Signs And Symptoms Of Leg Ulcers
The most common symptoms that accompany leg ulcers are as follows:
- Swelling of the ankles
- Irritated or flaky skin
- Skin begins to harden and scale around the ulcers
These symptoms often vary in their severity. Although most leg ulcers usually disappear in a few days, some may be non-healing. It is always better to try and heal leg ulcers as soon as you can to prevent further complications. For that, you need to diagnose them first. The following are a few most common techniques used to diagnose leg ulcers.
How Do I Take Care Of My Foot And Toe Ulcers
Your healthcare provider might teach you how to care for your ulcers at home. You might be instructed to:
- Wash the affected area with mild soap.
- Keep the wound clean and dry.
- Change the bandages as directed.
- Take prescribed medications as directed.
- Drink plenty of fluids. Ask your healthcare provider how much water you should drink every day.
- Follow a healthy diet, as recommended by your healthcare provider.
- Exercise regularly, under your healthcare providers care.
- Wear appropriate shoes.
- Wear compression wraps as directed.
Getting A Specialist Vascular Referral
If you have venous hypertension / insufficiency, intervention to your veins might help with healing and stop your wound or sore from coming back. Sometimes varicose veins can be treated by laser therapy. But if you have peripheral arterial disease, you may require further investigations and the vascular team will be able to assess the need to improve the blood supply to your leg or whether your ulcer can be managed in other ways such as reduced / modified with compression.
Ask your nurse or GP for a referral to your local vascular team to talk about how their input might help you.
Also Check: Is Oatmeal Good For Ulcerative Colitis
What Are My Treatment Options
Treatment will depend on many factors, including the reason for the condition and your health status and history. Other factors your doctor will consider are:
- Your specific symptoms.
- How severe your condition is.
- How well you can tolerate medications or procedures.
The most common treatment for venous insufficiency is prescription-wear compression stockings, she says. These special elastic stockings apply pressure at the ankle and lower leg. They help improve blood flow and can reduce leg swelling.
You also can improve blood flow by keeping your legs elevated whenever possible, which means keeping them uncrossed when you are seated and by exercising regularly.
If you need medication, the most commonly prescribed include:
- Diuretics. These medications draw extra fluid from your body through your kidneys.
- Anticoagulants. These medications thin the blood.
- Pentoxifylline . This medication helps improve blood flow.
Getting Diagnosed With A Leg Ulcer
If you have a wound or sore that isnt healing, make an appointment at your GP practice as it could turn into or be the beginnings of a leg ulcer. You might be given an appointment to see the nurse rather than the doctor as nurses are often responsible for caring for patients with leg problems.
Alternatively, there might be a Leg Club or specialist leg clinic in your area. You can attend these without having to be referred by your GP.
Remember to remove any nail polish from your toenails before your appointment.
When you see the nurse or doctor, they should:
- Ask about your symptoms and how long you have had problems
- Examine your lower legs
- Do a simple test called a Doppler ultrasound. This test compares blood flow in your ankle with that in your arm to find out if there are blood flow problems in your lower leg. You may have to come back to have your Doppler test on another day or at another clinic.
You may also be offered some other tests to check for other health problems that can affect your legs such as diabetes and anaemia.
If your GP practice thinks you have problems with your veins or arteries, they may refer you for more tests at your local hospital or specialist clinic.
You may hear different words to describe your wound such as ulcer, leg ulcer, sore, laceration, chronic wound and maybe others. Ask your nurse to explain their choice of word and what this may mean for you.
Don’t Miss: What Should You Eat When You Have Ulcerative Colitis
Causes Of Venous Ulcers
Venous ulcers most often form around the ankles.
Venous ulcers typically occur because of damage to the valves inside the leg veins. These valves control the blood pressure inside the veins. They allow it to drop when you walk. If the blood pressure inside your leg veins doesn’t fall as you’re walking, the condition is called sustained venous hypertension. That increase in blood pressure causes ulcers to form on your ankles.
Venous ulcers may also be caused by other problems with your leg veins. These include:
-
Varicose veins. These are large, bulging leg veins. They occur when valves in the leg veins dont work well, allowing blood to collect in the lower leg.
-
Chronic venous insufficiency. Like varicose veins, this condition occurs when your leg veins cant pump blood back up to your heart. Blood then pools in your lower legs, causing your legs to swell. Since the blood can’t flow well in your legs, the swelling may be extreme. This extreme swelling can put so much pressure on your skin that venous ulcers form.
Other Types Of Leg Ulcer
Other common types of leg ulcer include:
- arterial leg ulcers caused by poor blood circulation in the arteries
- diabetic leg ulcers caused by the high blood sugar associated with diabetes
- vasculitic leg ulcers associated with chronic inflammatory disorders such as rheumatoid arthritis and lupus
- traumatic leg ulcers caused by injury to the leg
- malignant leg ulcers caused by a tumour of the skin of the leg
Most ulcers caused by artery disease or diabetes occur on the foot rather than the leg.
Page last reviewed: 11 January 2019 Next review due: 11 January 2022
Also Check: Over The Counter Mouth Ulcer Treatment
Venous Ulcer Diagnosis And Treatment
Doctors at Vascular surgeons at UPMC’s Heart and Vascular Institute use duplex ultrasound, a noninvasive test, to diagnose abnormal veins that cause venous ulcers. Part of the UPMC difference is that we actively look for the causes of the ulceration to treat venous pathology and keep the ulcer healed.
After an evaluation of your veins, we recommend a treatment plan based on your needs:
- Compression of the leg is vital to healing venous wounds.
- Compression stockings are most commonly used for this treatment.
- The pressure from the compression dressing counteracts the pressure from the veins of the leg and allows skin to heal.
Treatment What Treatment Will I Be Offered For My Leg Ulcer
If your wound isnt healing because of venous hypertension and there are no problems with the blood supply to your legs, then you should be offered compression therapy.
Compression therapy improves blood supply by applying pressure to the leg. This can be done by bandaging the lower leg or by wearing supportive socks, stockings or tights. Compression therapy is very effective at reducing swelling, improving blood flow in the veins and healing or preventing sores or ulcers.
There are lots of different types of compression therapy so ask your nurse to find something that is right for you.
Compression can be a little uncomfortable when you first start treatment but should not cause you any pain. Any discomfort should reduce as the swelling goes down. If you do experience discomfort, talk to your nurse or doctor about it and they will advise you on ways of alleviating this.
In addition to the compression, your nurse should also advise you on wound care and dressings to keep your wound healthy.
You May Like: Exercising A Horse With Ulcers
Research On The Best Treatment For Venous Leg Ulcers
In the short term, a venous leg ulcer should be managed by a specialist team experienced in cleaning and dressing the ulcer and in this way, the ulcer can be healed by using compression, such as bandages or stockings. This specialist team may be attached to a GP surgery. Most GP surgeries have a leg ulcer nurse supported by healthcare assistants.
In the longer term, the underlying vein problem should be identified by a Duplex Ultrasound Scan and if superficial venous reflux is found, it should be treated.
Vein treatments for venous leg ulcers caused by superficial venous reflux can nowadays be carried out very safely under local anaesthetic as a walk in, walk out non-invasive procedure and the age of the person with a leg ulcer is no longer a barrier to effective treatment. Once an ulcer is healed and the underlying vein problem is addressed, under the guidance of a healthcare professional and provided there are no other health issues such arterial disease or diabetes, the risk of the ulcer returning can be reduced by wearing good quality medical-grade compression hosiery.
How long will it take the ulcer to heal?
The Latest Research On The Best Way To Heal Leg Ulcers
In total, 450 people agreed to take part in this study and were treated in 20 hospitals across England. Participants were randomly allocated to either early or delayed endovenous ablation and followed up for 12 months. The trial found that treating the veins early resulted in quicker ulcer healing than delaying treatment until the ulcer had healed. The trial also showed that participants had more time without an ulcer if the treatment was performed early rather than after ulcer healing. No safety issues with early intervention were identified. There is some evidence that quality of life was better in the early treatment group and that people in this group had less body pain. Treating ulcers early appears likely to be more cost-effective than delayed treatment.
This research was published 2 years ago but unfortunately, a survey published 6 months ago suggests that the UK has significantly longer referral times, longer waiting times to secondary care and longer times to intervention than other countries. This is supported elsewhere where it is suggested that the UK is possibly undertreating patients with chronic venous disease. This may relate to relative constraints of the National Health Service compared to other privatised health care systems globally.
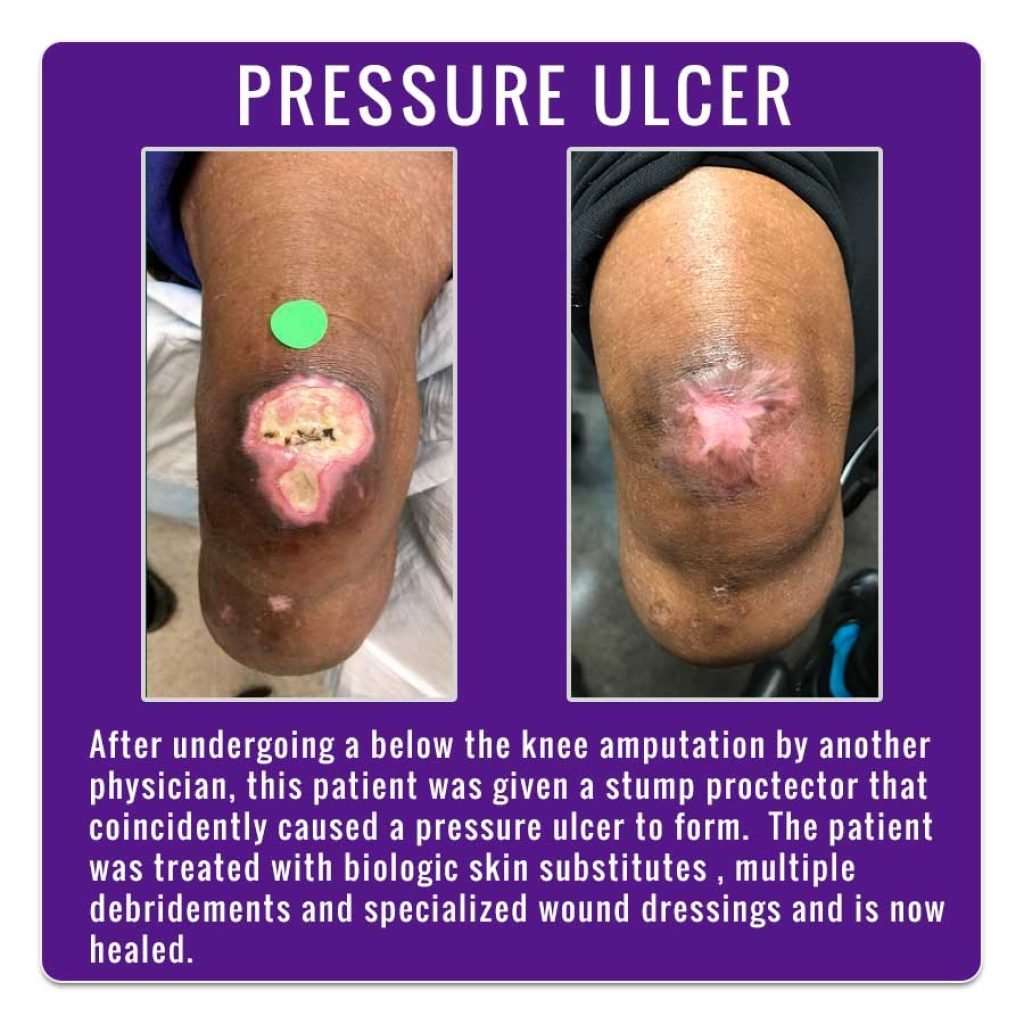
Recommended Reading: Mepilex Dressing For Pressure Ulcer
Split Thickness Skin Graft
This method is used for large ulcers under general, spinal, or extensive local anaesthesia. These grafts are usually successful, but the grafts may contract after harvesting and need a large donor site, which may be slow to heal and cause a lot of pain. In grafting large leg ulcers, graft failure may occur because of build-up of exudate underneath the graft this is best avoided by the use of a meshed graft.
Ulceration Due To Dermatitis Artefacta
Ulceration secondary to artefact may be difficult to diagnose. Clinical suspicion might be raised by the following: unusual appearance, unusual site, after trauma at work with possible compensation issues, angulate shape or the apparent indifference of the patient to their ulcer and its implication to their life. If the ulcer tends to come and go, a skin biopsy may be necessary to show up out-side-in damage, that is, disproportionate damage to the epidermis compared with the dermis.
Don’t Miss: What Are The Symptoms Of Ulcerative Colitis
When Should I See My Healthcare Provider About Foot And Toe Ulcers
If you have diabetes, its important to see a podiatrist regularly. Whether you have diabetes or not, you should see a healthcare provider immediately if you find an ulcer on your foot or toe. Left untreated, it could get infected, leading to complications like amputations.
A note from Cleveland Clinic
It can be distressing to discover an open sore on your foot or toe. You might not know what caused it, it might not be healing and, if you have neuropathy from diabetes, you might not even feel it. Keep in mind that your healthcare provider can successfully treat your ulcer, especially if its found early. If left untreated, an ulcer can lead to serious complications.
If you have neuropathy caused by diabetes, remember that its important to check your feet and toes on a regular basis. Check your toes and feet every time you shower or when you go to put on your shoes. Contact your healthcare provider right away if you find an ulcer.
Side Effects Of Leg Ulcers
- A green and foul-smelling discharge from the ulcers
- The skin around the ulcers begins to swell
- The sores become bigger
- Inflamed skin around the ulcers
Leg ulcers resemble sores that develop when bacteria enter underlying tissues through injured or broken skin. While skin injuries are the most common risk factor for leg ulcers, certain underlying medical conditions like diabetes, arterial disease, and venous disease may also lead to leg ulcers. Some common signs and symptoms that often accompany leg ulcers include irritated or flaky skin, swelling, heaviness, discoloration, and leg pain on prolonged standing. You may use natural ingredients like Gotu kola, turmeric, aloe vera, coconut oil, tea tree oil, and yarrow in home remedies to heal leg ulcers in mild to moderate cases.
Don’t Miss: How Fast Does Humira Work For Ulcerative Colitis
Clinical Manifestations Healing And Consequences
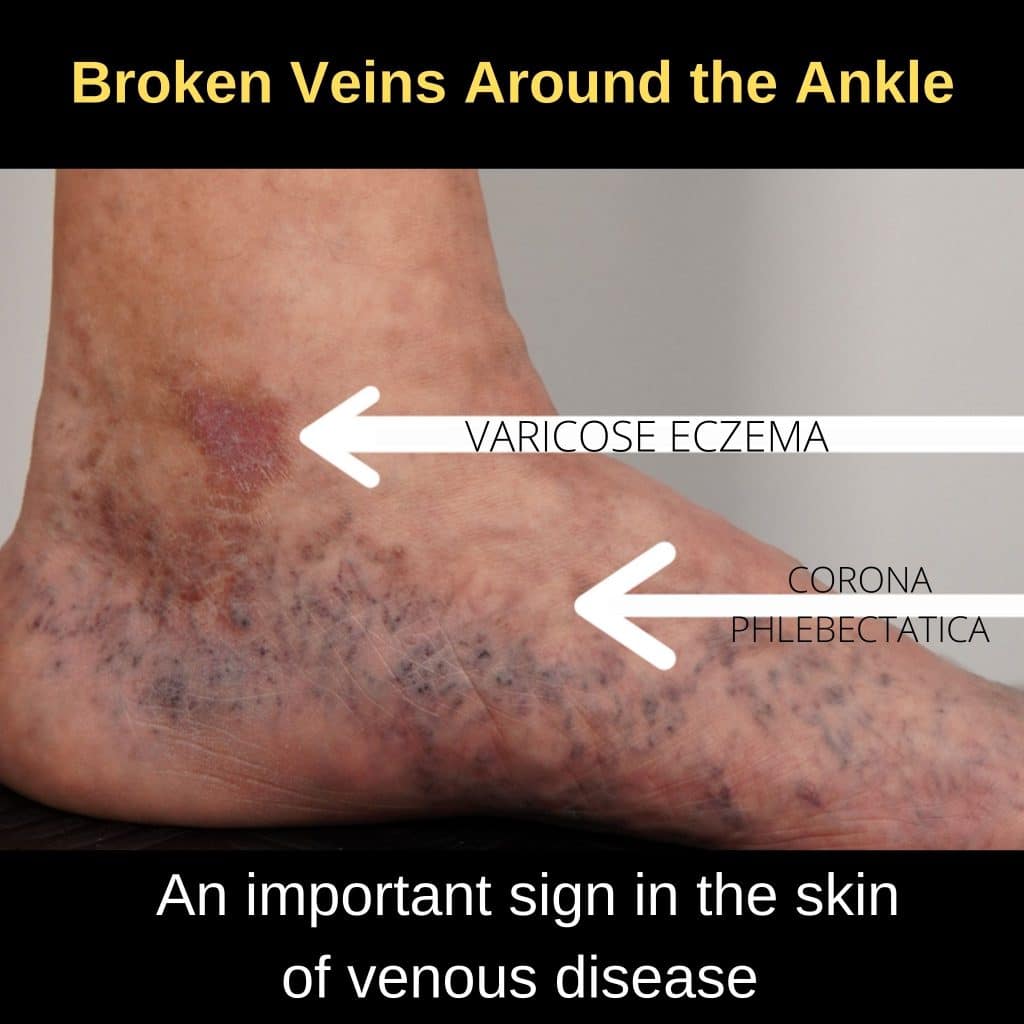
CVD includes a spectrum of clinical manifestations ranging from telangiectases and reticular veins to skin changes, such as lipodermatosclerosis and VLU. Varicose veins are among the first clinical evidences of CVD. They are enlarged superficial veins that progressively become twisted and dilated. Edema is the first sign of CVI. It appears as fluid accumulation starting from the perimalleolar ankle area to the upper side of the leg. Skin changes, due to red blood cell extravasation, hemosiderin deposition, iron overload, and inflammatory and fibrotic processes, are represented by hyperpigmentation, eczema, atrophie blanche, and lipodermatosclerosis .
VLU is the result of the pathological changes developed inside vessels after a prolonged condition of CVI. As the culminating complication of CVI, VLU is accompanied by several clinical manifestations of the underlying disease.
Other clinical features of CVI are generally present, including varicose veins, edema, dermatitis, telangiectasias and reticular veins, hemosiderin pigmentation, lipodermatosclerosis, and atrophie blanche. These clinical manifestations provoke patients suffering, swelling, leg pain, pruritus, pain, or nocturnal cramps .
Chronic VLUs provide a fertile breeding ground for the onset of several complications, ranging from immobility and reduced quality of life to cellulitis, severe infections, osteomyelitis, and neoplastic transformation .
General Health Advice For Patients With Leg Ulceration
There are some lifestyle changes patients can make that will help boost healing:
- Maintaining a healthy weight
- Eating a well-balanced diet that includes 5 portions of fruit and vegetables a day and protein rich foods such as eggs, fish, chicken or pulses
- Taking light to moderate exercise such as cycling or walking for about thirty minutes at least three times a week
- Avoiding standing or sitting for long periods of time
- Putting their feet up legs to be elevated above the heart.
Read Also: Medicines Used To Treat Ulcerative Colitis
How Do I Take Care Of My Ulcers
Your healthcare provider may teach you how to care for your ulcers at home. Some instructions may include:
- Wash the affected area with mild soap.
- Keep the wound clean and dry.
- Change the bandages as directed.
- Take prescribed medications as directed.
- Drink plenty of fluids. Ask your healthcare provider how much water you should drink every day.
- Follow a healthy diet, as recommended by your healthcare provider.
- Exercise regularly, under your healthcare providers care.
- Wear appropriate shoes.
You May Like: What Should You Not Eat With An Ulcer
When To Seek Medical Care
You May Like: Can Alcohol Cause Bleeding Ulcers
Who Gets Foot And Toe Ulcers
Foot and toe ulcers can happen to many people but might be more common in Black, Native American and Hispanic people. If you have an eye, kidney or heart disease related to diabetes, youre also at a higher risk. About 15% of people with diabetes will get an ulcer, typically on the bottom of their foot. Some of those people will be hospitalized because of complications.
Youre also at a higher risk of getting foot and toe ulcers if you have any of the following conditions:
- Blood circulation issues.
If your ulcer is black, that means cells in the tissues have died. This is called necrosis .