Ulcerative Colitis And Colonoscopy
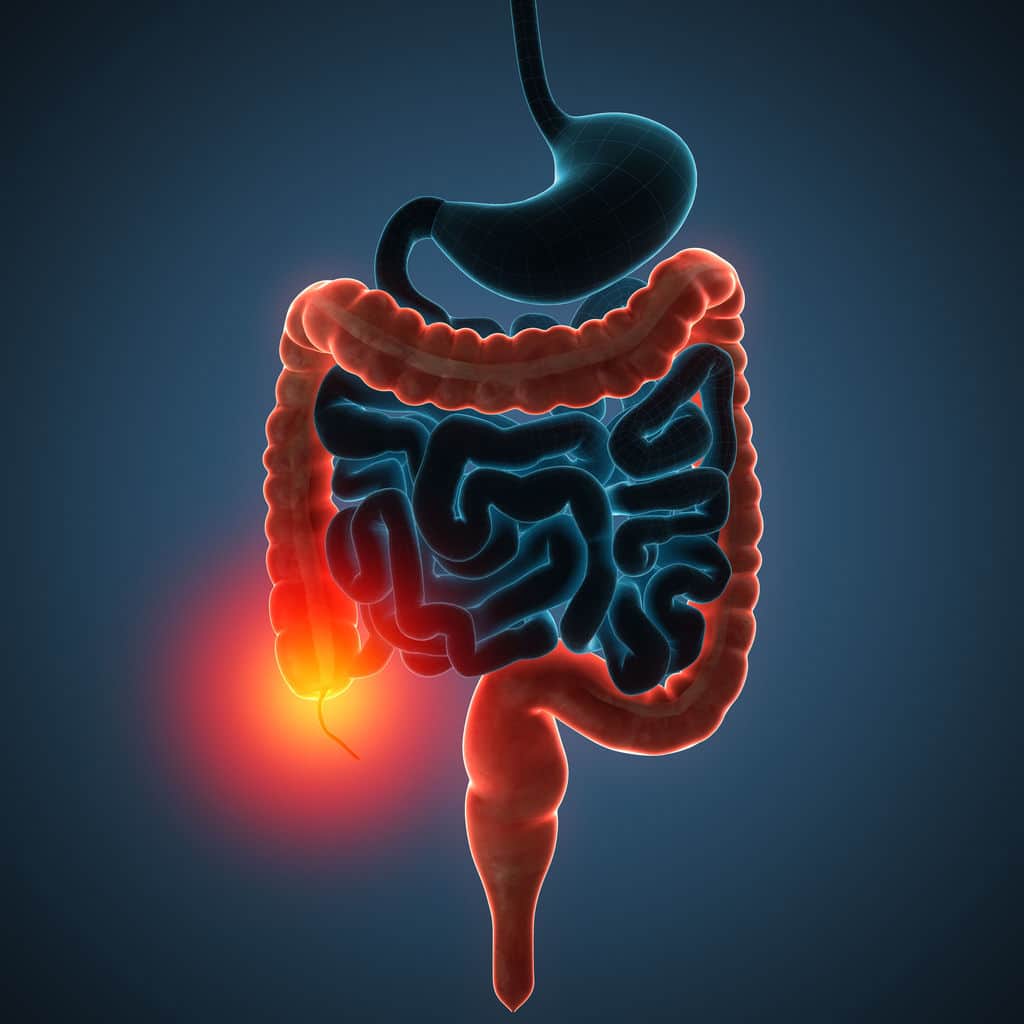
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
Once the medication takes effect, the doctor will insert a colonoscope into your anus. This device is long and flexible so it can move easily through your GI tract. The colonoscope also has a camera attached so your doctor can see inside the colon.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
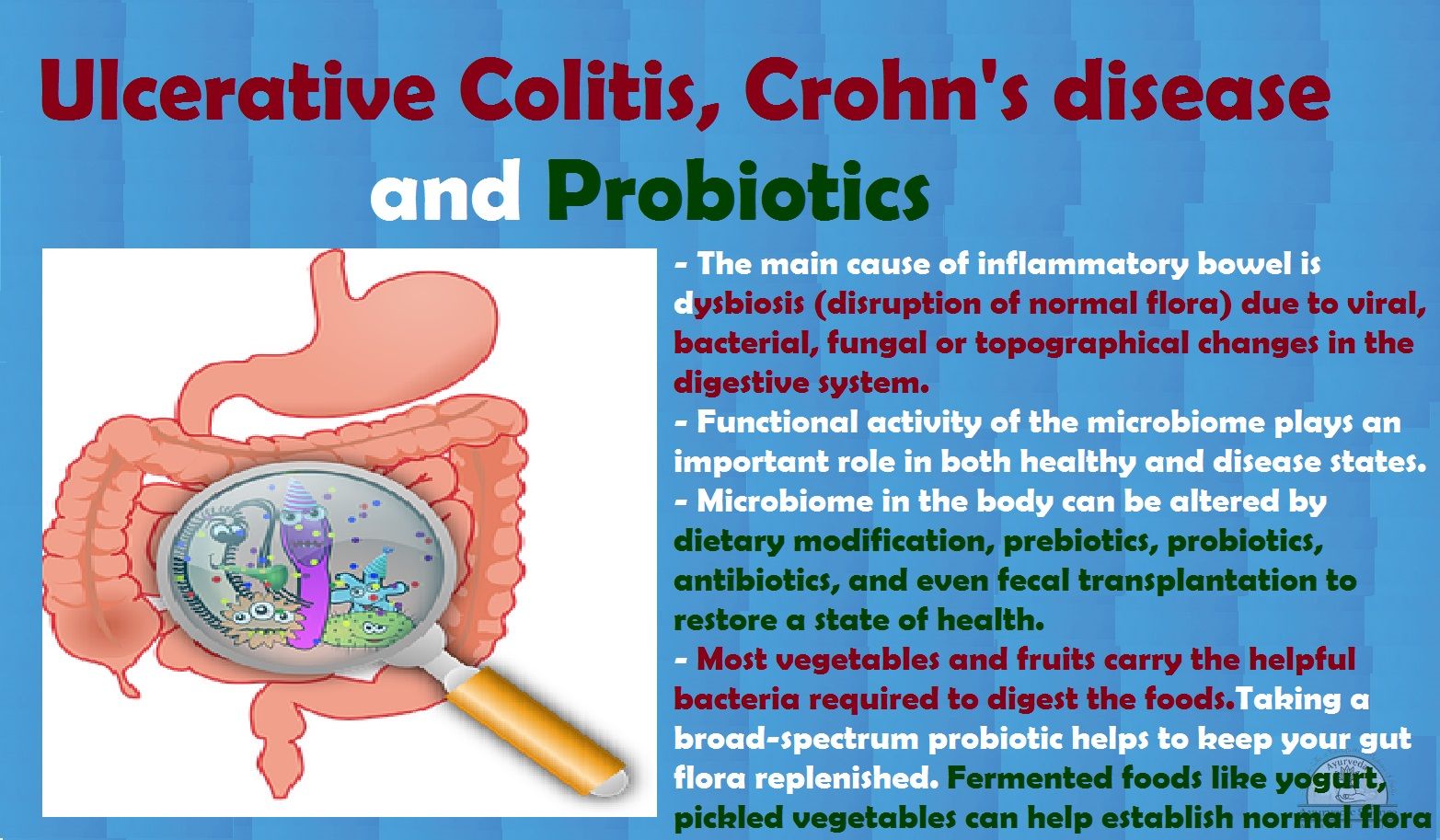
Crohns Disease And Ulcerative Colitis And Diet
Diet and food allergies do not cause IBD, and long-term special diets are not effective in treating IBD. However, adjusting your diet can help manage some of your symptoms, and can help IBD medications work better. A person with IBD has to pay close attention to their diet, since they may have malnutrition.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Don’t Miss: How To Get Remission In Ulcerative Colitis
Proctocolectomy And Ileoanal Anastomosis
Proctocolectomy is removal of the entire colon, including the lower part of the rectum and the sphincter muscles that control bowel movements. It can achieve a complete cure, but it is a last resort for ulcerative colitis that has not been helped by drug therapy.
Ileostomy
In some proctocolectomies, the surgeon creates an opening in the abdominal wall to allow passage of waste material. This part of the procedure is referred to as an ileostomy. The stoma is created in the lower right corner of the abdomen. The surgeon then connects cut ends of the small intestine to this opening. An ostomy bag is placed over the opening and accumulates waste matter. It requires emptying several times a day.
Ileoanal Anastomosis
Ileal pouch anal anastomosis , also simply called ileoanal anastomosis, has now largely replaced ileostomy because it preserves part of the anus and allows for more normal bowel movements. The procedure creates a natural pouch to collect waste, rather than using an ileostomy bag. The standard procedure involves:
What If I Get Sick
The main symptoms of COVID-19 are a fever, dry cough, and shortness of breath. It can also cause:
- Fatigue
- Loss of taste or smell
- Sore throat
- Skin rash
If you notice a change in how youâre feeling, call your doctor.
Most importantly, if you think you might have COVID-19, isolate yourself from other people. Call your doctor or follow the advice where you live to learn what to do next and how long youâll need to stay away for other people.
Free COVID testing is available in most communities. Some locations require an appointment while others are drive-up. Check with your local health department about testing availability.
You May Like: What To Drink With Stomach Ulcer
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Extraintestinal Manifestations And Complications
Aphthous ulcersPyoderma gangrenosum
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes. Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Uveitis and iritis are more commonly associated with ulcerative colitis, whereas episcleritis is more commonly associated with Crohn’s disease.
You May Like: Ulcerative Colitis Iv Infusion Treatment
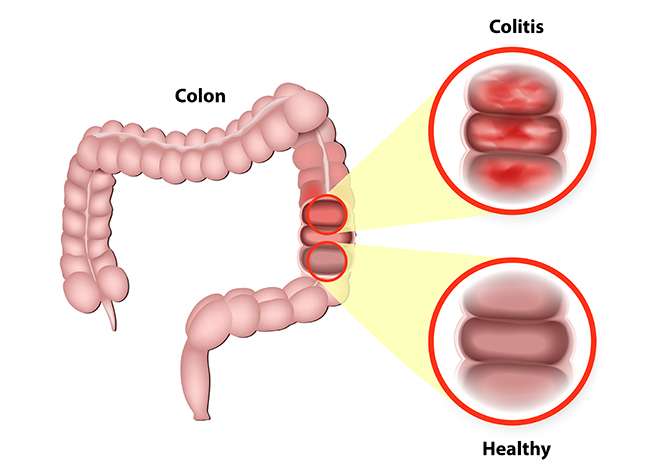
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- feeling tired
- dehydration
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Eating Diet And Nutrition
Researchers have not found that eating, diet, and nutrition play a role in causing ulcerative colitis symptoms. Good nutrition is important in the management of ulcerative colitis, however. Dietary changes can help reduce symptoms. A health care provider may recommend dietary changes such as the following:
- avoiding carbonated drinks
People should speak with a health care provider about specific dietary recommendations and changes.
Read Also: Does Smoking Cause Ulcers After Gastric Bypass
How Close Are We To A Cure
Ulcerative colitis is an inflammatory bowel disease that mainly affects the lining of the large intestine . This autoimmune disease has a relapsing-remitting course, which means that periods of flare-ups are followed by periods of remission.
Right now, theres no medical cure for UC. Current medical treatments aim to increase the amount of time between flare-ups and to make flare-ups less severe. This may include a variety of medications or surgeries.
Still, UC research continues to explore other methods to decrease the inflammation associated with this autoimmune disease. Learn more about the new UC treatments that have recently come out on the market, as well as emerging therapies that could be other options in the future.
Two new types of medications for UC have emerged in recent years: biosimilars and Janus kinase inhibitors.
Tips For Healthy Ulcerative Colitis Poop
There are several different approaches to UC treatment. Medications, diet, and other lifestyle changes can all help improve bowel symptoms in UC.
The foremost treatment for ulcerative colitis inflammation and related stool changes is medication. These include:
- Aminosalicylates such as Asacol or Azulfidine , to reduce inflammation
- Corticosteroids such as prednisone and Entocort EC , to reduce inflammation
- Immunomodulators such as Imuran or cyclosporine, to reduce your immune system response
- Biologic therapies such as Remicade or Simponi , to neutralize proteins made by the immune system and reduce inflammation
Your diet also plays a role in your bowel habits. After all, what goes in, must go through and come out. The following diet modifications may help reduce bowel symptoms:
- Avoid your individual trigger foods.
- Limit dairy products.
- Drink plenty of water throughout the day.
- Eat small meals.
Stress is another factor that can contribute to changes in the stool. The brain-gut connection may play a role in inflammation of the GI tract. Managing your stress levels might be able to decrease diarrhea and other changes in your stool.
In addition, participating in regular physical activity is healthy for the GI tract. Exercise helps with the movement of stools, which can be especially helpful for constipation.
Read Also: What Is The First Sign Of Stomach Ulcer
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
- low energy
- weight loss
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
During surgery, your small intestine will either be diverted out of an opening in your abdomen or be used to create an internal pouch that’s connected to your anus called an ileoanal pouch.
You May Like: What Is The Medication For Ulcerative Colitis
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
What Makes It Worse
The reasons why aren’t totally clear. Doctors don’t know why it affects only a small section in one person, but spreads through the entire colon in another. But certain triggers sometimes play a role. These include:
Food. It’s different for everyone, but certain foods can irritate your symptoms. For example:
- Caffeine can make severe diarrhea worse
- Dairy may lead to more diarrhea, gas, and pain
- Fizzy drinks can be a problem if you have gas
- Greasy and fried foods often lead to gas and diarrhea
- High-fiber foods, such as fresh fruits and veggies, whole grains, corn, nuts, and seeds, can be hard on you
- Spicy foods can be tough to handle
Stress. It can trigger flare-ups and make your symptoms much harder to deal with. It’s especially challenging because just having ulcerative colitis can bring on more of it.
Skipping meds. Even when you’re in remission, it’s very important to take your meds. In the best case, they prevent flare-ups. And even if not, they can help keep things under control.
Follow these 5 tips to help control your ulcerative colitis flare-ups.
Don’t Miss: How Do You Treat A Duodenal Ulcer
Complications In The Intestine
Malabsorption and Malnutrition
Malabsorption is the inability of the intestines to absorb nutrients. In inflammatory bowel disease , this occurs as a result of bleeding and diarrhea, as a side effect from some of the medications, and as a result of surgery. Malnutrition may occur in ulcerative colitis, but it tends to be less severe than with Crohn disease.
Toxic Megacolon
Toxic megacolon is a serious complication that can occur if inflammation spreads into the deeper layers of the colon. In such cases, the colon enlarges and becomes paralyzed. In severe cases, it may rupture, which is a life-threatening event requiring emergency surgery. Symptoms include weakness, abdominal pain, abdominal distention, and frequently, fever.
Toxic megacolon is characterized by extreme inflammation and distention of the colon. Common symptoms are pain, distention of the abdomen, fever, rapid heart rate, and dehydration. This is a life-threatening complication that requires immediate treatment, usually surgical removal of the colon.
Bleeding and Anemia
Rectal bleeding due to ulcers in the colon is a common complication of ulcerative colitis. It can increase the risk for anemia . In some cases, internal bleeding can be massive and dangerous, requiring surgery.
Intestinal Infections
Colorectal Cancer
Signs And Symptoms Of Ulcerative Colitis
While the clinical signs of ulcerative colitis can vary from child to child, some symptoms may be more common than others, including bloody diarrhea. Other symptoms related to inflammation in the colon may include: abdominal pain, urgent or uncontrollable bowel movements, poor appetite, weight loss, and fatigue. Some children may experience less common symptoms, including skin rashes, joint pain, fatigue or fevers.Ulcerative colitis is a chronic condition, meaning children may have periods of no symptoms alternating with periods of active symptoms . Mild symptoms may present at first, while in other children, the onset of symptoms is more severe.
Read Also: Over The Counter Medication For Ulcerative Colitis
Complications Caused By Nutritional Deficiencies
Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
Blood And Stool Tests
A blood test can show if you have anemia, which is a symptom of ulcerative colitis. Anemia happens when your red blood cells decrease and there arenât enough of them to carry adequate oxygen to your tissues. A blood test will also help identify or rule out other infections.
The blood test can also detect an increase in white blood cells, a low level of the protein albumin, and an elevated C-reactive protein level — all indications of inflammation in your body.
When you go to the doctorâs office, they will take a little of your blood and send it off for analysis. The results will come back anywhere from a couple of days to several weeks later.
A stool test may be ordered to rule out infection. Learn more about stool testing.
You May Like: Ulcerative Colitis Caused By Alcohol
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Don’t Miss: How Long Does Prednisolone Take To Work For Ulcerative Colitis