Vegetables For Ulcerative Colitis: The Bottom Line
Vegetables are worth eating if you have ulcerative colitis, but its important to find options that work with your GI tract and dont trigger symptoms. Soft-textured vegetables that are higher in soluble fiber and lower in insoluble fiber are often more easily tolerated, especially during a flare-up.
If youre having trouble finding vegetables that work for you, talk with a registered dietitian specializing in ulcerative colitis or inflammatory bowel disease. They can help determine how much fiber and what choices are best for each patient, Leben says.
Dietary Fibre A Definition
According to the American Association of Cereal Chemists , dietary fibre is the edible parts of plants or analogous carbohydrates that are resistant to digestion and absorption in the human small intestine, with complete or partial fermentation in the large intestine. In compliance with this definition dietary fibre includes non-starch polysaccharides and resistant oligosaccharides , analogous carbohydrates , lignin, and substances associated with the non-starch polysaccharide and lignin complex in plants . The Codex Alimentarius Commission definition from 2009 is that dietary fibre means carbohydrate polymers with three or more monomeric units, which are neither digested nor absorbed in the small intestine of humans and this is the main, current, operative definition ofdietary fibre around the world . It is worth mentioning that there are many other, considered definitions, and lately Jones made a concentrated review of the literature on this topic.
Reducing Fiber During A Flare
If fiber seems to worsen your symptoms, you may consider switching to a low fiber diet during a flare. Eating less fiber can help reduce the frequency of your bowel movements and the amount of stool you pass, according to the National Health Service.
You may want to steer clear of the following fiber-rich potential trigger foods during a flare:
- fruits with skin and seeds
- raw green vegetables
- cruciferous vegetables
You can also try different techniques to make fiber easier to digest or reduce the amount of fiber in a food. The Crohns and Colitis Foundation recommends cooking veggies until theyre tender, peeling fruits and veggies, and discarding seeds to help cut back on insoluble fibers.
Eliminating nutrients from your diet can have a negative impact on your health. Consider working with a doctor or dietitian to make sure a low-fiber diet is safe for you.
Recommended Reading: Herbal Treatment For Ulcerative Colitis
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
Eat In: Ulcerative Colitis Meal

When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
You May Like: Foods That Heal Ulcers And Gastritis
How Can I Eat Healthy On A Low
Start thinking in terms of roughage versus fiber. Think of the texture of the food when you swallow it. If the food is soft or pureed, then its low roughage. If its tough and coarse, then its high roughage.
Some high-fiber foods are low roughage. For example, an avocado has a lot of fiber, but its not rough. Usually people on low-fiber diets eat avocado without an issue. Same idea with nut butters. Whole nuts, such as almonds, are high roughage, but creamy almond butter is low roughage.*
Examples of low-roughage foods that have fiber:
- Fruit without tough skins and seeds: Banana, avocado, cantaloupe, peeled apple, and peeled and seedless cucumber
- Well-cooked vegetables without tough skins, seeds or stalks: Peeled and cooked winter squash, carrots, parsnips, potatoes without skin, sweet potatoes without skin, yams without skin, turnips
- Creamy nut and seed butters: almond butter, peanut butter, tahini
*Foods can upset people for reasons other than fiber. Work with your GI dietitian to identify safe foods.
Can Food Cause Crohns Or Colitis
We dont know what causes Crohns and Colitis but we do know that a combination of the following factors are likely to play a part:
- A problem with the immune system, where the body attacks its own cells
- Changes in the bacteria in the gut.
These, together with environmental factors, like food and stress, may trigger the conditions.There isnt any clear evidence that specific foods cause Crohns or Colitis. Some researchers think a diet low in fruit and vegetables may increase the risk of Crohns and a low intake of vegetables may increase the risk of Colitis for some people. Theres also some evidence that eating a lot of meat or table sugar, called sucrose, may increase the risk of Crohns and Colitis. But there isnt enough evidence yet to say for certain whether food affects the risk.
Dont Miss: How To Treat Mouth Ulcers
Also Check: How To Treat Hindgut Ulcers In Horses
Why Are People With Crohns And Ulcerative Colitis Told To Avoid High
If dietary fiber is so good for us, why is a low-fiber diet recommended for people with Crohns and ulcerative colitis?
1. Certain high-fiber foods can worsen gastrointestinal symptoms, including gas, bloating, abdominal cramping, diarrhea and constipation.
2. Foods high in roughage can irritate the bowel thanks to their coarse nature. Imagine rubbing sandpaper on an open wound. Ouch! Roughage includes thick skins and stalks of fruits and vegetables, whole nuts and seeds, and popcorn.
3. Roughage can lead to bowel obstructions in at-risk individuals. People most likely to obstruct include those with a prior history of abdominal surgery and/or stricturing Crohns disease.
Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
Also Check: Foods To Avoid With Peptic Ulcer
Also Check: What Does Venous Stasis Ulcer Look Like
Not A Substitute For Conventional Drugs
Seidner says the supplement isnt intended to replace prescription drugs. Generally speaking, individuals do need medication to maintain their disease in remission, he says.
This product is meant to be a complement to standard medical therapy, Seidner continues. People may be able to take a little less medication as a result of this. We dont want people to stop taking their pills.
His study notes that corticosteroids, such as prednisone, are highly effective in moderate to severe ulcerative colitis. Unfortunately, adverse effects are a concern and more than a quarter of patients will relapse when corticosteroid treatment is discontinued, the study notes.
The supplement is a drink containing omega-3 fatty acids from fish oil soluble fiber, which produces short-chain fatty acids and antioxidants. The ingredients were chosen to fight inflammation and improve nutrition.
The supplement is meant to replace a portion of daily calories. If someone were to take the supplement without decreasing their food calories, they would definitely get fat, says Seidner.
For six months, patients ate one-third fewer calories in order to drink about two daily 8-ounce cans of the supplement or placebo . Otherwise, they were told to follow their normal diet.
Supplement and placebo patients had a similar improvement in symptoms, such as stool frequency and rectal bleeding. But the supplement group was able to reduce their need for prednisone much more than the placebo group.
What To Eat During A Flare Up
It may be best to avoid more fibrous foods like whole grains, greens, and nuts when youâre having a flare up. Instead, look for easy-to-digest foods like:
- Refined breakfast cereals like cornflakes
- White rice instead of harder-to-digest brown or wild rice
- Low-fiber fruits like bananas, cantaloupe, honeydew melon, and cooked fruits
- Fully cooked non-cruciferous vegetables like asparagus tips, potatoes, squash without the peel, seeds, or stalks
- Refined, low-fiber pasta and noodles
- Lean meat and fish
For some people with UC, it also helps to break meals up into five or six smaller meals instead of three larger ones. You can talk to your health care team about going on an elimination diet. Thatâs when you stop eating different foods one at a time to see which ones tend to cause symptoms so you can remove them from your diet. Itâs important to work with your doctor or dietitian when you do this to make sure you get enough nutrients.
If you find that you are losing weight during a flare up, talk to your health care team. They might need to test to see if youâre getting enough of certain vitamins and minerals. They also may be able to help you zero in on foods that worsen your symptoms and help you replace them with healthy alternatives that will help you maintain a healthy weight. These might include some of the foods above, like bananas, eggs, lean meat, and noodles.
Recommended Reading: What Are The Signs Of Having A Stomach Ulcer
What Blender Is Best For Making Smoothies
For most people, any old blender will do. But, if you have GI symptoms or plan to add whole nuts, seeds, or raw fruits or vegetables with thick skins and/or seeds then you might need a high-speed blender. A high-speed blender, like a Vitamix, will really pulverize those tough-to-digest nuts, skins, and seeds.
Americas Test Kitchen tested several mid-priced blenders to see how they make smoothies and crush ice, among other functions. The winner was Brevilles Fresh & Furious. Smoothies are very smooth, and theres even a dedicated green smoothie button that completely blends fibrous ingredients into a silky smooth drink. Perfect for someone with an inflamed gut! Plus, its reasonably quiet and compact.
If you dont have a heavy duty blender then stick to blending softer fruits, vegetables and smooth add-ons, like nut butters versus whole nuts.
How To Add Fiber To Your Uc Diet
There are ways to make fiber easier to digest or reduce the amount of fiber in a food, while still getting some of that fabulous fiber into your belly. The Crohns and Colitis Foundation recommends cooking your veggies until theyre tender, always peeling your fruits and veggies, and removing the seeds to help cut back on the insoluble fiber. A fiber supplement like Bonny is another gentle and easy way to add fiber to your diet.
Before adding or reducing fiber in your diet, its always a good idea to check in with your doctor or dietician.
You May Like: Interesting Facts About Ulcerative Colitis
How Does The Low Residue Diet Work
The daily recommended amount of fiber that people should ideally consume is about 25 to 38 grams. However, this may not be right for people with IBD. A higher fiber diet should be avoided for people undergoing bowel surgery or if experiencing a flare of IBD symptoms.
When following a low residue diet, typical advice is to consume no more than 10 to 15 grams of fiber a day.
You should also avoid dairy products and certain types of carbohydrates. They may provoke abdominal cramping and diarrhea.
A healthcare professional or dietitian should supervise you if you decide to follow a low residue diet. Low residue diets are usually only recommended for short-term use.
It can also change the gut microbiome. Your individual needs should determine the amounts and types of food, as well as how long you follow the diet.
This diet is usually not followed long term.
These are general guidelines for a low residue diet. They can be changed based on how your body reacts to the diet and what your healthcare team recommends.
There are many healthy food options on a low residue diet. Its a good idea to talk with a dietitian before starting this type of diet, but here are some good options they may suggest:
Good cooking methods for a low residue diet include:
- prune juice or juice with pulp
Low residue foods should be well cooked. Avoid cooking methods such as roasting, broiling, or grilling, which may make food tough or dry.
Ulcerative Colitis Diet Tips
Its not always easy to know which foods will be best for your ulcerative colitis, but your diet and nutrition are a huge part of managing your ulcerative colitis. Even though it can feel like your diet is restricted when you have been diagnosed with ulcerative colitis, you still need to eat a large variety of foods to get all those necessary nutrients, like fiber.
Foods high in insoluble fiber are indeed a potential trigger for ulcerative colitis. But there are two types of fiber:insoluble fiber and soluble fiber. Soluble fiber dissolves in water and your GI fluids, while insoluble fiber remains unchanged as it moves through your GI tract. Soluble fiber might be more beneficial for people with an inflammatory bowel disease like ulcerative colitis.
Some research shows that fiber might help extend periods of ulcerative colitis remission and offer other benefits, like reducing blood pressure, reducing cholesterol, regulating blood sugar, boosting immunity, and helping with weight management.
Read Also: How Do Ulcers Feel Like
Choose Fish With Omega
Scientists have not yet come to a consensus about whether or not eating red meat has any effect on people with UC, but the nutrients in fish could be beneficial. Consuming foods like fatty fish, which are rich in omega-3 fatty acids, may help with UC-related inflammation, says Diekman.
Omega-3 fatty acids are a crucial nutrient your body uses to make cells and hormones that regulate blood clotting. While some studies have shown that omega-3 fatty acids are anti-inflammatory, more research still needs to be done to prove theyre beneficial. According to the National Institutes of Health , omega-3 fatty acids, like probiotics, also support the immune system.
Unlike other fats, the body cant make this good fat on its own from other raw materials. Instead, you must get it from food sources, including fish like salmon, herring, sardines, rainbow trout, and mackerel just refrain from frying fillets, since fatty or greasy foods can exacerbate UC symptoms.
Also remember that its especially important to make sure youre eating enough protein immediately after a flare-up to replace any lost nutrients and reduce the risk of anemia.
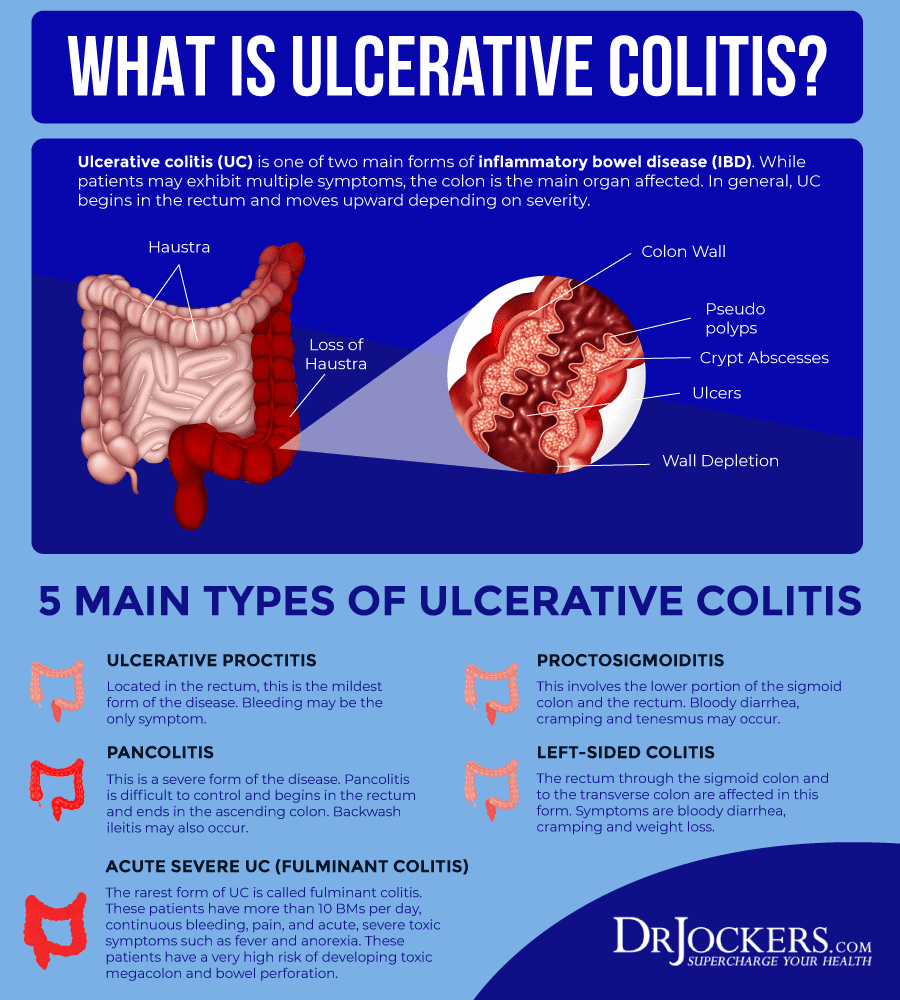
What Causes Ulcerative Colitis
The same environmental factors that contribute to disease onset can also cause debilitating flares.
Certain medications, like antibiotics and non-steroidal anti-inflammatory drugs, are known to increase disease risk and trigger flares. But be careful, abruptly stopping any medication may also lead to a flare. Only do so under a doctors approval.
Stress is also thought to be a major contributor, as well as diet .
In particular, research has linked excessive use of sugar and artificial sweeteners to IBD, but other studies have shown no connection .
Some research has also shown a strong link between animal protein and IBD risk.
For example, in an observational study of more than 67,000 middle-aged French women, those who frequently ate meat and fish were significantly more likely to develop IBD. Eggs and dairy were not linked to increased risk .
Summary: A combination of genetic, environmental and immunological factors contribute to ulcerative colitis risk. Symptoms occur in flares and include digestive complaints, as well as fatigue and fever.
If you would like more information on how to eat for Ulcerative Colitis, which involves what we call a low FODMAP diet, tap the button below to download our Eat This, Not That list as well as additional resources for Ulcerative Colitis
SEND ME THE LIST
Recommended Reading: Enema Medication For Ulcerative Colitis
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.