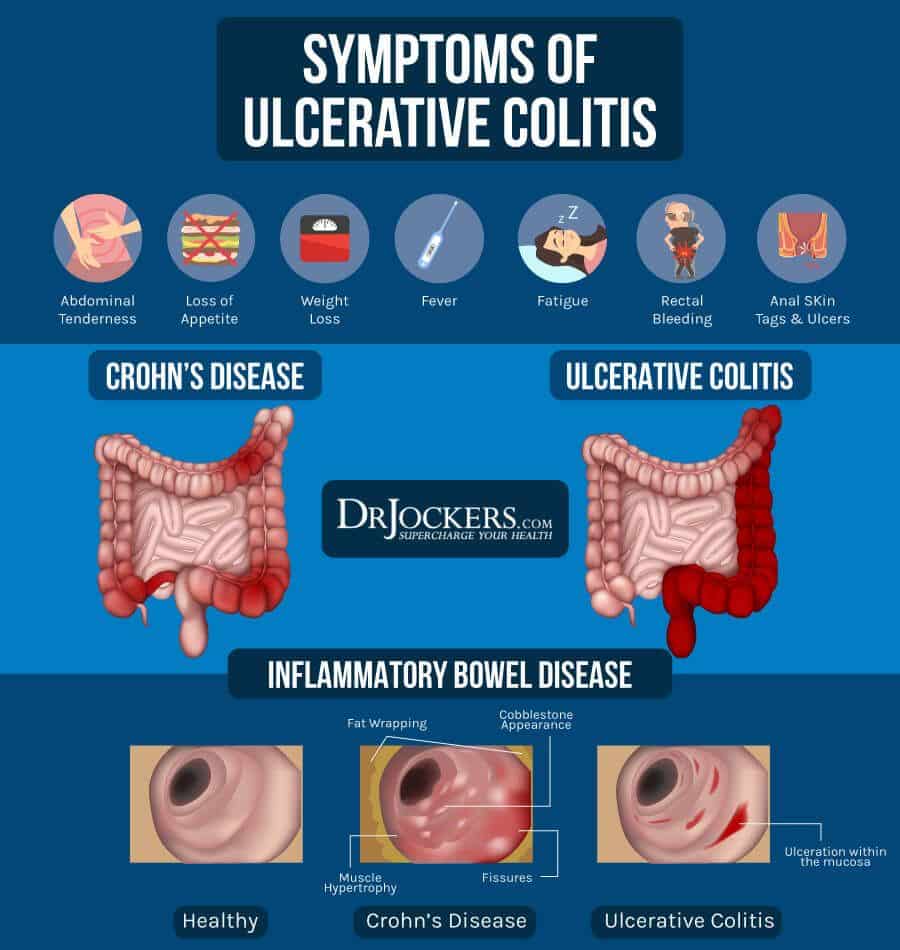
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
What Causes Ulcerative Colitis Flare Ups In The First Place
The experts arent exactly sure what causes UC, but they think its prob an autoimmune condition. Autoimmune conditions are basically what happens when the bodys defense mechanism is a little overzealous and attacks healthy tissue. Your body *means* well, but it causes inflammation.
In the case of UC, scientists think that the immune system might accidentally mistake perfectly harmless bacteria in the colon for serious threats, which causes the whole region to essentially swell up.
Though they dont know exactly what contributes to flare ups, a few possibilities include:
- Stress. According to 2016 research, being stressed out may trigger IBD flare-ups. Even though stress doesnt seem to directly cause UC, it does appear to weaken the intestinal wall and make it more vulnerable to issues. Researchers found that stress increased microbe activity in the colon and hindered the immune response.
- Diet. In a 2020 review, researchers found a correlation between diet and UC flare-ups. However, the research on exactly what triggers them just isnt there yet.
- Certain medications. Abruptly stopping medications like steroids or maintenance therapies, which slow the bods natural cortisol levels, can lead to flares and other negative side effects. Always talk to a doc before halting these drugs.
- Hormonal changes. There seems to be a link between IBD and hormonal changes in women, with some research from 2018 suggesting that UC symptoms worsen during pregnancy in particular.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
You May Like: Mepilex Border Sacrum Pressure Ulcer Prevention
What Are Some Practical Steps To Take When A Flare
The first thing to do if a flare up occurs is to make sure you are eating a healthy diet which is low in fibre and contains plenty of water. Avoiding dairy products and cutting down carbohydrates may also help. The vast majority of people will requite adjustments to their medication, so you should seek medical advice from your GP or specialist.
What To Look For In A Meal Kit
While food triggers vary by person, Kennedy recommends looking for meals with soluble sources of fiber, which tend to be easier to digest and cause less inflammation in the digestive tract.
Things like white rice are minimally processed but still a great source of soluble fiber are great to look for, as are fruits and vegetables that either have the skin removed or can be removed during the prep process, she says.
But the general rule of thumb, says Kennedy, is that whatever meal delivery kit you choose, always opt for foods in their purest, most whole forms. The key is to find meals that use minimally processed foods, and preferably whole foods all together.
Heres a peek at the best meal delivery options for people with ulcerative colitis.
You May Like: Best Treatment For Ulcerative Colitis Flare Up
Also Check: Mouth Ulcer On Tongue Remedies
How Is Ulcerative Colitis Treated
Treatment for UC depends on the severity of the disease and often involves both medications and lifestyle modifications.
Medications
Most people require a combination of medications to suppress and/or modulate the immune system:
- Anti-inflammatory drugs: Anti-inflammatory drugs such as 5-aminosalicylates and corticosteroids suppress the cells that cause inflammation. These drugs are usually the first step in the treatment of UC and are well tolerated by most people.
- Immune system suppressors: Immunosuppressant drugs work by suppressing the immune system response that stimulates the inflammation process. Examples include Azasan and Imuran Purinethol and Purixan Gengraf, Neoral and Sandimmune and Xeljanz .
- Biologics : Biologics target and neutralize proteins produced by the immune system. Examples include Remicade , Humira and Simponi . Entyvio is a type of biologic that works by blocking the inflammatory cells from reaching certain parts of the body, and can be used for people who cant tolerate other biologics.
- Anti-diarrheal medications: Your doctor may recommend anti-diarrheal medications such as Imodium for severe diarrhea. You should avoid taking over-the-counter anti-diarrheal medications without consulting your doctor, because they can increase the risk of toxic megacolon .
- Painkillers: Tylenol is safe to use for pain relief. Talk to your doctor before taking other OTC pain medications.
- Antispasmodic medications: Antispasmodic medications can help reduce cramps.
When To See A Doctor
Maybe its food poisoning or a stomach bug.
I really dont want to bother the doctor.
Sound familiar? While its totally normal to want to talk yourself out of going to see your doctor, this is probably not the best approach.
Honestly, I prefer that patients tell me right away when they start having symptoms, so we can treat the flare early and often with simpler measures before it becomes more severe and more complicated or requires hospitalization, Dr. Charabaty says.
If you any ulcerative colitis symptoms flare up, call your doctor so you both can work to see whats going on and keep your symptoms from worsening. If you have severe abdominal pain and a high fever, its best to head to the emergency room, according to the Crohns and Colitis Foundation.
When you do see a doctor, this isnt a time to shy away from talking about how ulcerative colitis is affecting more than your belly, if thats the case for you.
It is really important for women with ulcerative colitis to talk about their mental health with their treating physicians and it is crucial to treat depression and anxiety as a part of a comprehensive care of IBD, Dr. Charabaty says. The mental health affects the physical health and vice versa, and both components need to be addressed to keep ulcerative colitis in remission and improve quality of life.
Read Also: I Think I Have An Ulcer What Should I Do
Also Check: Can Eliquis Cause Stomach Ulcers
Complications Of Ulcerative Colitis
Although people with ulcerative colitis commonly have minor liver dysfunction, only about 1 to 3% have symptoms of liver disease, which vary from mild to severe. Severe liver disease can include inflammation of the liver , inflammation of the bile ducts , which narrow and eventually close, and replacement of functional liver tissue with scar tissue . Inflammation of the bile ducts may appear many years before any intestinal symptoms of ulcerative colitis. The inflammation greatly increases the risk of cancer of the bile ducts and also seems to be associated with a sharp increase in the risk of colon cancer.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Recommended Reading: Natural Way To Cure Ulcer
Prognosis For Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have disease only in their rectum have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
What To Do During An Ulcerative Colitis Flare To Minimize Symptoms
Youll inevitably experience another UC flare-up at some point, despite your best prevention efforts. When this happens, there are a few ways youll need to tweak your normal routine to minimize the severity of your symptoms and get back into remission ASAP. Even some of your typically healthy habits like loading up on veggies may be a no-go. Here are a few natural remedies that may help:
Don’t Miss: Acupuncture For Ulcerative Colitis Treatment
Diet Tips During A Flare
A modified diet may help you manage and reduce your UC symptoms. Depending on the person, specific foods may trigger flare-ups or worsen symptoms. As a result, its important to identify and limit these foods.
Your doctor and a dietitian can work with you to find a diet that best manages your symptoms while providing the nutrition you need.
Why Its Crucial To Act Immediately
If its not clear by now, this condition contains the word toxic because left untreated, toxic megacolon is potentially deadly. Dr. Murray underscores, Toxic megacolon is a potentially life-threatening condition that requires prompt diagnosis and treatment. Left untreated, toxic megacolon will eventually lead to these complications:
The bottom line, according to Dr. Murray: If you suspect you have toxic megacolon, you must take it seriously. When in doubt, you should get to the hospital or contact your gastroenterologist for further instruction. It can be difficult to distinguish toxic megacolon from other intra-abdominal conditionsevaluation by an emergency medicine physician can help determine if you do or do not have the condition, Dr. Murray says.
You May Like: Natural Medicine For Ulcerative Colitis
How Do You Calm A Colitis Flare Up
Read Also: What To Use For Stomach Ulcer
When To Call The Doctor
- Cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and drugs
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- A feeling of having little warning before you need to have a bowel movement
- A need to wake up from sleeping to have a bowel movement
- Failure to gain weight, a concern for a growing infant or child
- Side effects from any drugs prescribed for your condition
Don’t Miss: Foods To Stay Away From With Ulcers
What Foods Should I Avoid If I Have Ulcerative Colitis
Again, each person who has ulcerative colitis will need to find their personalized diet. However, here are some of the most common types of foods that trigger ulcerative colitis:
Raw Green Vegetables
You should avoid foods that give you more stool. Foods that do this are most often foods with a lot of fiber.
Green or cruciferous vegetables contain a large amount of fiber, especially when they are raw. If you have ulcerative colitis, you should try to stick to fully cooked, skinless, and non-cruciferous vegetables.
Some examples of cruciferous vegetables are:
Speak With Your Doctor
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
You May Like: Best Foods To Eat When You Have A Stomach Ulcer
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Dietary Recommendations For Ulcerative Colitis
There are different dietary recommendations for each stage of Ulcerative Colitis, active and remission. Recommendations mainly revolve around the amount of dietary fiber in your diet. During a flare its best to minimize the amount of fiber in your diet, whereas during remission fiber can be a beneficial part of your diet. Fiber is a tough nutrient for the gut to digest so during a flare, when the gut is already stressed, fiber can aggravate the symptoms of Ulcerative Colitis. Fiber also adds residue to stool, which should be avoided to allow the bowels to rest and heal. This is specifically true for insoluble fiber, which does not dissolve, and moves through your GI tract unchanged. Consuming fiber during a flare can increase bloating, gas, diarrhea, and abdominal pain, and may even lead to intestinal blockage.
Active
When UC is active, let your bowel rest as much as possible. Therefore, we recommend a low fiber, low residue diet:
- Low fiber fruit: bananas, cooked fruit, canned fruit
- Non-cruciferous vegetables: asparagus, potatoes, cucumbers, carrots
- Refined grain products: white pasta, white rice, white bread
- Lean protein: fish, chicken, lean pork, eggs, tofu
Also Check: What Causes H Pylori Ulcers
What Is The Treatment For Peptic Ulcers
The choice of treatment depends on whether or not the ulcer is caused by infection with H pylori. Correct diagnosis is key to whether a treatment works or not. If the bacteria are the cause, treatment focuses on killing the infection. Regardless of whether the bacteria are the cause, reducing acid in the stomach is another important focus of treatment.
The following treatments are recommended for ulcers:
- Lifestyle changes: Quit smoking, avoid alcohol, aspirin, and NSAIDs
- Acid-blocking medications
- Medications that protect the lining of the stomach and duodenum
- Triple-therapy or dual-therapy regimens for ulcers caused by H pylori
No single medication works to get rid of H pylori infection. Two combinations have been found that work well in most people.
These treatments are generally given for two weeks.
Once H pylori bacteria are eradicated from a persons digestive tract, usually it will not come back. The ulcers usually heal completely and do not return.
Treatment for bleeding ulcers depends on the severity of blood loss and includes:
It is important to remember that treatment may not work if the diagnosis is not correct. If the doctor diagnoses an ulcer, it is important to determine whether the ulcer is caused by infection with H pylori.
Your Uc Flare Management Plan
Your doctor may help you deal with a flare by changing your medications or offering new ones. Treatment of flares can include mesalamine products and usually a steroid, such as prednisone,” says Desi.
There are also some things you can do at home to temper a flare. These include:
During an ulcerative colitis flare, its recommended that you schedule regular visits to see your doctor, at least once every three months until the symptoms go away. After the flare has subsided, physicians recommend one or two checkups a year to manage the disease.
When an ulcerative colitis flare strikes, you have options for getting your life back on track. Its important to learn what you can about maintaining your health and work with your doctor to find the best ways to safely control UC. And remember to always let your doctor know when new or persistent symptoms arise.
Also Check: Natural Cure For Peptic Ulcer