What Are Nursing Home Bedsores
Bedsores, also called pressure sores or pressure ulcers, are skin tissue injuries caused by pressure that happens over a period of time. They mainly occur in people who are unable to move around well on their own and spend most of their time in a bed, chair, or wheelchair especially nursing home residents with mobility problems.
It is important to take steps to prevent bedsores in nursing homes and seek treatment if any develop. While most nursing home bedsores heal with treatment, they can cause life-threatening health risks without prompt medical attention.
Nursing home staff are trained to prevent bedsores, so residents who develop them could be victims of neglect or abuse. In these cases, a nursing home abuse lawyer can help. These specialized attorneys can help you get money from the nursing home and staff members responsible for the bedsore.
Adherence With The Clinical Interventions
The reported all-or-none adherence to the bundle was 16%, although this varied throughout the 9 weeks . The reported adherence to the individual elements also varied: adherence was 75% to the repositioning element 22% to the support surfaces element and 21% to the skin inspection element. The reasons for non-completion were rarely documented.
Figure 1
Pressure Ulcer Prevalence Varied By Age Sex And Length Of Time Since Admission To The Nursing Home But Not By Race
Residents aged 64 years and under were more likely than older residents to have pressure ulcers . Pressure ulcers were more common in males than in females . Residents in nursing homes for 1 year or less were more likely to have pressure ulcers than those with a longer length of stay . There was no significant difference between white and nonwhite populations with respect to having pressure ulcers.
Also Check: Icd 10 Stage 4 Sacral Ulcer
Causes Of Bedsores In Nursing Homes
In many cases, bedsores in nursing homes are the result of nursing home abuse and/or neglect.
The Mayo Clinic has identified a few common ways in which bedsores develop, which all involve the interruption of blood flow to the skin.
Bedsores may form due to:
Treatment Of Bedsores In Nursing Homes
Treating nursing home bedsores may be done by a general health care provider or wound care team, depending on the bedsore stage.
Treatment may include:
Nursing Home Holiday Visits & COVID-19
The holidays can be a great time to connect with older loved ones who may be living in nursing homes. However, with the COVID-19 pandemic and the threat of a new variant its key to take precautions so your loved ones arent put at risk. Learn how you can safely celebrate the holidaysRead More
What Percentage of Elder Abuse Is Done by Family Members?
Family members commit elder abuse in nearly 6 out of 10 cases, according to the National Council on Aging . Other studies found that family members are the most common perpetrators of nearly every type of elder abuse. Learn how to keep an older person you love safe. Family and the Problem of Elder AbuseRead More
Delta Variant Leads to Uptick in Nursing Home Deaths
After a spike in COVID-19 cases attributed to the Delta variant caused thousands of deaths in nursing homes over the summer, its important to focus on how to protect yourself and your loved ones living in long-term care facilities. COVID-19 poses a higher risk to nursing homes as residents often share living spaces and haveRead More
Nursing Home Abuse Justice sheds light on the dangers of nursing home abuse. It provides reporting that exposes truths previously hidden.
You May Like: Low Residue Diet For Ulcerative Colitis
Giving Staff The Right Level Of Knowledge
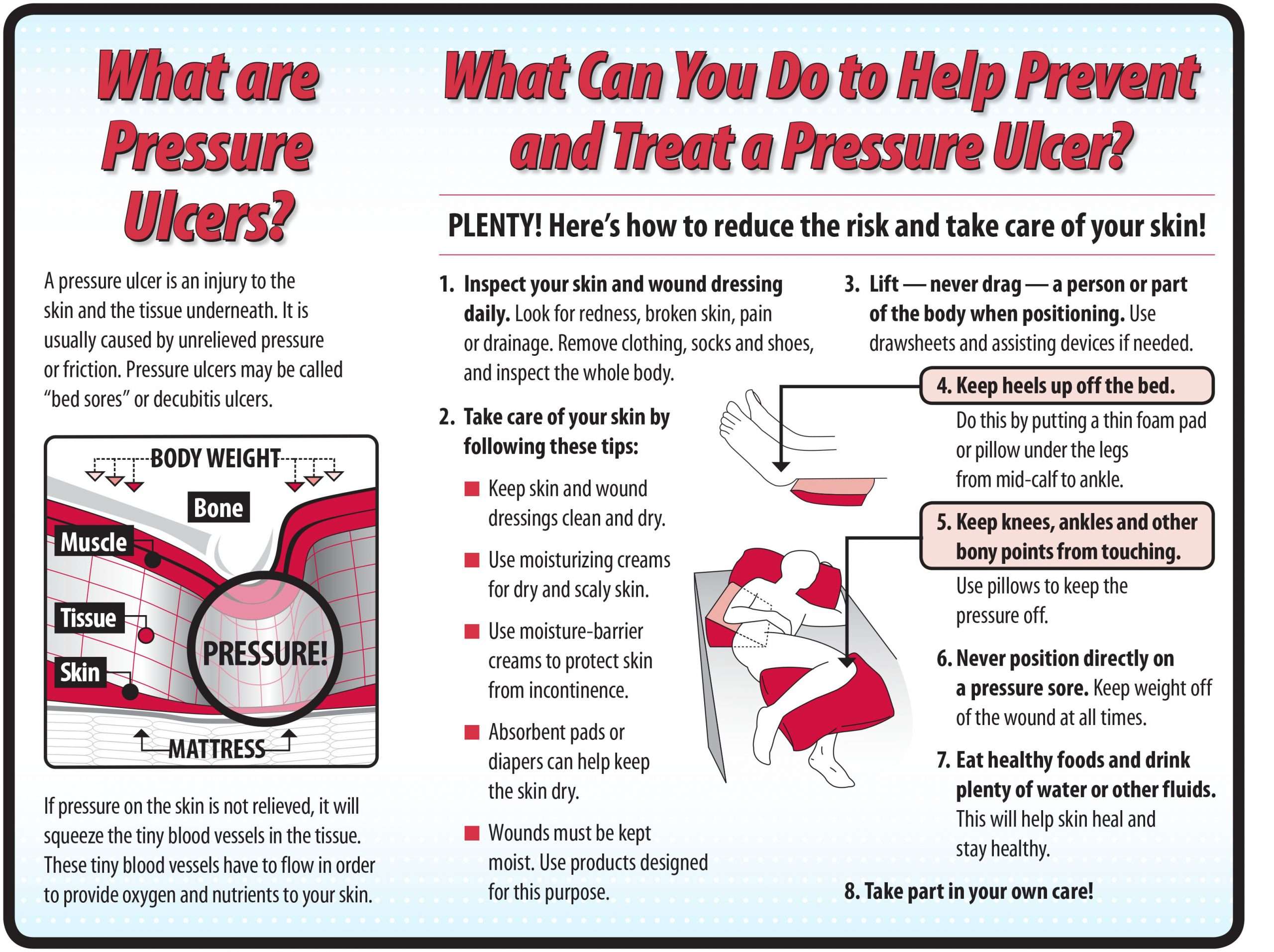
Ensuring staff have the right level of knowledge on pressure ulcers in key. They need to know how pressure ulcers develop and who is most at risk. This involves understanding how to assess patients and what measures they can take to reduce the risk.
A recent Scottish initiative has developed some very useful tools and resources designed specifically for the care home sector . These resources concentrate on recognising a pressure ulcer, reporting a pressure ulcer and how best to respond to the situation.
Bedsore Causes In Nursing Homes
Bedsores Caused by Nursing Home Neglect
Quick Answer
A 2019 report by the Sun Journal details elders’ experiences in a Lewiston, Maine nursing home, specifically describing one resident’s death, which was attributed to a stage 4 bedsore. Sadly, this is not an isolated incident. Many underlying bedsore causes stem from nursing home neglect. Too often, nursing home residents suffer from preventable bedsores due to poor or improper care from staff members.
Read Also: Can Stomach Ulcer Cause Fever
First Cycle Of Unfreezing: Planning
In this stage, there were some activities to come up with a preliminary diagnosis of the problem, gather data, and giving feedback on the results and the plan for action. The first author and the trained research assistant met several key people including the in-charge and experienced HWs or nurses selected by the in-charge of each NH to learn the issues relevant to pressure ulcers in their homes. They reported on the existing PUs but did not have record of the incidence of PUs. The prevalence of PUs in these four homes ranged from 8 to 10%. Overall, the residence-staff ratio was around four to six. The turnover rate of care staff was acceptable, although this sometimes affected the care that was delivered. They agreed that the occurrence of PUs was an important issue in their homes, and efforts e.g., having a prevention protocol and training to care staff should be made to decrease them.
Complications From Nursing Home Bedsores
- Infections: Infected bedsores can cause fever, chills, confusion, racing heart, and weakness. Infections from nursing home bedsores can also make their way into joints and bones, damaging cartilage and tissue. Others may develop cellulitis, an infection of the skin and soft tissue that causes warmth, redness, and swelling.
- Cancer: Some wounds that do not heal can lead to squamous cell carcinoma, a type of skin cancer.
- In very severe cases, nursing home bedsores can turn into sepsis. This is a potentially life-threatening condition that occurs due to an existing infection.
Nursing home staff members know how to treat bedsores before they cause serious health problems. If the staff members fail to do so, they should be held legally responsible for any complications that a resident develops from a bedsore.
In 2019, the family of a woman who developed a serious bedsore in a hospital was awarded $5 million in a jury trial. The family claimed the hospital failed to prevent the bedsore, causing the woman to suffer greatly in the last months of her life.
Don’t Miss: Surgical Management Of Ulcerative Colitis Ppt
Icipant Responsiveness To The Care Bundle
I don’t think there’s anything in that training that could make you use them more effectively, you just live and learn. You’ve just got to get used to them I think. .
Initially, the participants were unfamiliar with how to use the bundle and found it to be time-consuming. However, they explained that the time required to complete the bundle decreased with increased familiarity and one participant reported having more time with the residents as a consequence of using the bundle. Despite the low adherence to the whole bundle, the participants reported that the bundle was straight forward to use. Therefore the issues with adherence may have been related to documentation, as highlighted above.
you’re making your colleague aware that you’ve seen something because what sees, I might not have seen that day.
You can go and find this you can tick are they red? Yeah tick such a body is red and we know about it and we’ve been actively doing something about it. So I think we do need that on the back. .
continence care
I think if it was simplified, people are more likely to pay a bit more attention to what they’re ticking!
Prevention Of Pressure Ulcers In Nursing Home Residents
Alica Bangova Clinic nurse, University College London, Royal Free Campus, Medical School, National Amyloidosis Centre, London.
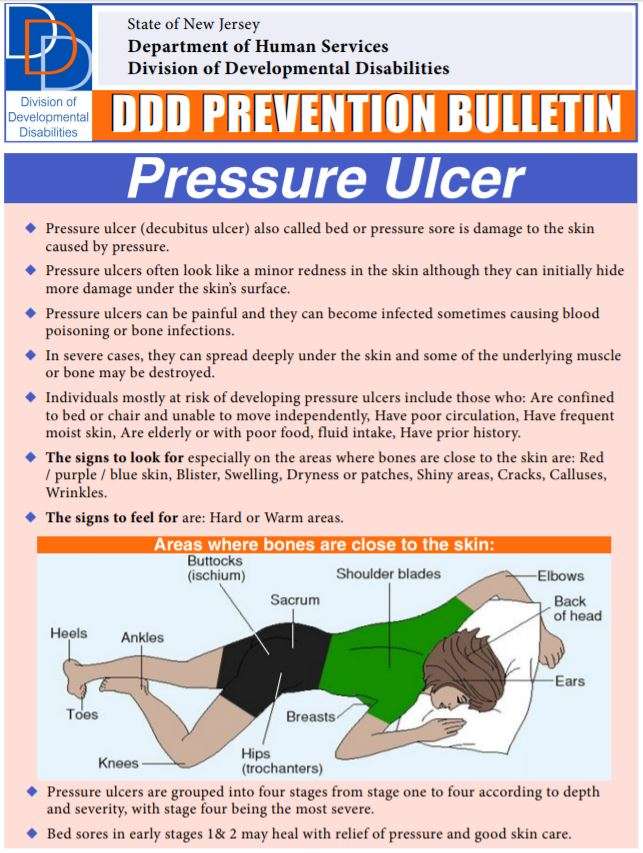
Pressure ulcer prevention strategies are applicable to all anatomical sites however, the main focus of this article is heel ulceration in the nursing home setting. The thinness of the subcutaneous tissue between the skin and bone, and the propensity for lower limb diseases, makes the heel the second most common site for pressure ulcer development. This article provides a review of the effect of education and knowledge on the prevention of heel pressure ulcers in nursing home residents. Where there is paucity of evidence, pressure ulcers in general will be examined.
Nursing Standard.27, 24, 54-61. doi: 10.7748/ns2013.02.27.24.54.e7243
Peer review
Read Also: Venous Leg Ulcer Dressing Treatment
Why Does Incontinence Increase The Risk Of Pressure Ulcers
Schenk:With regards to incontinence, why is that kind of like a danger zone in itself?
And then you think about feces, for example, have acidity in it. Its coming from our stomach or from our colon. It alters the skins pH, the bacteria in our stool can also decrease the skins resistance to not break down.
And so its interesting because its 2019, which is super fun. Were living in a fun age in the medical arena, because there are so many great products on the market now. For example, theres a company that developed a barrier wipe, essentially. Its synthetic. It goes on the skin, stays in place for up to seven days, but it allows sweat and moisture to come through it. It doesnt allow urine or feces to get to the skin. And thats groundbreaking. Additionally, there are some overlay mattresses, a device that you put on top of a mattress thats powered, theres a fan, and it evaporates the moisture on our skin, even if were a heavy wetter. It evaporates in a matter of minutes so that urine or liquid feces is not staying next to our skin. The challenge is some of these products are new and theyre not well recognized yet in the medical industry, but they do exist.
Smith:Yeah, I think that on our podcast, we talked about one time this new fabric technology. There are new sheets that they have that cut down on sheering. Its amazing, but not widespread at all.
Bedsores In Nursing Homes
According to the Centers for Disease Control and Prevention , bedsores occur in more than 1 in 10 residents in nursing homes. If left untreated, bedsores can be deadly. Since bedsores can often be prevented with proper care, they may be a sign of nursing home abuse or neglect. You can pursue financial compensation for bedsores by filing a nursing home abuse lawsuit.
You May Like: Budesonide Vs Prednisone For Ulcerative Colitis
Incidence Mortality And Costs
The incidence rates of pressure ulcers vary greatly with the health care settings. The National Pressure Ulcer Advisory Panel says the incidence ranges from 0.4 percent to 38 percent in hospitals, from 2.2 percent to 23.9 percent in skilled nursing facilities, and from 0 percent to 17 percent for home health agencies. There is ample evidence that the majority of pressure ulcers occur relatively early in the admissions process. For patients in the hospital, they can occur within the first 2 weeks. With the increased acuity of elderly patients admitted and decreased lengths of stay in hospital, new data suggest that 15 percent of elderly patients will develop pressure ulcers within the first week of hospitalization. For those elderly residents admitted to long-term care, pressure ulcers are most likely to develop within the first 4 weeks of admission.
Mortality is also associated with pressure ulcers. Several studies noted mortality rates as high as 60 percent for older persons with pressure ulcers within 1 year of hospital discharge., Most often, pressure ulcers do not cause death rather the pressure ulcer develops after a sequential decline in health status. Thus, the development of pressure ulcers can be a predictor of mortality. Studies further suggested that the development of skin breakdown postsurgery can lead elders to have major functional impairment post surgical procedure.
Prevention Of Bed Sores In Nursing Homes
Steps for Preventing Bedsores
Preventing a bedsore is much easier than treating an existing one. However, a bedsore can still develop even when providing appropriate preventative care on a consistent basis. There are well-established protocols and strategies for providing care to patients with a high propensity of developing a bedsore at home, in a hospital or medical facility.
Bedsores PreventionBedsores are caused by compression of the skin, usually over bony prominences. These areas could include on the ankles, hipbones, tailbone, knees, ankles, elbows, shoulder blades, back of the head and other areas. The compression restricts adequate blood supply to tissue, which can begin to die from lack of oxygen within just a few hours.
Repositioning the individual is a key component to preventing the development of a bedsore. However, position changes need to happen frequently, to minimize any stress on the skin. In addition to repositioning the body to minimize pressure on highly susceptible areas, other effective strategies can help. This includes providing good nutrition and hydration, routine movement when possible, and smoking cessation .
Usually, the patients most susceptible to developing a decubitus ulcer are those challenged with mobility. This could include patients confined to a bed, wheelchair-bound due to a medical condition, paralysis or in a coma.
Steps for the Wheelchair-Bound to Prevent Pressure Wounds
Wound Care Prevention Steps for the Bed Bound
Read Also: Can You Get An Ulcer In Your Intestines
Implementing A Prevention Plan
Preventing pressure ulcers can be nursing intensive. The challenge is more difficult when there is nursing staff turnover and shortages. Studies have suggested that pressure ulcer development can be directly affected by the number of registered nurses and time spent at the bedside., In contrast, however, one recent study suggested that there was no correlation between increasing the nurse-to-patient ratio and the overall incidence of pressure ulcers. Donaldson and colleagues noted that this particular study was limited by the fact that the researchers could not affirm compliance with ratios per shift and per unit at all times. Given that the cost of treatment has been estimated as 2.5 times that of prevention, implementing a pressure ulcer prevention program remains essential.
A key component of research studies that have reported reduction of pressure ulcers is how to sustain the momentum over time, especially when the facility champion leaves the institution. It is clear from the evidence that maintaining a culture of pressure ulcer prevention in a care setting is an important challenge, one that requires the support of administration and the attention of clinicians.
Ensure The Patient Receives Proper Daily Nutrition
Before becoming an attorney, I never understood the relationship between nutrition and skin health. However, after witnessing senior citizens experience the terrible repercussions associated with malnourishment, I quickly recognized that our elderly must maintain a proper diet. When our seniors are placed in nursing care, the facility becomes responsible for the patients caloric, vitamin, mineral, and fluid intake. If one of our loved ones does not receive enough food, nutrients, or fluids, the skin can quickly breakdown. Therefore, ask lots of questions about what your loved one is being fed, how often, and with what frequency his mineral levels are being checked.
Recommended Reading: Ulcer On Eye From Contact Lens
Study Design And Setting
Institutional based cross-sectional multi-center study using quantitative method was conducted from August 1322, 2018. Thera are 10 public hospitals functional in Wollega zones. The study setting includes five public hospitals including one teaching hospital , five Public Referral Hospitals: Nekemte, Gimbi, Nedjo, and Shambu Referral hospitals. Among ten hospitals, the investigators purposively selected five hospitals where large number of patients visit, referred and admitted. Wollegas main town is 330km to the west from the capital city of the country, Addis Ababa, Ethiopia. .
Swedish missionaries introduced the modern nursing to Ethiopia around 1866. Then, Russia and French were delivering the nursing service in limited areas of Ethiopia. After the Second World War , the Ethiopian Red Cross Society established the first nursing school in at Haile Selassie I hospital. Swedish Missionaries at the Princess Tsehai Memorial Hospital opened the second nursing school. These two nursing schools were only admitting females to train in nursing profession. Males were admitted to nursing programs in 1954 in Ethiopia in Nekemte nursing school found in the current study area, Wollega zones. Currently, in Ethiopia nursing profession could be educated after completed grade ten or twelve .
Nursing Homes Pressure Injury Information
This page is intended to provide information to assist nursing home staff to prevent and reduce the number of pressure injuries in nursing homes.
Background Information
In April, 2016, the term pressure injury replaced pressure ulcer in the National Pressure Injury Advisory Panel Pressure Injury Staging System. The NPIAP notes that the change in terminology more accurately reflects pressure injuries to both intact and ulcerated skin. “The NPIAP is an independent not-for-profit professional organization dedicated to the prevention and management of pressure injuries. Formed in 1986, the NPIAP Board of Directors is composed of leading experts from different health care disciplines all of whom share a commitment to the prevention and management of pressure injuries.”
According to the NPIAP, pressure injury, also known as pressure ulcer, pressure sore, decubitus ulcer or bed sore, is localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful and injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear.
Medicare.gov/Nursing Home Compare
MetaStar
Survey Process
- If the facility received a deficiency for pressure injuries.
- Whether the facility has any patterns of repeat deficiencies.
- Results of the last standard survey.
Regulations and Violations
Also Check: Does Stomach Ulcer Cause Pain