Tylenol And Heat Therapy
Doctors frequently prescribe nonsteroidal anti-inflammatory drugs such as ibuprofen or aspirin to help manage back pain. However, NSAIDs arent typically a viable solution for people with UC, as the medication can cause symptoms to flare.
Those with ulcerative colitis can generally take the pain reliever acetaminophen which is not an NSAID for minor aches and pains without side effects. Applying moist heat to affected areas may also reduce pain.
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.
Key Points About Ulcerative Colitis In Children
-
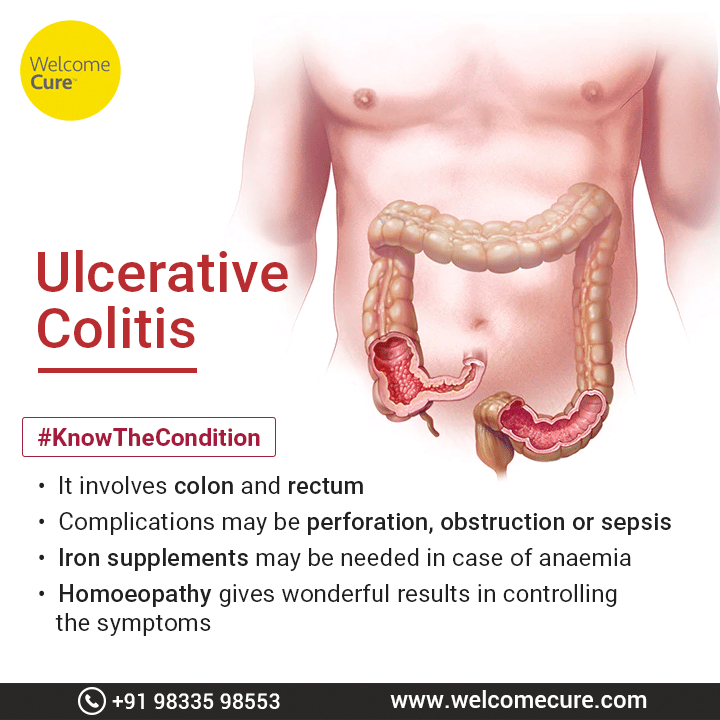
Ulcerative colitis is an inflammatory bowel disease. In this condition, the inner lining of your childs large intestine and rectum gets inflamed.
-
This inflammation causes diarrhea or frequent emptying of the colon. Your child may also have stomach pain and diarrhea.
-
Treatment may include avoiding foods that cause symptoms, taking medicine, and having surgery.
-
Children with this condition need long-term care. Your child may have times when symptoms go away. But symptoms usually come back.
Read Also: Crohn’s Vs Ulcerative Colitis Treatment
What Is Uc Cramping
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.
Meal Timing And Portion Sizes
For most people with IBD,eating small meals is easier on the digestive tract. For others, the simple act of eating can rev up the digestive system and make diarrhea worse. If your bowel movements subside when you take a break between meals, consider reworking your meal timing to include more substantial meals less often.
Since UC symptoms vary from person to person, theres no one-size-fits-all meal schedule. Pain can feel worse when youre not well-rested. Choose meals that are easy to tolerate when its close to bedtime, or finish eating for the day a few hours before going to sleep.
Don’t Miss: Ulcerative Colitis When Should I Go To Hospital
When You’re In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Recommended Reading: Whats A Stomach Ulcer Feel Like
Surgery For Ulcerative Colitis
Surgery for ulcerative colitis usually involves removing the entire colon and the rectum. Removal of the colon and rectum is the only permanent cure for ulcerative colitis. This procedure also eliminates the risk of developing colon cancer. Surgery in ulcerative colitis is reserved for the following patients:
Standard surgery involves the removal of the entire colon, including the rectum. A small opening is made in the abdominal wall and the end of the small intestine is attached to the skin of the abdomen to form an ileostomy. Stool collects in a bag that is attached over the ileostomy. Recent improvements in the construction of ileostomies have allowed for continent ileostomies. A continent ileostomy is a pouch created from the intestine. The pouch serves as a reservoir similar to a rectum, and is emptied on a regular basis with a small tube. Patients with continent ileostomies do not need to wear collecting bags.
Dont Miss: How To Treat Stress Ulcers
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Recommended Reading: Do Ulcers Cause Burning In The Stomach
Diagnosis Of Ulcerative Colitis
X-rays of the abdomen taken after barium is given by enema do not require any special preparation . These x-rays usually can show a blockage or paralysis… read more ) may indicate the severity and extent of the disease but are not done when the disease is active, such as during a flare-up, because of the risk of causing a perforation. Other x-rays of the abdomen may also be taken.
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
Read Also: What Causes Ulcers To Flare Up
When Does Cramping Usually Happen
UC cramps can be exacerbated by food, so many people notice cramping after eating or before a bowel movement, says Ha. Cramping can also be tied to eating trigger foods, which often include high-fiber fruits and veggies, lactose, nonabsorbable sugars, high-fat or sugary foods, alcohol, and caffeine.
The hormone fluctuations that occur during a womans menstrual cycle may also trigger UC cramping, according to a study published in January 2018 in Inflammatory Bowel Diseases.
Cramping can occur at all times and throughout the night. Medication and other treatments can help reduce symptoms.
Study Population And Genetic Information
For our analysis, clinical, epidemiological and genetic data of 2063 individuals with IBD were available. 1206 of those patients were diagnosed with CD and 857 with UC. Table provides an overview of the study population our study population comprises patients with mild, moderate and severe disease. The collected data of up to nine years of follow-up was analysed.
Table 1 Basic data and disease characteristics
Don’t Miss: Offloading The Diabetic Foot For Ulcer Prevention And Healing
What Do Abdominal Spasms In Ulcerative Colitis Feel Like
People with ulcerative colitis have many different experiences with abdominal or intestinal spasms. Sometimes, these spasms can be uncomfortable, but not painful. As one MyCrohnsAndColitisTeam member wrote, Ive been having spasms in my colon since yesterday. I am so glad they arent painful, but its super annoying. Another agreed, saying, I dont think my abdominal spasms really hurt at all.
Some people with UC have painful spasms. One member described their daily spasms like this: Normally, by 8 p.m., the spasms start in my colon. By 10 p.m., I usually go to the bathroom in tremendous pain and with more spasms. Another member who also experiences painful spasms wrote, I have been having rectal spasms that last and cause me so much pain! My whole pelvic floor is sore.
Ultimately, the abdominal spasms associated with ulcerative colitis can range from annoying and frustrating to painful and debilitating. No matter what they feel like, talking to your doctor may help you find ways to manage this symptom and improve your quality of life.
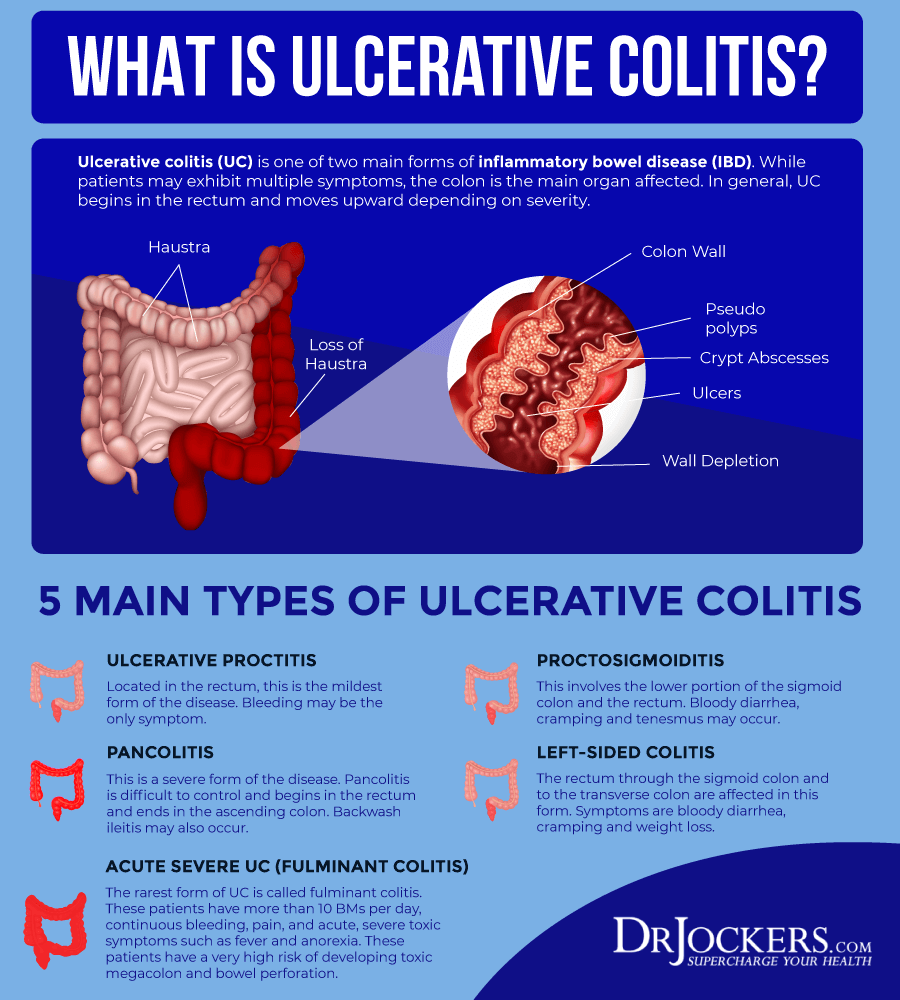
What Is Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease. It is sometimes referred to simply as ‘colitis’.
It causes painful swelling and redness in the digestive tract. This can lead to symptoms such as abdominal pain and diarrhoea. Its estimated that more than 33,000 Australians have UC.
Inflammation is a normal way in which the immune system defends the body when fighting off invaders, such as bacteria or viruses. Usually, the inflammation disappears once the invaders are destroyed. With UC, a problem with the immune system causes the inflammation to continue, damaging the walls of the digestive tract.
Read Also: What Should You Eat With Ulcerative Colitis
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
What Are The Risk Factors Of Ulcerative Colitis
The cause of ulcerative colitis is unclear, but its thought that a combination of genetics and environmental factors are at play. Up to 20 percent of people with ulcerative colitis have a parent, sibling or child with the disease.
Ulcerative colitis is more common for people living in urban, industrialized areas compared to undeveloped countries, which indicates that highly refined diets may play a role. Although all ethnic groups are affected, the problem is most common among Caucasians and people of Eastern European Jewish descent.
Lastly, there appears to be a connection to nonsteroidal anti-inflammatory medications. Its not that these medications cause the disease but, because they inflame the bowel, they can worsen symptoms. This category of medication includes ibuprofen , naproxen sodium and diclofenac sodium .
You May Like: What Is A Perforated Ulcer
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Whats A Good Plan To Manage Uc Cramping
Monitor your medications. Talk to your doctor about any prescription, over-the-counter, or herbal medications youre taking. Iron deficiency is common with UC, but oral iron supplements have been shown to increase the risk of inflammation and cramping. Some antibiotics and pain relievers, such as ibuprofen, may also increase flare-ups and cramping.
Review your diet. Keep a food diary and note the connection between the foods you eat and your UC symptoms. In general, its smart to stay away from processed foods and those high in saturated fat and sugar. High-fiber foods and dairy products can also cause UC cramping, but check with your doctor before eliminating foods from your diet, to ensure youre getting the nutrients you need.
Eat frequent, small meals. Instead of two or three large meals, eat four to six smaller meals spaced more closely throughout the day. Also, take your time while eating and chew thoroughly.
Skip caffeine and carbonated drinks. Caffeine can cause gas, intensifying abdominal cramping. It is also a stimulant, which can make cramping and diarrhea worse.
Drink enough water. People with UC may be at increased risk of dehydration, so be sure to drink plenty of H2O. A good rule of thumb, according to the Crohns and Colitis Foundation, is to aim for about 64 ounces or eight 8 oz glasses per day.
Also Check: Ulcerative Colitis Kidney Stones Type
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
You May Like: Specific Carbohydrate Diet Ulcerative Colitis
Stomach Pain Could Be Ulcerative Colitis
Ulcerative colitis is a chronic disease that causes inflammation/irritation and sores called ulcers on the inner lining of the large intestine or the colon. Here the lining of the colon becomes inflamed and develops tiny open sores, or ulcers, that produce pus and mucous. Usually the cells and proteins that make up the immune system protect one from infection. In people with inflammatory bowel diseases, however, the immune system mistakes food, bacteria, and other materials in the intestine for foreign or invading substances. During such situations the body sends white blood cells to the lining of the intestines, where they produce chronic inflammation and ulcerations. Temporary inflammation is caused by the immune system to combat an illness or infection, and then the it is reduced but in people with ulcerative colitis, however, this inflammation can persist long after your immune system finishes its job.
Thus, Ulcerative colitis is a chronic inflammatory disease of the gastrointestinal tract, and is also called inflammatory bowel disease .
Causes ofUlcerative colitis
What are the risk factors of Ulcerative colitis?
The exact cause of ulcerative colitis is unknown. The following factors may play a role in causing ulcerative colitis among people:
Symptoms
Ulcerative colitis symptoms may be different for different people and may also depend on the severity of inflammation and where it occurs. Signs and symptoms may include:
Diagnosis of the disease
Treatment
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Also Check: What Is Good For Ulcer Pain