Clinical Visit With A Rheumatologist And Hla
Among the 51 IBD patients, 39 suffered from articular pain, 20 benefited from a rheumatologist visit. From these 20 patients, 11 suffered from LBP, 9 with inflammatory LBP, and 2 with mechanical LBP. Only 1 patient with inflammatory LBP was HLA-B27 positive and presented sacroiliitis on MRE and CT scan. For the last 10 patients with LBP, HLA-B27 was negative in 2 cases, not available for 8 patients, and none presented sacroiliitis on digestive imaging.
How To Relieve Ulcerative Colitis Pain
While there is no cure for UC, there are ways to relieve the pain and reduce the inflammation you feel. Dietary modifications are one strategy to help manage the pain. Shifting to a low fiber, low residue diet can help you find relief. Incorporate more low fiber fruits such as bananas, non-cruciferous vegetables such asparagus, cucumbers, and carrots, refined grain products like white bread and white rice, and lean protein sources like chicken, fish, and eggs. Additionally, try to avoid consuming refined sugar, alcohol, caffeine, high fat foods, high fiber foods, and spicy foods.
Beyond nutrition, there are other ways to control the pain you feel. Focusing on managing your stress level can help. Yoga, meditation, and breathing exercises are some activities you can try on your own. Joining a support group or speaking to a mental health professional may help as well. Talking to your doctor about different medications to help control pain is also important.
Although Ulcerative colitis is life-long, that doesnt mean your UC pain has to be. When UC is well-managed, you can experience long periods of remission and become symptom-free. The key is to modify your approach based on the stage of your condition and learn to listen to your body. If youre having trouble managing your UC, we recommend working with a dietitian who can help you obtain and sustain remission.
Causes Of Collagenous Colitis And Lymphocytic Colitis
- infection with an unknown virus or bacterium
- problems with the immune system such as an autoimmune disorder, which means the immune system attacks a healthy part of the body by mistake. Some affected people may have autoimmune disorders such as rheumatoid arthritis, scleroderma or Sjogrens syndrome
- certain medications that may increase the risk, including non-steroidal anti-inflammatory drugs such as ibuprofen or aspirin.
Recommended Reading: Mepilex Dressing For Pressure Ulcer
Get The Latest Health Information From Mayo Clinic Delivered To Your Inbox
Read more: How to clean your Androids or iPhones charging port | Asurion
Last Name
To provide you with the most relevant and helpful information, and understand which data is beneficial, we may combine your electronic mail and web site custom information with other information we have about you. If you are a Mayo Clinic affected role, this could include protect health data. If we combine this information with your protected health information, we will treat all of that information as protect health information and will only use or disclose that data as set up forth in our notice of privacy practices. You may opt-out of electronic mail communications at any time by clicking on the unsubscribe yoke in the electronic mail .
What Are The Complications Of Ulcerative Colitis
Colon Cancer
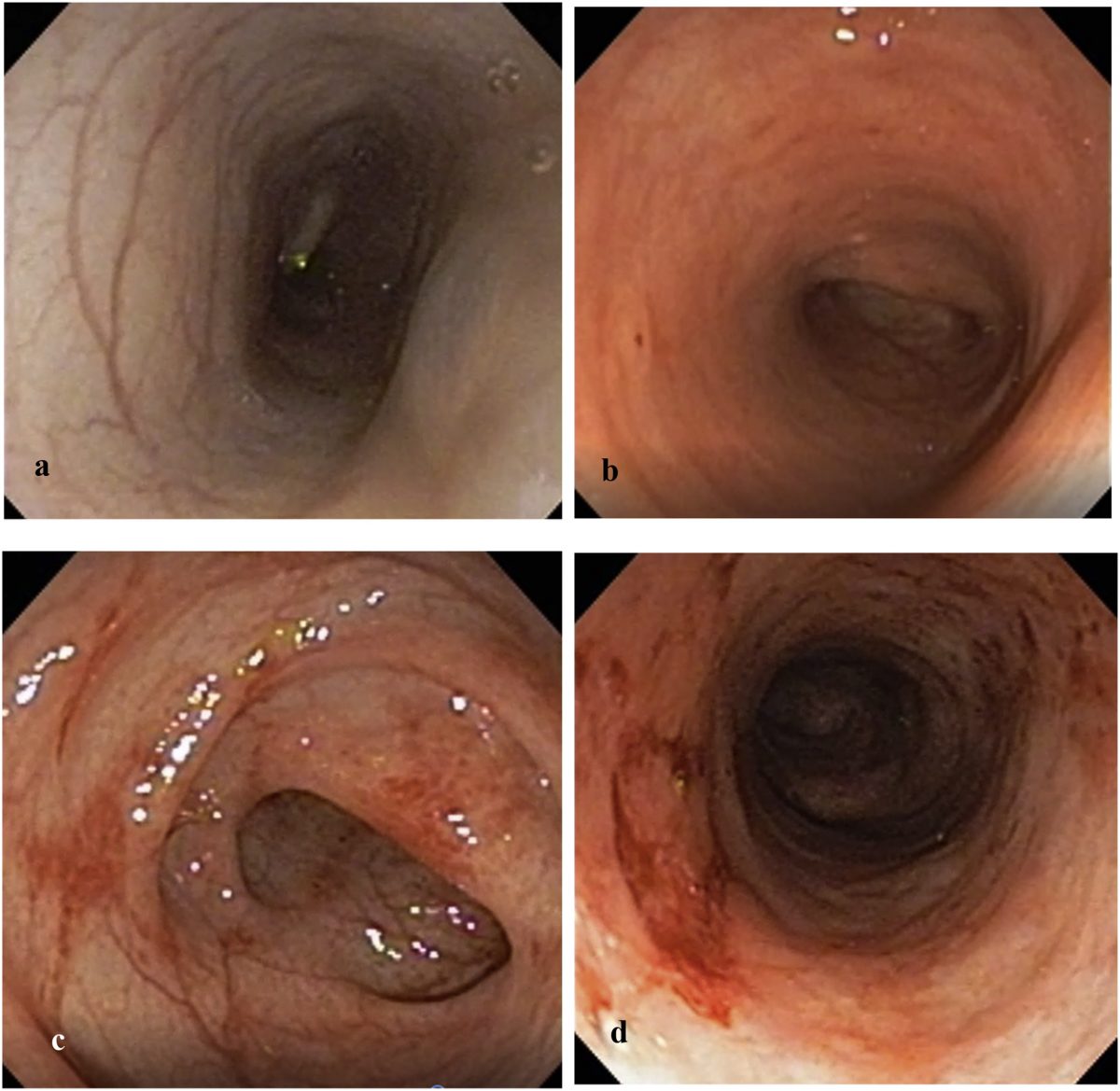
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Don’t Miss: Ulcerative Colitis How Much Blood Is Too Much
Hydrogen Sulfide The Gas
The H2S gas is made in the colon. It is a nasty customer. It is mostly what gives flatus its foul smell. We avoid the smell when we can and make fun of it. But, there is nothing funny about H2S. Consider these facts about H2S, all medically documented.
- Half the normal population makes H2S gas in their colon. The other half makes methane gas.
- However, 90-100% of ulcerative colitis patients make H2S. Thats an interesting fact, isnt it?
- H2S is a toxic gas. In higher doses, it can irritate the eyes. In even higher concentrations, it is as damaging as hydrogen cyanide. In the normal colon, there are cells that contain an enzyme that detoxifies the H2S gas.
- There is some evidence to suggest that this enzyme is deficient in ulcerative colitis patients, so that the H2S may linger and damage the colon wall.
- Most patients have ulcerative colitis in the left side of the colon where the H2S gas is mostly made.
- Certain bacteria in the left side of the colon use sulfur in our foods, water and especially in meats, to make the H2S gas.
- The good bacteria in the colon make certain acid substances, thereby acidifying the colon contents.
- Here is a possible key point. These H2S producing bacteria do not grow in an acid environment. Keeping the colon acid may be important.
When To See A Doctor
See your doctor if you experience a persistent change in your bowel habits or if you have signs and symptoms such as:
- Abdominal pain
- Ongoing diarrhea that doesn’t respond to over-the-counter medications
- Diarrhea that awakens you from sleep
- An unexplained fever lasting more than a day or two
Although ulcerative colitis usually isn’t fatal, it’s a serious disease that, in some cases, may cause life-threatening complications.
Read Also: Is Papaya Good For Ulcerative Colitis
Other Ways To Manage Pain
Medication isnt the only way to treat sacroiliitis. Exercise is also an important part. Moderate-intensity aerobic exercises like walking, bike riding, and swimming help to lessen pain and improve movement.
Physical therapy helps, too. A physical therapist can teach you range-of-motion exercises to stretch your sacroiliac joints and strengthen the muscles around them.
When your back hurts, try holding a cold pack or heating pad to the area. Use whichever one feels best, or go back and forth between warmth and cold.
Rest when you need to, and avoid any activities that worsen pain.
Show Sources
Annals of the Rheumatic Diseases: AB1293 Incidence of sacroiliitis in inflammatory bowel disease: a single-centre study from Tianjin, China.
Arthritis Care & Research: Prevalence of Sacroiliitis in Inflammatory Bowel Disease Using a Standardized Computed Tomography Scoring System.
Cleveland Clinic: Sacroiliitis.
Gastroenterology Research and Practice: Management of Musculoskeletal Manifestations in Inflammatory Bowel Disease.
Inflammatory Intestinal Diseases: Low Back Pain and Sacroiliitis on Cross-Sectional Abdominal Imaging for Axial Spondyloarthritis Diagnosis in Inflammatory Bowel Diseases.
Journal of Crohns and Colitis: The joint-gut axis in inflammatory bowel diseases.
Mayo Clinic: Sacroiliitis.
Medscape General Medicine: Extraintestinal Manifestations of Inflammatory Bowel Disease: Focus on the Musculoskeletal, Dermatologic, and Ocular Manifestations.
What Happens If You Dont Treat Colitis
Colitis is usually a temporary condition that resolves on its own in a few days to a week. It can, however, be a sign of a more serious condition such as ulcerative colitis, Crohns disease, autoimmune disorders, metabolic disorders, circulation problems, heart problems, or radiation injury. It can also be a sign of a serious infection, such as a potentially fatal E. coli gut infection or amoebic dysentery. If the symptoms become severe or last longer than a week, its time to talk to a doctor.
Recommended Reading: What Happens When You Have A Bleeding Ulcer
Sex Pregnancy And Ankylosing Spondylitis
Sex may be painful if you have ankylosing spondylitis. If it is, try taking some painkillers beforehand and experiment with different positions.
Ankylosing spondylitis can make you feel tired, so its important your partner understands how your condition affects you. Good communication can help you maintain an active sex life and counselling can sometimes benefit both partners.
Its fine to use the contraceptive pill if you have ankylosing spondylitis, but you should tell your doctor youre taking it.
If youre thinking of starting a family, its very important for both men and women with ankylosing spondylitis to discuss medication with a doctor beforehand.
Some drugs such as methotrexate should be stopped several months before a woman tries to get pregnant. Latest research suggests its safe for men to take methotrexate when trying for a baby with their partner.
Biological therapies seem to be safe in the earlier stages of pregnancy but are then stopped later in pregnancy.
If you become pregnant while using a conventional DMARD such as methotrexate or a biological therapy, discuss this with your rheumatology team as soon as possible.
Usually, pregnancy doesnt cause any special problems for the mother or baby, though the symptoms of ankylosing spondylitis may not ease during pregnancy. If your spine is very stiff, it may not be possible to have an epidural during childbirth. This is an injection into the back that stops people feeling pain in part of the body.
Ulcerative Colitis Treatments And Drugs Mayo Clinic
Posted: July 12, 2016 at 5:17 am
This post was added by Dr Simmons
Ulcerative colitis treatment usually involves either drug therapy or surgery.
Several categories of drugs may be effective in treating ulcerative colitis. The type you take will depend on the severity of your condition. The drugs that work well for some people may not work for others, so it may take time to find a medication that helps you. In addition, because some drugs have serious side effects, you’ll need to weigh the benefits and risks of any treatment.
Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel disease. They include:
Corticosteroids. These drugs, which include prednisone and hydrocortisone, are generally reserved for moderate to severe ulcerative colitis that doesn’t respond to other treatments. They are given orally, intravenously, or by enema or suppository, depending on the location affected.
Corticosteroids have numerous side effects, including a puffy face, excessive facial hair, night sweats, insomnia and hyperactivity. More-serious side effects include high blood pressure, diabetes, osteoporosis, bone fractures, cataracts, glaucoma and increased chance of infection. They are not usually given long term.
Immunosuppressant drugs include:
You may need additional medications to manage specific symptoms of ulcerative colitis. Always talk with your doctor before using over-the-counter medications. He or she may recommend one or more of the following.
Read Also: What Is The Best Thing To Put On Leg Ulcers
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Preparing For Your Appointment
Symptoms of ulcerative colitis may first prompt you to visit your elementary wish doctor. Your sophisticate may recommend you see a specialist who treats digestive diseases .
Because appointments can be brief, and there s often a set of information to discuss, it s a good idea to be well prepared. here s some information to help you get quick, and what to expect from your sophisticate .
You May Like: What To Eat With Gastric Ulcer
Ulcerative Colitis Questions: Confused And Frustrated
I have been navigating a UC diagnosis for about the last 6 months. Previously the stool bleeding was diagnosed as hemmeroidal, but things continued to progress until a colonoscopy revealed serious inflammation in the colon. After a grade 3 diagnosis, the doctors pushed for humira. I tried a very strict, anti-inflammatory diet first, and it helped a lot. Still a little blood in the stool tho. So tried mesalamine both oral and the suppository. I thought things were improving using b, as the color I saw in the stool was purple rather than red, but doctors said it was still blood and pushed again for humira. I took their advice and am now approaching the 7th injection. I have more bleeding now than ever and I have abdominal pain and urgency. I am definitely in the middle of one of my worst flareups. Anyone out there have a similar story and advice? I’m feeling confused and frustrated.
Hello @psdoolittle, welcome to Mayo Clinic Connect. Has your doctor offered any suggestions or have you thought about seeing a specialist?
Hello @psdoolittle, welcome to Mayo Clinic Connect. Has your doctor offered any suggestions or have you thought about seeing a specialist?
You need a continuum of care, which won’t happen with seeing a different doctor every time. I’d go somewhere else.
Certain Foods Can Trigger Uc Symptoms In Some People
Has ulcerative colitis made you hesitant to eat for fear of causing painful symptoms? If you know for sure what foods make you feel worse, it’ll be easier to live with the disease. A review published in April 2019 in the journal Current Treatment Options in Gastroenterology noted that people with inflammatory bowel disease who had a diet full of fiber from fruits and vegetables, and low in animal fats, dairy, and processed food, had the fewest flares and best health outcomes. Doctors and nutritionists recommend that people who are diagnosed with ulcerative colitis change their dietary intake to ensure that they are consuming much-needed nutrients without exacerbating symptoms.
Whats the best way to identify what not to eat if you have UC? According to the research review mentioned above, starting an elimination diet for patients with Crohns disease or UC allowed 73 percent of patients to achieve remission in a six-week period. . Elimination diets, where patients remove certain foods from their diet to see if their symptoms abate, are a good way to identify common food triggers.
To get started on one, record all the food you eat during the day in a diary or journal along with any symptoms you experience. You can do this with pen and paper or with phone apps.
Recommended Reading: How Do You Diagnose An Ulcer
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
My Experience With Severe Pain In My Back
In 2008, I had such severe back pain I couldnt walk. I tried to go to school but needed my dad and male friends to literally carry me into class. It came on suddenly and was just so random to me.
I went to a ton of doctors, went through a lot of tests, physical therapy, acupuncture, etc. Nothing showed up and nothing helped. At my last appointment with an orthopedist, the doctor told me he had been thinking about my case for a while in between the tests and visits to other specialists. He even brought in colleagues to try and help him figure things out.
The conclusion was that there was nothing structurally wrong with my back. He believed the intense pain I was experiencing was from all of my abdominal surgeries. He thought my stomach muscles were so weak that it forced my back to pick up the slack, so to speak.
While this made sense, I had no idea what to expect for the future. Was this just how it was now? Did I just have to accept I would be this way forever?
You May Like: Surgical Management Of Ulcerative Colitis Ppt
Don’t Miss: What Are Ulcers Caused From
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.