Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
Healing Your Ulcerative Proctitis
Ulcerative proctitis treatment or cure for rectal inflammation, includes anti-inflammatory medication such as canasa, hydrocortisone enemas, foams & suppositories, herbal treatments, acupuncture, and going on acolitis diet.Common symptoms are rectal bleeding and rectal pain.
Definition: When inflammation occurs in the rectum and the lower part of the colon, the last 15-20 cm, you have ulcerative proctitis.
Misspellings: ulcerative proctatitis, ulcerated proctitis, ulceritive proctitis, ulcerative proctitus, ulcertive proctitis, ulcerative protitis, ulcerative proctisis, ulcerated proctitus
How Is Proctitis Diagnosed
To diagnose proctitis, a health care provider will take a complete medical history and do a physical exam. The health care provider will ask the patient about symptoms, current and past medical conditions, family history, and sexual behavior that increases the risk of STD-induced proctitis. The physical exam will include an assessment of the patients vital signs, an abdominal exam, and a rectal exam.Based on the patients physical exam, symptoms, and other medical information, the doctor will decide which lab tests and diagnostic tests are needed. Lab tests may include blood tests such as a complete blood count to evaluate for blood loss or infection, stool tests to isolate and identify bacteria that may cause disease, and an STD screening. The doctor also may use one of the following diagnostic tests:
Recommended Reading: Drugs To Treat Ulcerative Colitis
Acg Releases Updated Practice Guidelines For Ulcerative Colitis In Adults
KAREN HELLEKSON, PH.D.
Am Fam Physician. 2005 Feb 1 71:604-611.
The American College of Gastroenterologyâs Practice Parameters Committee has issued updated practice guidelines for the treatment of ulcerative colitis in adults. The guidelines were generated by an expert panelâs review of published evidence and outline the preferred approaches to the treatment of patients with ulcerative colitis, a chronic disease characterized by diffuse mucosal inflammation of the colon and marked by bloody diarrhea, rectal urgency, and tenesmus. Ulcerative colitis affects 250,000 to 500,000 people in the United States each year resulting in steep hospital and drug costs as well as lost work. The full text of the updated practice guidelines, which originally appeared in the July 2004 issue of the American Journal of Gastroenterology, is available at http://www.acg.gi.org/physicians/guidelines/UlcerativeColitisUpdate.pdf.
The quality of evidence on which a recommendation is based is as follows:
Grade A: Homogenous evidence from multiple well-designed randomized or cohort controlled trials, each involving a number of participants to be of sufficient statistical power.
Grade B: Evidence from at least one large well-designed clinical trial with or without randomization, from cohort or case-control analytic studies, or well-designed meta analyses.
Grade C: Evidence based on clinical experience, descriptive studies, or reports of expert committees.
How Do You Get An Ulcerative Colitis Diagnosis
One important thing to note is that people with more severe cases of ulcerative colitis are at an increased risk of developing colon cancer and other serious health conditions, like liver disease, Rudolph Bedford, M.D., a gastroenterologist at Providence Saint Johnâs Health Center in Santa Monica, California, tells SELF. Thats why its important to reach out to a medical professional if you do have any of the above symptoms.
However, an ulcerative colitis diagnosis can be challenging because other conditions can mimic symptoms of IBD, like infections or even hemorrhoids, Dr. Sinha says. In terms of differentiating between Crohns and ulcerative colitis, he says, Theres no single test that we have that 100% distinguishes between the two. We rely on the patient history and other information such as radiographic imaging and endoscopy. Doing a colonoscopy, for example, can be one of the most reliable ways to identify IBD and to then distinguish between Crohns and ulcerative colitis.
While a colonoscopy is an effective tool, Dr. Sinha clarifies that its not the only way. Rather, theres an entire constellation of tests and data that can be considered, including imaging, lab tests, and a detailed intake of the patients symptoms and presentation.
Also Check: Ulcerative Colitis High Calorie Diet
Complementary Treatments And Therapies
You may consider these approaches in addition to what your doctor prescribes. But itâs important to talk to your medical team about any and all of them because some, like supplements, can interfere with treatments from your doctor. Letâs take a look at a few:
Mind-body therapies:Stress and anxiety are well-known triggers for many people with ulcerative colitis, so it is not surprising that mind-body relaxation techniques could help. These techniques help nurture a healthy connection between your mind and body as well as between you and the outside world. In some cases, they encourage behavior changes in your everyday life. They may be worthwhile if only to lessen anxiety and depression linked to UC and improve quality of life. In addition, there is some evidence that yoga, meditation, and gut-centered hypnotherapy could help with some physical symptoms or flare-ups of UC. Some of the techniques, like cognitive behavioral therapy and patient support groups, have been so successful that they have slowly become a part of mainstream treatment for IBD.
Keep in mind that the FDA doesnât regulate supplements, so claims on packaging may not be accurate. Thatâs yet another reason why itâs important to talk to your doctor before you start taking any supplements for your UC.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Don’t Miss: Cabbage Juice Recipe For Ulcerative Colitis
Skipping Or Forgetting To Take Your Uc Medication
UC causes inflammation and ulcers in the colon. If left untreated, this condition can lead to life threatening complications, such as:
- bowel perforation
- colorectal cancer
- toxic megacolon
Your doctor will likely prescribe a medication to reduce inflammation, such as an anti-inflammatory drug or an immunosuppressant drug.
These medications help ease symptoms of UC and can also function as maintenance therapy to keep you in remission. Symptoms could return if you dont take your medication as directed.
At some point, your doctor may discuss slowly tapering off the medication. However, you should never decrease your dosage or stop taking your medication without speaking with your doctor first.
Prognosis In Ulcerative Colitis
UC is a chronic, lifelong disease. Most UC patients lead normal lives and have a typical lifespan. Fertility is similar to that in the general population, and most women are able to conceive and have children.
Some patients with UC become incapacitated by persistent or refractory symptoms. Rare complications include fulminant disease and toxic megacolon. Patients with UC are at greater risk of developing colorectal cancer than the general population.11 This risk is related to the extent and persistence of inflammation and the duration of the disease. Today, with the use of regular surveillance for precancerous changes and effective treatment, the risk of cancer has been markedly reduced.
Read Also: Foods Bad For Ulcerative Colitis
Prognosis Of Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have ulcerative proctitis have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
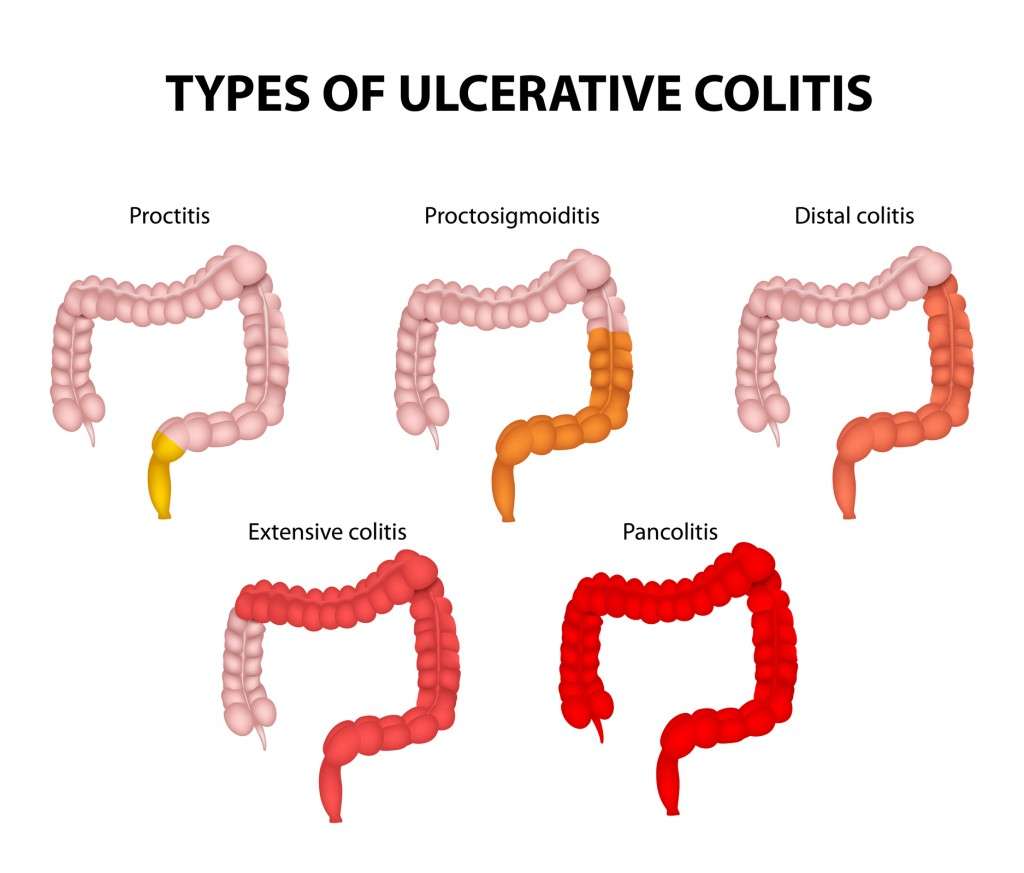
Mild To Moderate Ulcerative Colitis: Disease State
Idiopathic inflammatory bowel disease represents a spectrum of conditions, with ulcerative colitis on one end and Crohns disease on the other. UC is typically a diffuse continuous superficial inflammation that always begins within the rectum and affects the proximal colon to a varying extent. The disease is limited to the rectum in approximately a third of patients, to the left side of the colon in another third, and to the splenic flexure or beyond in the remaining third. UC does not typically involve the small intestine, although a small percentage of patients may have a limited superficial inflammation of the terminal ileuma condition termed backwash ileitis. Although the inflammation associated with UC is usually superficial, it can extend throughout the mucosa in patients with severe ulcerations, a condition known as fulminant colitis or toxic megacolon. Approximately 10% of patients have an overlap between UC and CD, in which inflammation is limited to the colon.1
Read Also: Best Diet For Ulcerative Colitis Flare Up
How Long Does An Ulcerative Colitis Flare
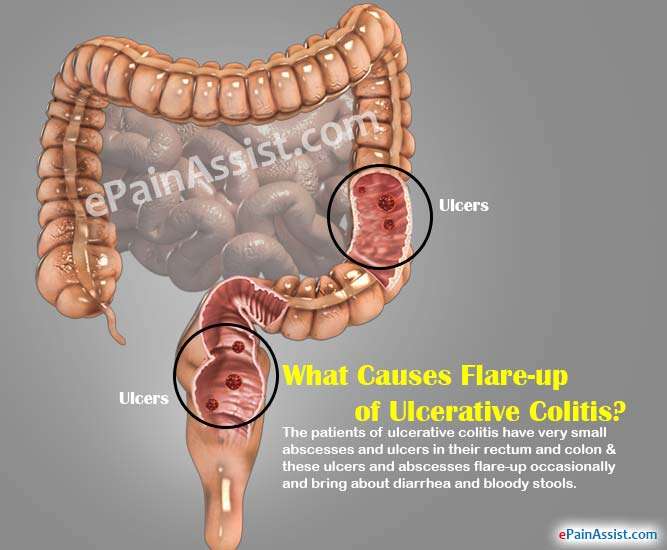
Ulcerative colitis is a chronic disease that causes inflammation and ulcers in the inner lining of the large intestine and rectum. If you have UC, you may experience repeated cycles of flare-ups and remissions .
A flare-up can last a few days or a few weeks and then be followed by a remission that lasts for months or even years. How long a flare-up lasts depends on factors such as:
While there is no cure for UC, several treatment options and lifestyle modifications can help reduce symptoms or prevent flare-ups.
Current Treatment Approaches For Mild To Moderate Ulcerative Colitis
Combined clinical and endoscopic remission in the CORE I and II trials, which compared budesonide MMX at 2 doses vs placebo in patients with mild to moderate UC.
Gastroenterology.Aliment Pharmacol Ther.
Corticosteroids may be considered in patients who have active symptoms despite optimized mesalamine therapy. In the population of patients with moderate or severe UC, it may also be reasonable to initiate treatment with corticosteroids when needed, given the potential long-term benefits. The use of corticosteroids might be considered a tipping point in the treatment of UC, indicating a more virulent disease course. If corticosteroids are required twice within a year or if a patient has a severe flare of IBD mandating parenteral corticosteroids, there is a need for a corticosteroid-sparing agent. Although immunomodula-tors were historically used for these patients, most clinicians would now advocate the use of biologic treatment.
You May Like: Exercising A Horse With Ulcers
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
You May Like: Is Alcohol Bad For Ulcerative Colitis
What Foods Heal Ulcerative Colitis / What Drinks Are Good For Ulcerative Colitis
There is scientific evidence that wheatgrass helps to reduce active ulcerative colitis symptoms. There is also evidence that green tea can help calm the symptoms of ulcerative colitis. No food or drink, however, can induce remission or help prevent flare-ups. However, Lactobacillus and E. coli probiotics, have shown benefit in some studies in preventing flare-ups.
Don’t Miss: What Should You Eat If You Have Stomach Ulcers
Inflammation Of The Rectum
Symptoms may be different if a flare-up only affects the rectum and not the colon. You may have fresh bleeding from the rectum and you may form normal stools rather than have diarrhoea. You may even become constipated further up in the unaffected higher part of the colon but with a frequent feeling of wanting to go to the toilet.
How Long Do Flares Last
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment.
Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
The Crohns & Colitis Foundation recommends waiting to become pregnant until UC has been in remission for at least 3 months.
If you conceive during a flare-up, you may have more symptoms during pregnancy.
Youre likely to have a healthy pregnancy if you have UC, but youll still have a higher chance of complications than someone without the condition. Particularly if your UC is active, you may have a greater risk for:
- miscarriage
In general, UC medications can be taken during pregnancy.
Talk with your doctor about any possible changes to your medications while pregnant.
Ideally, having a conversation with your doctor prior to getting pregnant can allow them to prepare a UC treatment plan in advance that can be revised, if and as needed, during your pregnancy.
Read Also: Home Remedies For Stomach Ulcer In Tamil
Home Remedy For Ulcerative Proctitis With Chitosan
Chitosan is an all-natural Chinese medicine based on chromium and amongst the best natural remedies for ulcerative proctitis with hemorrhage. Its made from natural marine red crab shells, this medicine has no contraindications.Take two pills per day around 5-7 in the morning on an empty stomach.The easiest way is to dissolve the capsules in ½ cups of warm water beforehand. In addition, licorice tea is amazing.
What Are The Treatment Options For A Flare
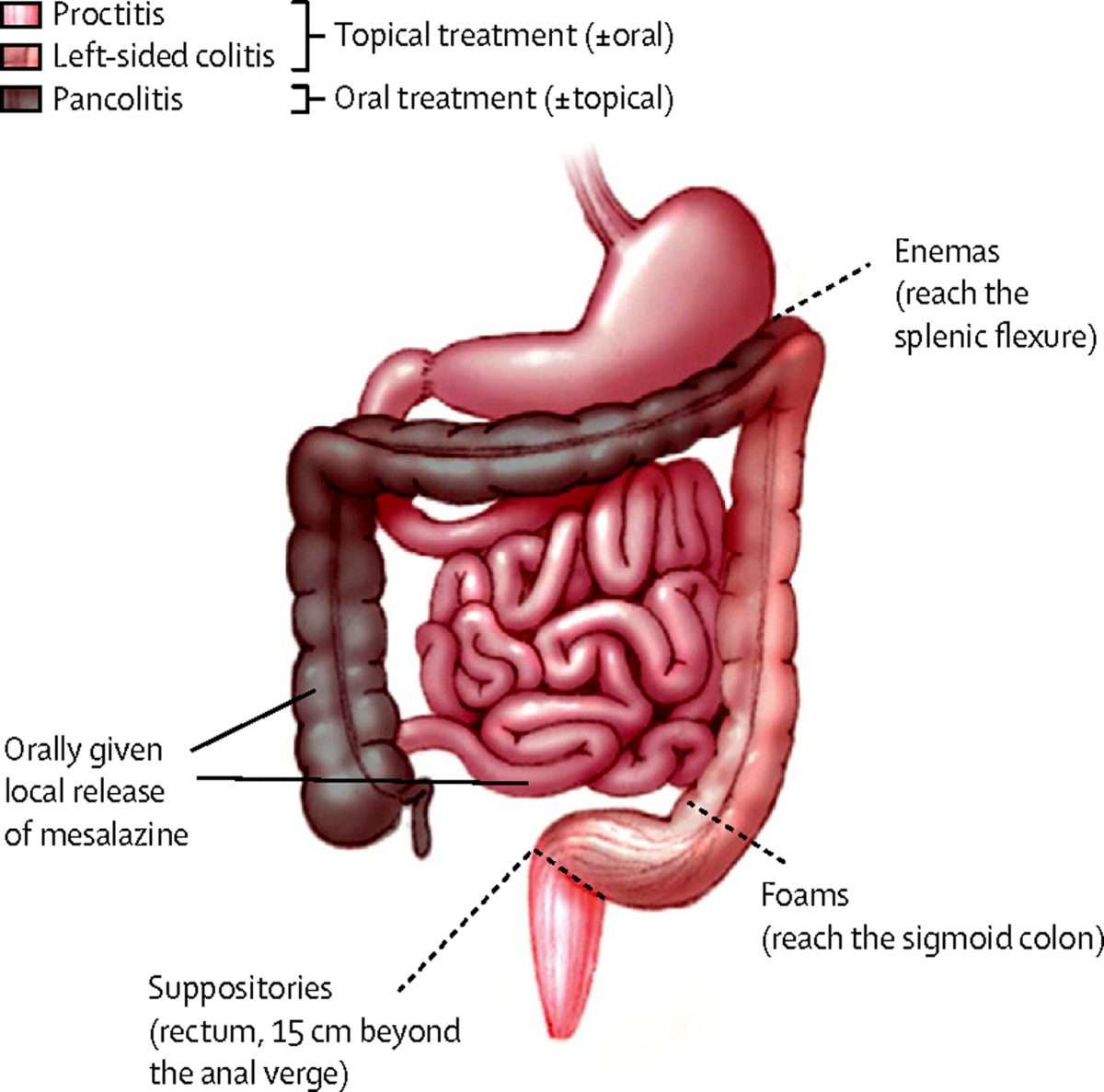
When you first develop ulcerative colitis it is usual to take medication for a few weeks until symptoms clear. A course of medication is then usually taken each time symptoms flare up. The medicine advised may depend on the severity of the symptoms and the main site of the inflammation in the colon and the rectum .
Topical treatments applied locally by an enema or suppository are widely used for treating ulcerative colitis, particularly aminosalicylate and steroid medicines – see below. They are a treatment option if ulcerative colitis affects only the lower part of the bowel .
Medication options include the following:
Read Also: Stomach Ulcer Treatment Over The Counter
Reducing Diarrhea Bloating And Gas
Certain foods can worsen symptoms of your condition and aggravate your rectum. Mayoclinic.com recommends limiting dairy intake to reduce diarrhea. In some cases, you might need to eliminate it completely. You should work with a dietitian to ensure adequate calcium intake from other sources.
Foods that contribute to gas and bloating include cruciferous vegetables like broccoli and cabbage, beans, popcorn, fatty and greasy foods and raw fruit juice. Alcohol and caffeine stimulate the intestines, which can worsen diarrhea, while carbonated drinks can cause gas.
What Are Some Practical Steps To Take When A Flare
The first thing to do if a flare up occurs is to make sure you are eating a healthy diet which is low in fibre and contains plenty of water. Avoiding dairy products and cutting down carbohydrates may also help. The vast majority of people will requite adjustments to their medication, so you should seek medical advice from your GP or specialist.
Read Also: Does Turmeric Help Ulcerative Colitis
You May Like: Food For Ulcer Patient In Nigeria
Who Develops Ulcerative Colitis
About 2 in 1,000 people in the UK develop ulcerative colitis. It can develop at any age but most commonly first develops between the ages of 10 and 40. About 1 in 7 cases first develop in people over the age of 60 years. Non-smokers are more likely than smokers to develop ulcerative colitis. However, smoking brings other dangers to health which far outweigh this benefit.
Donât Miss: What Is A Decubitus Ulcer Why Does It Occur
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Don’t Miss: Foods To Avoid If You Have A Stomach Ulcer