pressure damage
- Preventive skin care to promote skin integrity and protect the skin from damage
- Use of support surfaces to reduce the magnitude of pressure
- Keeping the head of the bed at or below 30 degrees elevation in order to reduce the risk of shear
- Use of prophylactic dressings to areas frequently exposed to friction and shear
- Turning and repositioning patients to reduce the duration of pressure
- Providing nutrition and hydration to maintain tissue tolerance for pressure
Read Also: Yea Sacc For Horses With Ulcers
Read Also: Are Apples Good For Ulcerative Colitis
Are We Ready For This Change
Because pressure ulcer care is complex, efforts to improve pressure ulcer prevention require a system approach that will involve organizational change. Bringing about organizational change of any type is difficult. It is even more difficult when it involves multiple, simultaneous modifications to workflow, communication, and decisionmaking as are needed in a pressure ulcer prevention initiative. Failure to assess your organization’s readiness for the change at multiple levels can lead to unanticipated difficulties in implementation, or even the complete failure of the effort. Each of the questions below will help you and your organization explore readiness and identify action steps to improve it, if necessary.
Under What Circumstances Do Bedsores Develop
Pressure sores occur with prolonged pressure. Concentrated pressure, that is, pressure on a relatively small spot on the body, causes pressure sores to form. As pressure increases and persists for longer periods, bedsores become more severe.
Places where the bone is close to the skin are most susceptible to pressure sores. High-risk areas include the back of the head, the seat, the heels and the hips.
Don’t Miss: How To Soothe Mouth Ulcers