Whats The Connection Between Joint Conditions And Uc
When ulcerative colitis causes problems outside of the gut, its known as an , according to Arun Swaminath, M.D., chief of gastroenterology and director of the Inflammatory Bowel Disease Program at Lenox Hill Hospital in New York City. Joint pain is one of the most common extraintestinal manifestations when it comes to UC, says Dr. Swaminath. These joint issues can affect all the joints in your bodyor just a few. How often we see these issues with UC really depends on the patientif the ulcerative colitis is severe or complex, then we often see more joint pain.
The correlation between the severity of ulcerative colitis and the intensity of joint pain comes back to uncontrolled inflammation, which is at the root of both health issues. Because joint issues can be so common with UC, as specialists we are trained to ask our UC patients about joint problems, Dr. Swaminath says. And what we find is that if you fix the inflammation in the gut, many times, joint pain improves as well.
How To Manage Joint Pain When You Have Uc
If your joints are bothering you, getting your UC under control may be the best way forward, according to Michelle Keller, Ph.D., an assistant professor in the division of general internal medicine at Cedars-Sinai Medical Center in Los Angeles. In many cases, joint pain symptoms can decrease when UC is well-managed, she says.
In fact, before exploring the severity of symptoms and treatments for joint pain, Dr. Swaminath says most gastros will zero in on asking UC patients more questions about UC treatment first. For instance, your doctor may try to determine whether your IBD is no longer in remission, or whether your disease is being undertreated. They might also ask questions to suss out whether you are having a reaction to one of your ulcerative colitis meds, which is inadvertently causing joint pain, or whether your pain is related to a separate joint problem altogether outside of your UC.
If the answers indicate the ulcerative colitis is under control but joint issues persist, it may be time to bring in the calvary, says Dr. Keller. In cases where joint pain is still present even when inflammation of the intestine is resolved, you may need to work with a gastroenterologist and a rheumatologist to identify medications that can help, she says.
Be Diligent And Careful With Medication
A physician will usually prescribe an anti-inflammatory and medication to help with an overactive immune system with a diagnosis of ulcerative colitis. This medication is vital to fight off flare-ups and missing a dose can be a trigger all by itself.
When taking medication for this condition, it is always wise to consult a doctor. Certain over-the-counter medications, like NSAIDs, can exacerbate ulcerative colitis as well as cause other issues.
Recommended Reading: What Is The Best Medicine For Mouth Ulcer
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Complications Of Ulcerative Colitis
A severe complication of Ulcerative colitis is toxic megacolon. In this situation, the severity of the inflammatory process may reach the point where the neuromuscular function of the colon is disrupted. This leads to the dilation and perforation of the colon. This will often lead to the removal of the colon.
Pancreatitis, which can be acute or chronic in nature, may precede, occur with or be a complication of ulcerative colitis.
Less common complications involve the kidneys, lungs and vascular system.
- Kidney complications include renal insufficiency and nephrolithiasis.
- Lung complications include pulmonary vasculitis and pulmonary embolism.
- Vascular complications include venous thrombosis and pulmonary embolism.
Also Check: What Causes Diabetic Foot Ulcers
Believe It Or Not This Digestive Disorder Can Wreak Havoc On Your Elbowsand Knees Too We Asked The Experts For The Bottom Line
Bowel inflammation may be the main characteristic of , but joint pain is far more common than many people realize. According to the Crohns and Colitis Foundation, as many as 30% of people with UC and Crohns disease may also experience . Most of the time, UC causes joints to feel stiff without inflammation, but other times you may also experience inflammatory arthritis that includes swelling in areas where two bones join, such as your knees, elbows, or wrists. Arthritis that is associated with UC doesnt just target your large joints in your arms and legs, thoughit can also affect your spine.
The good news? Joint pain usually disappears once the inflammation in your colon is treated. Still, it can seem a bit confusing to be experiencing joint aches when youve been diagnosed with a gastrointestinal disorder. How does it all relate? We asked the experts to break down the ways ulcerative colitis and joint pain are related.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove some or all of your bowel may be an option.
During surgery, your small intestine can be diverted out of an opening in your abdomen known as a stoma. This type of surgery is known as an ileostomy.
In some cases, the stoma is only temporary and can be closed up once your bowel has healed.
Read Also: How To Stop Ulcer Pain Instantly
What Does A Uc Cramp Feel Like
People who have UC describe a pronounced sensation of squeezing and releasing in their abdomen, Dr. Ha says, that feels more like pressure than a stabbing pain.
Doctors diagnose UC based on where symptoms are occurring. Many people with the condition experience whats known as left-sided colitis, where the pain and inflammation occur on their left side, from the rectum up to the descending colon.
Cramps can also be accompanied by bloating and gas, which cause a feeling of pressure and knotting in your abdomen.
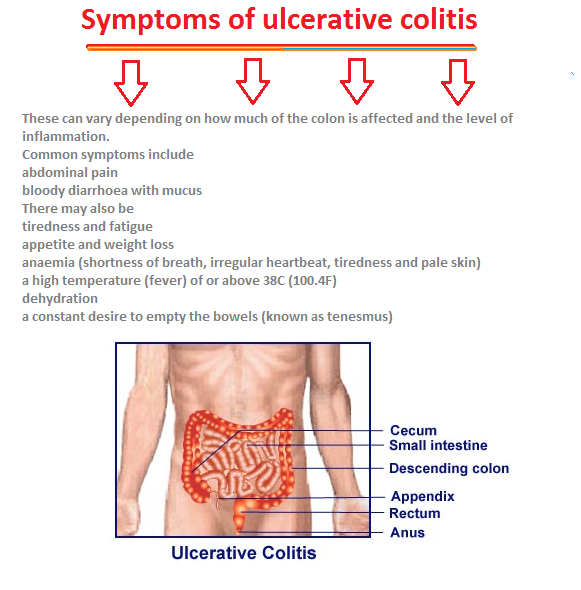
Other Ulcerative Colitis Symptoms
Ulcerative colitis causes rectal and abdominal pain, but its not the only condition that does . UC pain is chronic, meaning its either continuous or flares up repeatedly over time.
Chronic gut pain isnt the only symptom of UC though, and if youre experiencing it with the following seek out a medical professional:
- A noisy/rumbling gut
Don’t Miss: Cheap Ulcer Treatment For Horses
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Pain No More: The Pill That Can Prevent Ulcerative Colitis Flare
According to the CDC, an estimated 3.1 million adults in the United States have been diagnosed with inflammatory bowel disease , which includes Crohns disease and ulcerative colitis.
Although Ulcerative colitis and Crohns disease can be managed, there is currently no cure. Many people with the complex condition are plagued by persistent inflammation of the lower intestine and pain.
Ulcerative colitis and Crohns disease can affect people in different ways. For some the pain may be continuous, for others, its mild unless theres a flare-up.
Some people with ulcerative colitis will find that it gradually develops, while others are hit with full force immediately. However, one drug is showing promise for those living with ulcerative colitis and Crohns disease.
You May Like: Best Otc Probiotic For Ulcers
What Is Life Like With Ulcerative Colitis
The only cure for ulcerative colitis is complete surgical removal of the colon. However, most patients will not require surgery to have their symptoms under control, and some patients may have complications after the surgery such as pouchitis. Whether they require surgery or not, our goal is to allow our patients to live a full and productive life with ulcerative colitis. Most patients will require medications for an indefinite period of time. Research has shown that patients with ulcerative colitis who do not take their medication, even if they are feeling well, are more likely to have a return of their symptoms compared to patients who continue their medications. It is very important that patients discuss with their doctor if they are considering stopping their medications.
It is important for patients with ulcerative colitis, even if they are feeling well, maintain regular visits with their physician. For example:
- Patients on medications may need routine blood work to monitor for side effects.
- Patients with ulcerative colitis should keep up to date on immunizations including influenza , pneumococcal , human papilloma virus , and hepatitis A and B.
- Some patients with ulcerative colitis, particularly those who have had been exposed to steroids , may need to have bone mineral density tests to screen for early osteoporosis.
- Patients with ulcerative colitis will need to have colonoscopies to screen for colon cancer.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis

Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Recommended Reading: How To Gain Muscle With Ulcerative Colitis
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK
Put Together An Emergency Kit
Having an emergency kit is important as it can help you avoid embarrassing situations, especially when you are at work or school. You can include items such as underwear, pants, deodorizer, and baby wipes in this kit to help you in most situations.
You may never use this kit, but just having it may bring some mental relief, which can help reduce overall stress and pain levels.
Ulcerative colitis pain is a complex disorder. What techniques or strategies do you use to manage ulcerative colitis pain when a flare-up happens?
Don’t Miss: How Do You Heal A Bleeding Ulcer
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
What Kind Of Diet Is Helpful For Living With Colitis
Your healthcare provider may suggest one or several of these diets, depending on the type of colitis you have and the condition youre in:
- Low-residue diet. A low-residue diet is easy to digest when your symptoms are acute or severe. It limits fiber and fat and emphasizes soft, well-cooked foods. If you have a temporary infection or radiation colitis, your healthcare provider may recommend a low-residue diet.
- Anti-inflammatory diet. To keep chronic inflammation low, your healthcare provider might recommend you avoid highly inflammatory foods, especially fast and processed foods high in sugar and fat. They might suggest more healthy, unsaturated fats to calm inflammation like olive oil, avocados, nuts and oily fish.
- Elimination diet. If you have an inflammatory bowel disease, your healthcare provider will likely recommend an elimination diet to isolate the foods that cause your symptoms to flare up. An elimination diet eliminates certain types of foods and then adds them back in a systematic way so that you can observe how your gut responds to them. After the temporary elimination diet, you can use what you learned to design a personalized, long-term maintenance diet.
A note from Cleveland Clinic
Last reviewed by a Cleveland Clinic medical professional on 06/22/2022.
References
Read Also: Can You Take Tylenol With Ulcerative Colitis
Read Also: Is Ensure Good For Ulcerative Colitis
What Are The Complications Of Ulcerative Colitis
Colon Cancer
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Skin
Other Complications
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
Recommended Reading: Ulcerative Colitis Treatment For Flare Up
Whats A Good Plan To Manage Uc Cramping
Monitor your medications. Talk to your doctor about any prescription, over-the-counter, or herbal medications youre taking. Iron deficiency is common with UC, but oral iron supplements have been shown to increase the risk of inflammation and cramping. Some antibiotics and pain relievers, such as ibuprofen, may also increase flare-ups and cramping.
Review your diet.Keep a food diary and note the connection between the foods you eat and your UC symptoms. In general, its smart to stay away from processed foods and those high in saturated fat and sugar. High-fiber foods and dairy products can also cause UC cramping, but check with your doctor before eliminating foods from your diet, to ensure youre getting the nutrients you need.
Eat frequent, small meals. Instead of two or three large meals, eat four to six smaller meals spaced more closely throughout the day. Also, take your time while eating and chew thoroughly.
Skip caffeine and carbonated drinks. Caffeine can cause gas, intensifying abdominal cramping. It is also a stimulant, which can make cramping and diarrhea worse.
Drink enough water. People with UC may be at increased risk of dehydration, so be sure to drink plenty of H2O. A good rule of thumb, according to the Crohns and Colitis Foundation, is to aim for about 64 ounces or eight 8 oz glasses per day.
Read Also: Best Meds For Ulcerative Colitis