Better Target Range Less Dementia Risk
The study found a strong link with the amount of time a patients INR was in a target range and the likelihood of developing dementia. While this can’t prove cause and effect, the researchers did find a strong correlation. Those who had an INR in the target range more than 75 percent of the time were four times less likely to develop dementia than those in the target range only 26 to 50 percent of the time.
“What we found is, if you can have a reliable, predictable level of Coumadin in the blood, the risk of dementia is quite low,” Bunch says. He followed the patients for five years, and then did an estimate or projection for an entire decade. “From the data, the projected risk of dementia with very well-controlled Coumadin was less than 3 percent at 10 years,” Bunch says.
He found an increased risk of dementia not just when blood levels were below the target. There was also a suggestion of increased risk when the blood level is too high, particularly in patients over 80 yrs old. If the blood level is too low, there is a danger of developing blood clots, which increase the risk of strokes, experts know. However, if blood levels are too high, there can be brain bleeds, which can also compromise the brain.
“The study doesn’t suggest we need more blood thinning,” Bunch says, “but that we need more effective blood thinning.”
How Is Blood In Stools Treated
The right treatment for blood in your stool depends on what is causing the problem.
If it is caused by haemorrhoids or an anal fissure, the treatment could be to make changes to your lifestyle or diet. Sometimes surgery is needed.
If the bleeding is due to a haemorrhage, for example if you have diverticular disease, you may need emergency surgery.
Polyps may be removed during a colonoscopy. If you have bowel cancer, you might need more urgent and invasive treatment such as surgery, chemotherapy, radiotherapy or other treatments.
Feature Article: Medications And Covid
Many people take regular medications, so as they prepare to get the COVID-19 vaccine, they wonder whether their medications will interfere with the vaccine or vice versa. In this article, we will discuss why some medications may be expected to alter the response to the vaccine and others would not. However, given the almost 40 different categories of medications and the thousands of medicinal products distributed, this article will not exhaustively address the topic. With this in mind, individuals should always consider three important points:
Four types of medications have been commonly discussed related to COVID-19 vaccinations, so we will start by addressing these:
- Antipyretics
- Antihistamines
Don’t Miss: Ulcerative Colitis And Apple Cider Vinegar
How To Use Suppositories
Your doctor or pharmacist will tell you how many suppositories to use each day. Some types you use once a day before you go to bed, and others you use several times a day with the last dose before you go to bed. Use them after you do a poo.
Try not to do a poo for at least an hour after using a suppository. This gives the medicine time to work.
What Causes Rectal Bleeding In Plano Tx

Blood in the stool means that there is bleeding somewhere in the digestive tract. Finding blood in the toilet or on toilet paper can be very alarming. Rectal bleeding can range from seeing a few spots of blood on the toilet paper when you wipe to having a toilet bowl full of blood after a bowel movement. The most common causes of rectal bleeding are:
- Anal fissure
- Blood thinner medications
Also Check: Natural Treatment Of Ulcer In Hindi
What Should I Know About Storage And Disposal Of This Medication
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture .
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program. Talk to your pharmacist or contact your local garbage/recycling department to learn about take-back programs in your community. See the FDA’s Safe Disposal of Medicines website for more information if you do not have access to a take-back program.
It is important to keep all medication out of sight and reach of children as many containers are not child-resistant and young children can open them easily. To protect young children from poisoning, always lock safety caps and immediately place the medication in a safe location â one that is up and away and out of their sight and reach.
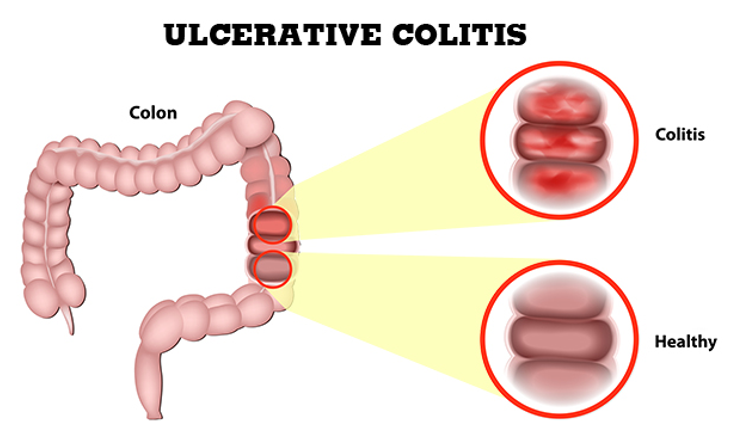
Uc Symptoms Can Get Worse Over Time
Because UC is a chronic disease, symptoms can change or get worse over time. Many people go through periods when they experience few or no symptoms, known as remission, as well as periods of flare-ups when they experience frequent and/or more intense symptoms.
If youre still experiencing symptoms, even while being treated for UC, it could be a sign that your symptoms are not under control.
Experiencing uncontrolled symptoms could mean its time to consider a new treatment.
Recommended Reading: Can Diverticulitis Cause Ulcerative Colitis
Recommended Reading: What Does An Ulcer Look Like
Watery Diarrhea After A Camping Trip
This can be due to giardia,a protozoal organism that is found in freshwater and the reason that you should always boil and sanitize water from mountain streams or lakes, Carrubba said.
Ingestion of this organism can result in giardiasis, which leads to abdominal pain and persistent, watery diarrhea. The issue can be treated with antimicrobials. In addition to drinking contaminated water, you can also be exposed to giardia by eating uncooked vegetables or fruits that were rinsed in contaminated water and by improperly washing hands after coming into contact with feces or an infected human or animal.
Warfarin Levels & Dementia: Second Opinion
The new findings definitely suggest that keeping warfarin within the ideal range provides dementia protection as well as stroke protection, says Luigi Di Biase, MD, PhD, senior researcher at the Texas Cardiac Arrhythmia Institute, St. David’s Medical Center, Austin. He reviewed the findings.
“It makes absolute sense,” he says. However, he concedes, it can be difficult for patients with atrial fibrillation to stay in that optimal range. This is because warfarin can interact with other drugs. And certain foods and drink can affect how well warfarin works.
RELATED: Dementia Prevention What Can Be Done?
Also Check: Signs Of A Bleeding Stomach Ulcer
Quick Facts About Black Stool
- Most cases of black stools are from eating black foods or iron supplements.
- Stool that is black due to blood indicates a problem in the upper GI tract.
- Blood in the stool can be detected through a stool test.
- See your healthcare provider right away if you have black stool along with pain, vomiting, or diarrhea.
- If you suspect there is blood in your stool, contact your healthcare provider as soon as possible.
How To Cope With Side Effects Of Mesalazine
What to do about:
- indigestion, stomach pain or wind â try not to eat foods that cause wind . Eat smaller meals, and eat and drink slowly. Puttingâ¯a heat pad or covered hot water bottle on your stomach may also help with stomach pain.
- feeling or being sick â stick to simple meals and do not eat rich or spicy food. Check the instructions that come with your medicine to see if you can take it after you’ve eaten. If you’re being sick, try having small, frequent sipsâ¯of water or squash to avoid dehydration. Do not take any other medicines to treat vomiting without speaking to a pharmacist or doctor.
- diarrhoea â drink plenty of fluids, such as water or squash, to avoid dehydration. Do not take any other medicines to treat diarrhoea without speaking to a pharmacist or doctor.
- headaches, muscle aches and pains â drink plenty of water and ask your pharmacist to recommend a suitable painkiller. Tell your doctor if the aches continue despite taking painkillers or if they last for more than a few days.
Don’t Miss: Can Stomach Ulcers Be Cancerous
How Does Blood In The Stools Appear
According to the Canadian Institute of Intestinal Research, most people with UC experience varying levels of hematochezia, which refers to blood in the stools. The blood will usually be clearly visible in the stool â which has a semi-solid consistency â or on the surface. The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate.
Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
People with UC may have slow, steady bleeding when they do not have a bowel movement. They may also experience bloody diarrhea and constipation.
Some individuals with severe UC may notice blood in their stools more than 10 times a day.
People with UC will also usually have mucus in the stools but may not be able to see it. The mucus helps protect the inner lining of the intestines, as well as helping with bowel movements.
According to the Crohnâs and Colitis Foundation, people need immediate medical attention if they experience rectal bleeding with blood clots in stools.
Treatment To Reduce Blood Clot Risk
Study researcher Matthew J. Grainge, MD, of the University of Nottingham, and colleagues conclude that patients with symptomatic IBD who are not hospitalized may benefit from short-term treatment with intravenous heparin or other anticlotting drugs.
But in an editorial published with the study, University of Toronto inflammatory bowel disease specialist Geoffrey C. Nguyen, MD, PhD, writes that this may be premature.
He notes that treating non-hospitalized patients with daily injections of heparin has no proven effectiveness and would add to the disease burden.
Johns Hopkins University School of Medicine IBD specialist Mark Lazarev, MD, tells WebMD that a study comparing treatment vs. non-treatment for reducing blood clot risk would be expensive and difficult to do.
“You would need a large number of patients because the individual risk is very low,” he says.
Stephan R. Targan, MD, who directs the IBD Center at Cedars-Sinai Medical Center in Los Angeles, agrees it is too soon to talk about treating all patients with symptomatic IBD to reduce their blood clot risk.
“It doesn’t really make sense to talk about treating the entire population with active IBD,” he tells WebMD. “Maybe if we knew more about what predisposes people with these conditions to develop blood clots we could target such treatments. But right now we can’t do that.”
Show Sources
Recommended Reading: How To Heal Colon Ulcers
What Was Causing The Blood Clot
Then, though, my leg swelled up and I could barely walk across my apartment. I knew that at this point something was wrong. When I contacted my doctor, he told me to go to the emergency room immediately because he suspected this could be a blood clot, which could be a side effect of the many medications I was on at the time, including mesalamine, a biologic, and prednisone. The doctor likely saved my life, as I was diagnosed with a blood clot in my leg, which could’ve become something worse.
Thankfully, this clot was caught in time so my treatment was relatively simple. I was given blood thinners in the hospital and then was told to continue these for 3-6 months while following up with a hematologist. The only negative to the blood thinners was the possibility that my rectal bleeding might also increase. Luckily, if it did increase, it was not by a noticeable amount.
When I met with the hematologist, we discussed the possible causes of my blood clot. She explained that I did have some risk factors. One was that I had been on oral birth control for about a decade and that wed gone on a long 10- or 11-hour drive. Although she also said that blood clots due to driving are less common than those due to flying.
What Other Information Should I Know
Keep all appointments with your doctor and the laboratory. Your doctor may order certain lab tests to check your response to olsalazine. Before you have any laboratory tests, tell the laboratory personnel that you take olsalazine, as this medication may interfere with some laboratory tests.
Do not let anyone else take your medicine. Ask your pharmacist any questions you have about refilling your prescription.
It is important for you to keep a written list of all of the prescription and nonprescription medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Recommended Reading: Can Duodenal Ulcer Cause Back Pain
Aspirin Warfarin Or Both For Primary Prevention Of Cardiovascular Disease
Eric A. Dietrich, PharmD, BCPS, and Kyle Davis, PharmD, BCPS
The use of aspirin therapy for the primary prevention of cardiovascular disease has become commonplace in the United States. Clinical trials have demonstrated that the use of aspirin in high-risk patients may be associated with fewer coronary events in men and fewer strokes in women.1 Additionally, the US Preventive Services Task Force recommends the use of aspirin for the primary prevention of CVD in at-risk patients aged 50 years and older.2
For patients receiving aspirin for primary prevention who suddenly require short-term anticoagulation with warfarin for deep vein thrombosis or pulmonary embolism , a difficult clinical decision is required of their primary care provider: continue both agents at the risk of increased bleeding, or discontinue aspirin and assume that warfarin will provide sufficient cardioprotection.
Is there evidence supporting the use of warfarin in the primary prevention of CVD?
Patient Case
JJ is a 63-year-old man with a history of type 2 diabetes mellitus, hypertension, and dyslipidemia. He is a current smoker with a 40 pack-year history. He is taking 500 mg of metformin twice daily for his diabetes 40 mg of lisinopril daily and 25 mg of chlorthalidone daily for his hypertension 40 mg of atorvastatin daily for his dyslipidemia and diabetes and 81 mg of aspirin daily for primary prevention of CVD.
The Evidence
Clinical Application
Outcome of the Case
References:
Why Blood Clots Are More Common In People With Ibd
Its well known that inflammatory bowel disease is associated with what’s called extra-intestinal manifestations: conditions that are related to IBD but arent found in the digestive tract. One of these is the risk of developing blood clots.
The increased risk of blood clots in people with Crohn’s disease and ulcerative colitis is known to IBD experts but it may not be as well understood by other physicians and by people who have IBD. It’s unclear exactly why people with IBD are at risk for blood clots but it’s thought to have to do with disease activity and changes in the blood that promote clotting.
While the risk of blood clots has been shown to be higher in people with IBD, there are things that can be done to prevent them. Whats vital is that people with IBD understand their personal risk of blood clots and that physicians take steps to avoid this complication when necessary, such as after surgery. People with IBD can also familiarize themselves with symptoms of a blood clot, such as pain, swelling, tingling, and pale skin in one leg.
Read Also: Vsl 3 For Ulcerative Colitis
What To Expect At Your Office Visit
Your provider will take a medical history and perform a physical exam. The exam will focus on your abdomen.
You may be asked the following questions:
- Are you taking blood thinners, such as aspirin, warfarin, Eliquis, Pradaxa, Xarelto, or clopidogrel, or similar medicines? Are you taking an NSAID, such as ibuprofen or naproxen?
- Have you had any trauma or swallowed a foreign object accidentally?
- Have you eaten black licorice, lead, Pepto-Bismol, or blueberries?
- Have you had more than one episode of blood in your stool? Is every stool this way?
- Have you lost any weight recently?
- Is there blood on the toilet paper only?
- What color is the stool?
- When did the problem develop?
Also Check: Support Surfaces For Pressure Ulcer Prevention
Lower Your Risk Of Workplace Injuries
If you work in a high-risk profession as a racecar driver or a lumberjack or construction worker who uses heavy machinery, for example you would be well advised not to take a blood thinner, Garcia says. Or you should avoid those high-risk tasks while on the medication.
This advice would only apply to someone with a high risk of trauma while they work. In most cases, your job shouldnt prevent you from taking a blood thinner, Garcia adds.
Read Also: Ulcerative Colitis Loss Of Appetite