Signs You Should Get Help For Ulcerative Colitis
You shouldn’t put off seeing a doctor if you have these common symptoms of ulcerative colitis:
- Abdominal pain or cramps
- Bloody diarrhea that doesn’t go away
- Bloated or tender abdomen
- Rectal pain or bleeding
- Urgent need to defecate
IBD experts at Rush can determine if you have ulcerative colitis and come up with a plan to help you stay in remission. If you are looking for a second opinion, our experts can help you understand all of the available treatments so you make the most informed decisions about your care.
When Ulcerative Colitis Symptoms Get Worse
If you’ve been battling ulcerative colitis for some time, you understand the need to break free from symptoms. Perhaps past treatments haven’t worked. Or maybe you’ve achieved remission, only to have your condition flare again. If you’re facing increasing symptoms of UC, take heart. There are innovative therapy options that can help you gain control.
If your UC symptoms progress beyond the mild stage, your doctor will change your treatment plan. People with moderate UC usually have four to six stools a day with rectal bleeding. Those with severe colitis usually have more than six stools a day with bleeding. They also experience other symptoms like fever, anemia, and increased heart rate.
Many people are successfully treated with 5-aminosalicyclic acids . However, it’s common to require more aggressive therapy at moderate and severe stages of the disease, when higher dosages of these medications fail to provide relief. Although every treatment plan is different, your doctor may consider the following options for treatment when 5-ASAs no longer work.
Complications Outside The Bowel
Colitis doesnt just affect the bowel. As many as 1 in 5 people with Colitis develop problems in other parts of the body. Most affected are joints, eyes or skin. These are known as extraintestinal manifestations . They usually happen during a flare-up, but can occur without or before any bowel symptoms. These complications can often happen to people who dont have Colitis too. For many of the complications, there are things you can do to reduce your risk.
Joints
You may have pain and/or swelling in your joints. Around 1 in 6 people with Colitis experiences joint problems. For some, this will get worse during a flare, but will usually improve with treatment for Colitis. Others may have joint problems even when bowel symptoms feel better. Find out more in Joints.
Bones
People with Colitis are more at risk of developing thinner and weaker bones or osteoporosis. This can be due to ongoing inflammation, smoking, taking steroids or low levels of physical activity. Calcium is needed for bone formation, and this may be low if your diet doesnt contain enough dairy. Weight-bearing exercise, calcium and vitamin D supplements, not smoking and avoiding long-term steroid use can help. Some people may also take bisphosphonate medicines. Find out more in our information on Bones.
Skin
Colitis can affect the skin in different parts of the body.
Eyes
Anemia
Anaemia can make you feel very tired. If its more severe you may also have shortness of breath, headaches, and general weakness.
Liver
Recommended Reading: What Foods Should You Avoid When You Have An Ulcer
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Some Doctors May Use The Following Table To Classify Your Symptoms*:
*A patient does not need to have all of these factors to be considered in a specific category of disease
Ulcerative colitis symptoms are considered moderate when you experience between 4-6 stools per day which include a moderate amount of blood. Severe UC is when you experience 6-10 per day with a severe amount of blood when passing.
If youre concerned about any of your symptoms, talk to your doctor immediately.
How would you describe your symptoms?
Do your best to keep track of your symptoms so you can clearly describe them to your doctor. This information is key in helping your doctor determine the right treatment for you.
because of my UC symptoms, I wasnt able to socialize with my friends. Unfortunately I was missing out on a lot of plans.
Sarah, a real UC patient using HUMIRA
Changing your routine because of UC symptoms? Youre not alone. Hear from others who have been there.
Read Also: How To Heal Mouth Ulcers
Recommended Reading: What Are Infusions For Ulcerative Colitis
You Can Use Telemedicine To Build A Strong Patient
Dont underestimate the importance of a good relationship with your doctor. When patients have good communication with their doctors, theyre especially likely to stick with their treatments and be more satisfied with their care, according to a review published in 2010 in The Ochsner Journal. If the communication between patient and doctor is poor, the patient can feel disheartened and may be less likely to stick with their treatment plan.
Both Battat and Chachu agree that combining in-person visits with telemedicine visits and the use of patient portals usually allows the doctor and patient to communicate with each other more effectively.
Its great to have access to both , as they each provide different options for patients, says Battat.
Donât Miss: Stelara Dosing For Ulcerative Colitis
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Read Also: How Do You Cure Mouth Ulcers
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Ulcerative Colitis Care At Seattle Childrens
Seattle Childrens has a special IBD Center to care for children with this complex condition.
- The experts you need are here
The clinic provides access to many IBD experts. We can schedule your visit so your child sees many of them in one place on the same day. We treat your whole child by combining care from specialists in digestive health, immune health, nutrition, surgery and psychology.
- We offer advanced treatments, including nutrition therapy
Through our IBD Center, we offer advanced treatments for children with ulcerative colitis that are not offered everywhere. This includes nutrition therapies such as the Specific Carbohydrate Diet . Our surgeons have the most experience in the region doing the highly technical surgeries that some children with ulcerative colitis need.
Read about our clinical trials using SCD to treat ulcerative colitis and other forms of IBD.
- Early therapeutic medicine monitoring
- One of the early signs of remission is how much medicine is still in your childs body after a certain amount of time. We will check your childs medicine levels early so we can individualize the dose, and increase the likelihood of your child getting and staying in remission.
Don’t Miss: Support Surfaces For Pressure Ulcer Prevention
You Dont Need To Change Your Diet Dramatically
Theres no evidence that following a strict diet can put you into remission or keep you there. In fact, cutting out certain foods could prevent you from getting the nutrients you need to stay healthy.
You may want to avoid certain foods like dairy products if they seem to aggravate your symptoms. However, talk with your doctor or a dietitian before making any major changes to your diet.
Will Ulcerative Colitis Make It Harder For Me To Get Pregnant
Researchers found that women with Crohns disease and ulcerative colitis, both types of inflammatory bowel disease, had a greater risk of pregnancy complications and poor maternal and fetal outcomes. The disease causes chronic inflammation of the gastrointestinal tract and typically occurs in young people.
Researchers reviewed more than 8 million pregnancies from 2016 to 2018, finding over 14,000 women with IBD. The research showed that pregnant women with IBD had higher numbers of gestational diabetes, postpartum hemorrhage, hypertensive complications, preterm delivery, fetal growth restriction and fetal death.
Patients with IBD also spent longer in the hospital after giving birth, by about a half-day, and had about $2,700 more in medical costs.
You May Also Like
We understand this news may create concern about your chances of having a healthy child, but this further reiterates the need to make the necessary changes before you begin trying to conceive.
Based on our findings, we suggest that women who have moderate to severe IBD should get pre-conception counseling and be treated aggressively to achieve remission prior to getting pregnant, Ghouri says. Our study results illustrate the importance that IBD be optimally controlled prior to conception.
Also Check: Can Foot Ulcers Be Cured
How We Care For Ulcerative Colitis
At the Boston Childrens Inflammatory Bowel Disease Center, our team believes that, with proper management, all children and teens with ulcerative colitis can live comfortably. We partner with you and your child to effectively manage IBD and provide support through all life stages, from school and relationships to work.
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
Recommended Reading: Holistic Treatment For Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
What Are Ulcerative Colitis Symptoms
Ulcerative colitis is an inflammatory bowel disease that can be life-threatening when the symptoms flare up. Its important for you to go to the hospital for treatment when your symptoms are too severe.
The condition doesnt have a cure, but it can have periods where the symptoms become extreme and flare-up or where they go into remission.
At least 25% of all cases of ulcerative colitis lead to hospitalization. You may need to be hospitalized many times throughout your life for this condition, particularly during flare-ups.
The main way to manage the disease is by taking an oral corticosteroid, typically in the form of a daily pill. You need to seek medical attentionand will likely be hospitalizedwhenever your body isnt responding to this treatment.
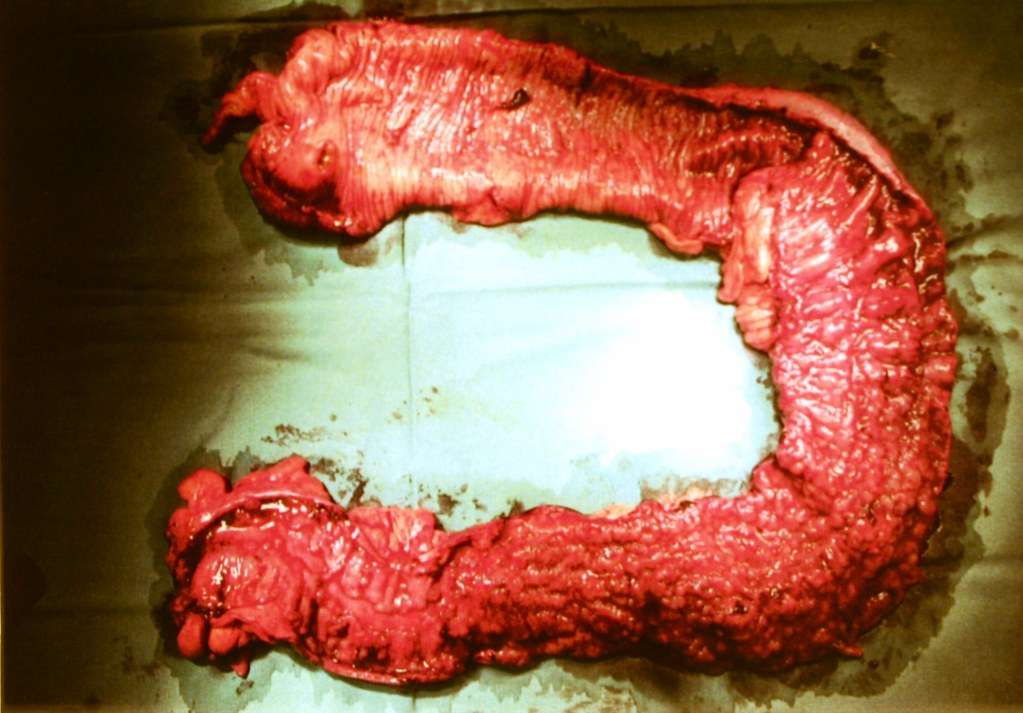
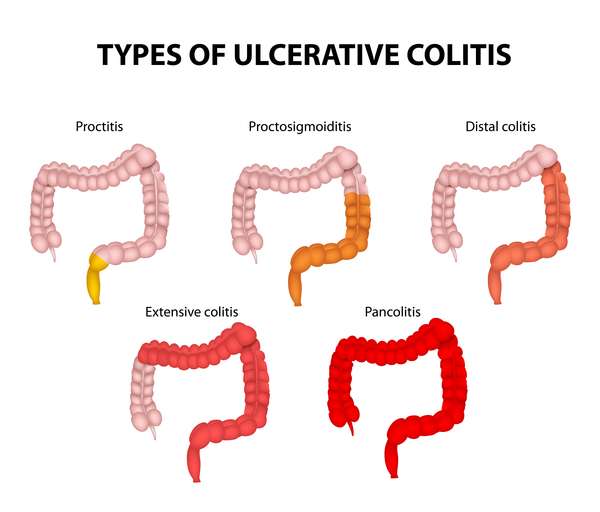
Ulcerative colitis usually begins with inflammation at the base of your colon. Over time, this inflammation can spread up the organ until the entire large intestine is affected.
This leads to many different symptoms, including:
Over long periods of time, ulcerative colitis can lead to further complications, including:
When Are Your Symptoms Severe Enough For Hospitalization?
Youll experience your ulcerative colitis symptoms on and off throughout your life. You should always contact your doctor when you have concerns about your symptoms or if new ones develop.
You should seek inpatient treatment at a hospital whenever:
You May Like: How To Treat Stomach Ulcers At Home
The Difference Between Ulcerative Colitis And Crohn’s Disease
Crohn’s disease is also an inflammatory bowel disease . The 2 diseases affect the digestive tract differently:
- Ulcerative colitis only affects the large bowel , and inflammation is only in the surface layers of the bowel lining. It causes ulcers to form in the lining of the bowel.
- Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus , but usually just the last section of the small bowel and/or the colon. Inflammation can extend into the entire thickness of the bowel wall.
What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
Also Check: What To Do For Leg Ulcers
Should I Go To The Hospital For Ulcerative Colitis Pain
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
How Does Blood In The Stools Appear
According to the Canadian Institute of Intestinal Research, most people with UC experience varying levels of hematochezia, which refers to blood in the stools. The blood will usually be clearly visible in the stool â which has a semi-solid consistency â or on the surface. The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate.
Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
People with UC may have slow, steady bleeding when they do not have a bowel movement. They may also experience bloody diarrhea and constipation.
Some individuals with severe UC may notice blood in their stools more than 10 times a day.
People with UC will also usually have mucus in the stools but may not be able to see it. The mucus helps protect the inner lining of the intestines, as well as helping with bowel movements.
According to the Crohnâs and Colitis Foundation, people need immediate medical attention if they experience rectal bleeding with blood clots in stools.
Recommended Reading: Can Ulcers Cause Black Stool
Warning Signs Of Perforated Bowel And Hemorrhaging
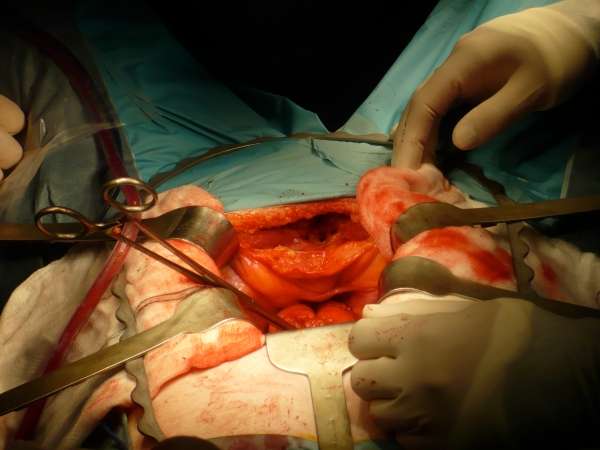
A perforated bowel is a hole in the wall of the intestine which can occur as a consequence of toxic megacolon, but can also be caused by intestinal infections, and certain types of medication.
A full colonoscopy during acute severe ulcerative colitis may also increase the risk of perforation, according to the January 2019 review in the BMJ Postgraduate Medical Journal.
This perforation is so dangerous because the contents of the intestine, which contain a large number of bacteria, can spill into the abdomen and cause a serious infection called peritonitis, notes the Crohn’s and Colitis Foundation.
Signs of bowel perforation include severe abdominal pain, a high fever, and heavy rectal bleeding or hemorrhaging. As a caregiver, look for, or ask about, sudden and dramatic increases in the amount of blood in your loved one’s stool.
If you suspect perforation, call 911 or go to the emergency room. Massive hemorrhaging in a patient with ulcerative colitis is an emergency condition that requires immediate medical attention and possibly surgical care to repair the hole in the colon wall.
RELATED: What Is Rectal Bleeding? Symptoms, Causes, Diagnosis, Treatment, and Prevention
How Can I Find Support After An Ulcerative Colitis Diagnosis
When taking care of your physical well-being, dont forget that ulcerative colitis can take a toll on your emotional and mental well-being too. If it turns out your symptoms are ulcerative colitis, you can find a support group, or ask your doctor if they can connect you with a therapist or G.I. psychologist. Dr. Riehl, for example, works with patients on aspects of body image and even connects them with other patients who have experienced colectomy or ostomy . We talk openly about the impact that it can have on them from an intimacy perspective to how it impacts their self-identity, she says.
Since ulcerative colitis often starts at an age when people are thinking about their first job or starting a family, it can be particularly tough. One of the reasons that I and several of my colleagues went into this field is precisely because of thatso that we can hopefully make a difference in peoples lives early, and have them be able to lead productive and complete lives by putting their disease in remission, Dr. Sinha says.
Also Check: What To Take For Mouth Ulcers