What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Appendix 6 Assessment Of Risk Of Bias
1. Was the allocation sequence randomly generated?
Low risk of bias
The investigators describe a random component in the sequence generation process such as: referring to a random number table using a computer randomnumber generator coin tossing shuffling cards or envelopes throwing dice drawing of lots.
High risk of bias
The investigators describe a nonrandom component in the sequence generation process. Usually, the description would involve some systematic, nonrandom approach, for example: sequence generated by odd or even date of birth sequence generated by some rule based on date of admission sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process provided to permit a judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation sequentiallynumbered drug containers of identical appearance sequentiallynumbered, opaque, sealed envelopes.
High risk of bias
Unclear
3. Blinding was knowledge of the allocated interventions adequately prevented during the study?
Low risk of bias
Any one of the following.
High risk of bias
Any one of the following.
Unclear
4. Were incomplete outcome data adequately addressed?
Low risk of bias
Unclear
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
- the Cochrane Wounds Specialised Register
- the Cochrane Central Register of Controlled Trials
- Ovid MEDILINE
- EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
- ClinicalTrials.gov
- WHO International Clinical Trials Registry Platform
- EU Clinical Trials Register .
Searching other resources
Recommended Reading: How To Heal Mouth Ulcers
Examples Of Smart Textiles For Wound Care
10.5.1Hydrogel dressings
Some of the gel-containing dressings on the market are: Tegagel , Curasol Hydrogel Saturated Dressing , DuoDerm Hydroactive Wound Gel , and Carrasyn Hydrogel Wound Dressing . One of the examples of wound dressings that has gel formed in situ is based on oxidised alginate, gelatine and borax.34 Each of these components has a specific function in the dressing. The gelatine has a haemostatic effect, while the alginate is well known for promoting wound healing and is supported by the antiseptic quality of borax. The combination of these functions makes the dressings very effective for moist wound healing. The alginate is oxidised, rapidly cross-links the gelatine and in the presence of borax gives in situ formation of hydrogel. It does not wrinkle or flute in the wound bed and moreover is non-toxic and biodegradable. It protects the wound bed from the accumulation of excess exudate because it has a capacity of fluid uptake that is 90% of its weight. It takes up the exudate, but still maintains the moist environment to facilitate and stimulate epithelial cell migration during the healing process.34
10.5.2Fluid-retention dressings
10.5.3Foam dressings
Some of the best known foam-dressing products are: Lyofoam , Polymem Non-Adhesive Dressings and Allevyn Adhesive Dressings .
10.5.4Silicone-foam pads
Some brand-name dressings which contain soft silicone are: Tendra Mepitel , Tendra Mepilex Lite and Tendra Mepilex Border .
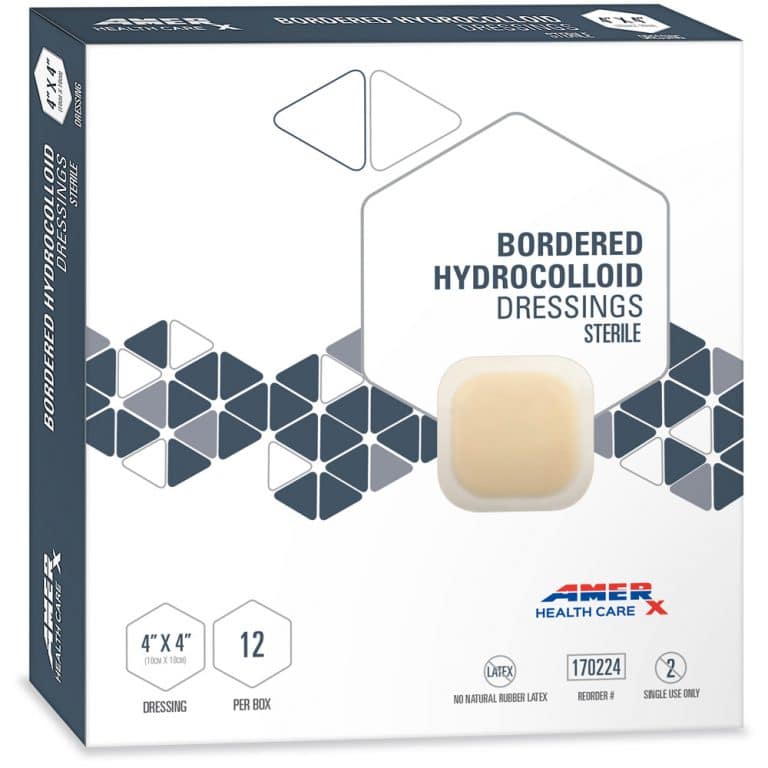
10.5.5Hydrocolloid dressings
Nursing Home Abuse & Neglect Resources

Common Cases:
Client Reviews
Nursing Home Law Center, LLC is not a law firm. It is an organization that concentrates solely on helping provide nursing home patients and their families the legal help they need. NHLC LLC has a network of recognized attorneys located across the country who have experience representing clients in all types of nursing home injury cases. References to “NHLC attorneys” or “our attorneys” are references to attorneys within NHLC’s network, and not employees, agents, or partners of NHLC. Please consult the disclaimer page for further information concerning NHLC. All information on this site shall be considered ‘attorney advertising’ and not construed as legal advice. Prior case results should not be relied on when retaining a lawyer.
You May Like: Does Stomach Ulcer Cause Pain
Data Extraction And Analysis
Two reviewers independently extracted data from included studies. The following data were abstracted: basic research features , characteristics of participants , features of pressure ulcers , features of dressings used for pressure ulcers , evaluation of dressing effectiveness . Whenever the data were missing, the authors were contacted via email. In the case of Hondé et al.s study , we were not able to verify the authors email addresses.
The data extraction was carried out in line with PRISMA guidelines. The main result of this meta-analysis was regarding the effectiveness of hydrocolloids compared to the other therapeutic interventions used in the treatment of pressure ulcers. To assess this, the number of pressure ulcers cured was analyzed. This result was taken into account either as the percentage of participants whose pressure ulcers were healed at the last control checkpoint or as the percentage of all persons successfully treated with pressure ulcers. Next, the incidence of pressure ulcers among the participants was assessed. In the analysis, the number of pressure ulcers was determined, taking into account their location and stage according to the pressure ulcer classification scale chosen by the papers authors. The final stage of the study was to assess the healing time of the wound, the frequency of dressing changes, and the duration of dressing wear.
What Types Of Wound Dressing Can Be Used On Bed Sores
By Nursing Home Law Center
In order for bed sores to heal, attention must be paid to the removing dead tissue and protecting the wound from infection causing bacteria. Dressings are usually applied to help the body heal itself. The type of dressing and the frequency with which it is to be changed is ordered by a physician with the application and changes carried out by nurses.
Many patients with bed sores suffer additional harm when the staff responsible for caring for them fails to follow medical orders with respect to the frequency with which dressings are to be changed. If dressings are not changed according to orders set forth by a physician, the healing of the bed sores may be delayed and perhaps become infected.
The most commonly used dressings used to treat bed sores include:
Absorptive Dressings: These dressings are either applied directly to the wound or on top of other primary dressings. Absorptive dressings are intended to remove the drainage from the bed sore that may impede healing. Most absorptive dressings are changed on a daily basis. However, excessive drainage from a bed sore may require more frequent dressing changes.
Common types of Absorptive dressings include: Medipore, Silon Dual Dress, Aquacel Hyrofiber Combiderm, Absorbtive Border, Multipad Soforb, Iodoflex, Tielle, Telefamax, Tendersorb, Mepore and Exu-dry.
Call Toll-Free for a No Obligation ConsultationCall Toll-Free for a No Obligation Consultation
Related Information
You May Like: Is Ulcerative Colitis An Inflammatory Bowel Disease
Cost And Quality Of Life Data
Cost and quality of life data used in the studies were also generally poor quality or lacking. When quality of life measures were reported they tended to be linear analogue scales or simple Likert-type scales. The inclusion of more sophisticated measures of quality of life when evaluating dressings is an area that needs to be tackled. This is particularly important as it may be one of the few ways to distinguish between dressings. The impact of venous ulcers on quality of life has been studied, but within randomised controlled trials quality of life data were very poor or omitted altogether.
The poor reporting of cost data was a particular concern. Where such data were collected,w7w14w29 the reporting did not conform to rigorous guidelines for economic evaluations. The trials simply totalled the monetary cost of the dressings and did not examine their cost effectiveness. This was illustrated in the hydrocolloid versus alginate comparison, where costs were reported for the interventions but insufficient detail was provided on their derivation.
Contributions Of Editorial Base:
Nicky Cullum: edited the protocol advised on methodology, interpretation and protocol content. Approved the final protocol prior to submission. Sally BellSyer: coordinated the editorial process. Advised on methodology, interpretation and content. Edited the protocol. Ruth Foxlee: designed the search strategy and edited the search methods section.
You May Like: Remicade Infusion For Ulcerative Colitis
Sacral Decubitus Ulcers Are A Certain Type Of Wound Located On The Lower Back At The Bottom Of The Spine
How to measure a sacral wound. Clock terms can also be used to describe the location of undermining. Use the body as a clock when documenting the length, width, and depth of a wound using the linear method. The braden risk assessment scale can be utilized to assess a patientâs risk of developing a pressure ulcer.
Get the wound depth using a cotton pledget or applicator dipped in a normal saline solution to measure the deepest part of the wound bed. Look closely at the wound and its edges, and then draw the wounds shape. Measure the wound how to measure wound size consistency is key.
Any adult who scores lower than 18 on the braden scale is high risk. For example, you might use words like jagged, red, puffy, or oozing to describe the wound.step 2, use a ruler to measure the length. Remove the applicator and hold it against the ruler to measure the depth of the wound margin based on.
This is particularly important when The total amount of tissue debrided should be listed separately from the wound measurements The six approaches for measuring wound area were simple ruler method , mathematical models , manual planimetry , digital planimetry , stereophotogrammetry and digital imaging method .
Step 1, draw the shape of the wound and write a brief description. Assessing and measuring wounds you completed a skin assessment and found a wound. In all instances of the linear method, the head is at 12:00 and the feet are at 6:00.
Archives Of Plastic Surgery
How The Intervention Might Work
The principle of moist wound healing governs wound care practice today. This is optimised through the application of occlusive or semiocclusive dressings and preparation of the wound bed . Animal experiments performed 50 years ago suggested that acute wounds healed more quickly when their surface was kept moist, rather than being left to dry and to scab . Winter 1962 examined the rate of epithelialisation in experimental wounds cut into the skin of healthy pigs, comparing wounds with a natural scab exposed to the air against wounds that were covered with polythene film. He found that epithelialisation occurred more quickly in the latter.
The principle of moist wound healing has led to the development of several commercially available wound dressings to support optimal healing processes. These have revolutionised wound management products include hydrogels that retain moisture in contact with the wound, hydrocolloids that absorb small amounts of excess moisture without drying the wound bed, absorbent foams, alginates, adhesive dressings, nonadhesive dressings and siliconebased lowadherent dressings. Hydrocolloid dressings are composed of a layer of sodium carboxymethylcellulose bonded onto a vapourpermeable film or foam pad. These occlusive dressings absorb exudate whilst maintaining a moist wound environment. Fibrous hydrocolloids are a subset of dressings that are designed for use in wounds with heavy exudate in lieu of alternate dressing types such as alginates .
Also Check: How Can Decubitus Ulcers Be Prevented
Implications For Current Practice And Future Research
Hydrocolloid dressings have been widely used in clinical practice since the early 1980s. Differing in structure and function, they still meet the criteria for an absorbent dressing that adheres well and protects the wound from external factors and provides a warm and moist environment that promotes better wound healing. By absorbing water and low molecular weight ingredients, hydrocolloids form a characteristic gel that stimulates the immune system and reduces the effects of bacterial colonization . Clinical studies of hydrocolloids on more than 2000 pressure ulcers have shown a significantly lower incidence of infections than in the case of other treatments . These are the most common advantages of using hydrocolloid dressings compared to conventional methods.
Currently available evidence is insufficient to assess whether any dressing or topical treatment increases the likelihood of pressure ulcer healing more than others and to assess whether there is a negative relative effect on wound healing or not. None of the interventions appear to heal more wounds than others . For this reason, according to some researchers, when choosing a suitable dressing, clinicians should take into account wound symptoms, clinical experience, patient preference, and the cost of intervention .
Diagnosing A Stage 3 Bedsore
A medical professional relies on a bedsores appearance to diagnose its stage.
Stage 3 bedsores have the following characteristics:
- Black or rotten outer edges
- Crater-like indentation
- Dead, yellowish tissue
- Visible fat tissues
Stage 3 bedsores are quite deep, but tendons, ligaments, muscles, and/or bones will not be visible. If they are, the patient likely has a stage 4 bedsore. That said, health care providers may not be able to properly stage every severe bedsore.
Two complications may delay a stage 3 bedsore diagnosis:
- Deep tissue injuries: A deep tissue injury occurs when there is no open wound but the tissues beneath a patients skin are damaged.
- Unstageable injuries: If a doctor cannot see the base of the sore due to slough or eschar in the wound bed, they cannot make a diagnosis.
Even if a bedsore cannot be staged, doctors can still recommend treatments to start the healing process.
Donât Miss: Whatâs The Signs Of An Ulcer
Also Check: What To Do For A Peptic Ulcer
Which Wound Dressing Is Best For Your Pressure Ulcer
Now that weve touched on some of the more common types of dressings used for pressure ulcers, you may be wondering which is the best for your particular situation. The answer will depend on multiple factors including where the pressure ulcer is located, how severe the bedsore is, and the degree of skin and tissue damage. Talk to your health care professional about any pressure wounds you notice on your body as soon as possible.
Compare With Similar Items
| This item JJ CARE Hydrocolloid Dressing , 2×2 Hydrocolloid Bandages w/Border, Self-Adhesive Hydrocolloid Wound Dressing, Faster Healing for Bedsores, Blisters, and Acne | |||||
|---|---|---|---|---|---|
| 4.4 out of 5 stars | 4.4 out of 5 stars | 4.5 out of 5 stars | 4.6 out of 5 stars | 4.4 out of 5 stars | |
| Price | $14.95$14.95 | ||||
| Shipping | FREE Shippingon orders over $25.00 shipped by Amazon or get Fast, Free Shipping with | FREE Shippingon orders over $25.00 shipped by Amazon or get Fast, Free Shipping with | FREE Shippingon orders over $25.00 shipped by Amazon or get Fast, Free Shipping with | FREE Shippingon orders over $25.00 shipped by Amazon or get Fast, Free Shipping with | FREE Shippingon orders over $25.00 shipped by Amazon or get Fast, Free Shipping with |
| Sold By |
Also Check: Quantitative Research On Pressure Ulcer Prevention
Criteria For Considering Studies For This Review
Types of studies
We included published and unpublished randomised controlled trials , irrespective of language of report. We did not identify any crossover trials, but we would have included them only if they reported outcome data at the end of the first treatment period and prior to crossover. We excluded studies using quasirandom methods of allocation . We highlighted trials in which three or more interventions were randomised.
Types of participants
We included studies that recruited people with a diagnosis of pressure ulcer, Stage 2 and above , managed in any care setting. We excluded studies that only recruited people with Stage 1 ulcers as these are not open wounds requiring dressings.
We accepted study authors’ definitions of what they classed as Stage 2 or above, unless it was clear that they included wounds with unbroken skin. Where authors used grading scales other than NPUAP, we attempted to map to the NPUAP scale.
Types of interventions
Interventions of direct interest
The interventions in this section were all those that can be directly applied as dressings or topical agents to open pressure ulcers. We presented results for these interventions and included them in summary tables. In the context of a network of competing treatments, there are no ‘comparators’.
Some of the interventions we considered were as follows:
Supplementary intervention set
Terminology
Types of outcome measures
Primary outcomes
- the proportion of wounds healed
- time to complete healing .
Assessment Of The Risk Of Bias In The Included Studies
The risk of bias in the included studies was assessed using a standardized critical appraisal instrument developed by the Cochrane Collaboration , which covers the following seven evaluation aspects: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. The bias was presented as the number of points of low risk of bias assessment.
Also Check: Ulcerative Colitis Flare Up Treatment Guidelines