The High Cost Of Emergency Care
The emergency room also costs a ton of money. I know people shouldnt be thinking about that when it comes to their health but chronic illness is expensive. It is difficult not to weigh the pros and cons of going to the emergency room when you are already in a pile of medical debt that is stressing you out.
Lastly, being alone while in a crisis is hard enough but when your disease impacts your stomach it makes it that much more challenging. People are in such a vulnerable place and oftentimes it is difficult for people to let medical professionals know the complete picture of what is going on. Being overwhelmed can often make you sound incoherent or babbly which is the last thing doctors and nurses are looking for when trying to care for you.
I wish there were IBD-specific emergency rooms. I know that is a pipe dream but I just want most people in the medical field, as well as the general public, to really understand how difficult it is to bring yourself to the ER. It takes a tremendous amount of courage to admit you need help especially when you cant predict what you will be walking into when you go to the emergency room.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Recommended Reading: Foam Dressing For Pressure Ulcer
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Diagnosis And Tests For Ulcerative Colitis
Ulcerative colitis can usually be controlled, so make an appointment to see your GP. If your GP thinks you may have an inflammatory bowel disease ie ulcerative colitis or Crohns disease, they will refer you to a gastroenterologist .
Your doctor will carry out a physical examination of your abdomen to check for tenderness, which is caused by inflammation. They will also check if you are pale, which can be a sign of anaemia. You may need an X-ray or CT scan to rule out other more serious complications.
They may ask you to collect a stool sample for testing to rule out gastroenteritis , which has similar symptoms to ulcerative colitis. In some cases, an infection can trigger a flare-up of ulcerative colitis and treating the infection can ease your symptoms.
Your doctor may also recommend blood tests to check for anaemia and inflammation anywhere in your body and/or a biopsy where a small sample of tissue from your bowel is collected to check for bowel inflammation.
A biopsy can be collected during one of two different procedures:
A thin, flexible tube with a camera on the end is inserted into your rectum to examine it and your lower colon, and if needed, collect a tissue sample. This is an outpatient procedure, so you can go home the same day, and it takes around 15 minutes. You will be awake, however, you can have a sedative to relax you.
You May Like: How Do You Prevent Pressure Ulcers
Ulcerative Colitis: Sheas Story
Shea suffered ups and downs in her health from ulcerative colitis until treatment at Childrens Hospital of Philadelphia helped her turn the corner. Now 9, Shea finally has her energy back and revels in her favorite activity cheerleading.
Shea was 6 when she started showing signs of sickness. It started with occasional bouts of bloody diarrhea, and then she started getting stomach cramps. Shea started to look pale, acted lethargic and was losing weight.
She did a lot of crying, her mother, Miranda, remembers. Sometimes Id just sit and cry with her. Her local pediatrician in Lehigh Valley, PA, couldnt figure out the cause.
One day, Shea was feeling extremely weak. She didnt even think she could make it down the steps without falling, so her parents took her to the emergency room at their local hospital. Shea was diagnosed with anemia and admitted for treatment with iron infusions. When her stomach pains and diarrhea continued, doctors performed a colonoscopy. The scope led to a diagnosis of ulcerative colitis.
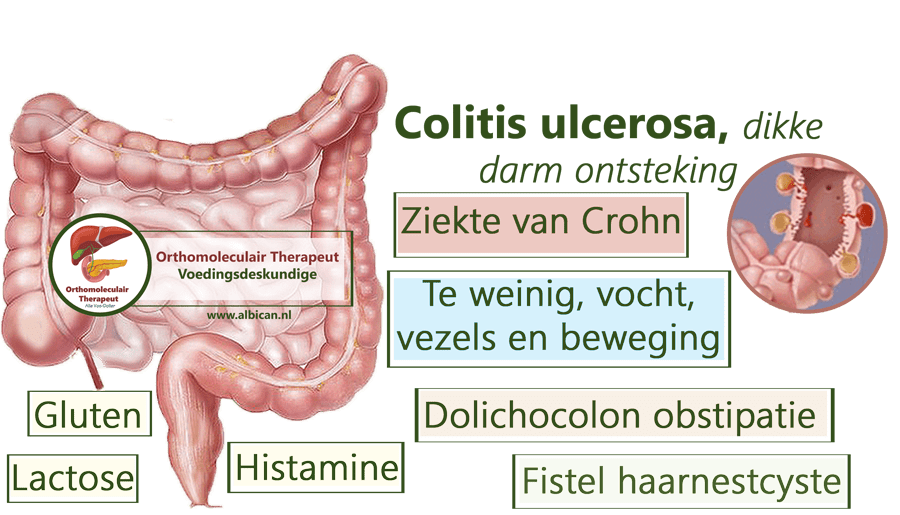
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
You May Like: Best Way To Treat Mouth Ulcers
Ulcerative Colitis: When To Call
anytime you think you may need emergency care. For example, call if:
- Your stools are maroon or very bloody.
- You passed out .
or seek immediate medical care if:
- You are vomiting.
- You have new or worse belly pain.
- You have a fever.
- You cannot pass stools or gas.
- You have new or more blood in your stools.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You have new or worse symptoms.
- You are losing weight.
Managing Severe Active Ulcerative Colitis
Severe active ulcerative colitis should be managed in hospital to minimise the risk of dehydration, malnutrition and potentially fatal complications such as your colon rupturing.
You will be given intravenous fluid to treat dehydration. The condition itself can be treated using injections of steroids or immunosuppressants.
Infliximab
Infliximab is a new type of medication only used to treat severe active ulcerative colitis if you are unable to take steroid medication for medical reasons, such as being allergic to it.
It works by targeting a protein called TNF-alpha, which the immune system uses to stimulate inflammation.
Infliximab is given through a drip in your arm over the course of two hours. This is known as an infusion.
You will be given further infusions after two weeks and again after six weeks. Infusions are then given every eight weeks, if treatment is still required.
Around one-in-four people have an allergic reaction to infliximab and experience symptoms such as:
- joint and muscle pain
- swelling of the hands or lips
- problems swallowing
- headaches
Symptoms range from mild to severe and usually develop in the first two hours after the infusion has finished.
Rarely, people have experienced a delayed allergic reaction days or even weeks after an infusion. If you begin to experience the symptoms listed above after having infliximab, seek immediate medical assistance.
Infliximab is also not recommended for people with a history of heart disease.
Recommended Reading: Where Is Stomach Ulcer Pain
Some Doctors May Use The Following Table To Classify Your Symptoms*:
*A patient does not need to have all of these factors to be considered in a specific category of disease
Ulcerative colitis symptoms are considered moderate when you experience between 4-6 stools per day which include a moderate amount of blood. Severe UC is when you experience 6-10 per day with a severe amount of blood when passing.
If youre concerned about any of your symptoms, talk to your doctor immediately.
How would you describe your symptoms?
Do your best to keep track of your symptoms so you can clearly describe them to your doctor. This information is key in helping your doctor determine the right treatment for you.
because of my UC symptoms, I wasnt able to socialize with my friends. Unfortunately I was missing out on a lot of plans.
Sarah, a real UC patient using HUMIRA
Changing your routine because of UC symptoms? Youre not alone. Hear from others who have been there.
Read Also: How To Heal Mouth Ulcers
You Can Use Telemedicine To Build A Strong Patient
Dont underestimate the importance of a good relationship with your doctor. When patients have good communication with their doctors, theyre especially likely to stick with their treatments and be more satisfied with their care, according to a review published in 2010 in The Ochsner Journal. If the communication between patient and doctor is poor, the patient can feel disheartened and may be less likely to stick with their treatment plan.
Both Battat and Chachu agree that combining in-person visits with telemedicine visits and the use of patient portals usually allows the doctor and patient to communicate with each other more effectively.
Its great to have access to both , as they each provide different options for patients, says Battat.
Don’t Miss: Stelara Dosing For Ulcerative Colitis
You Might Be Able To Communicate With Your Doctor More Often
Doctors are sometimes too busy to jump on a phone call with their patients right away. With telemedicine, people can ask their healthcare providers questions about medications, symptoms, and upcoming visits not to mention go over important lab and test results via patient portals anytime.
I always want patients to know whats going on, says Chachu. When we do routine labs or colonoscopies, for example, I make sure to send those to patients with a little message that says, Your labs are normal, or whatever it may be. … I always want my patients to feel like theyre part of the decision-making process, and telemedicine allows that.
This is a particularly good thing for people with ulcerative colitis. According to a study published in September 2017 in the journal The Lancet, people with IBD who used patient portals to monitor their symptoms had fewer outpatient visits and hospital admissions than those who didnt use telemedicine.
Battat also uses patient portals to share healthcare records and test results with new patients before their appointment. It really helps the doctor know his or her patient much better when theres a back-and-forth, he says.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Recommended Reading: Over The Counter Meds For Ulcers
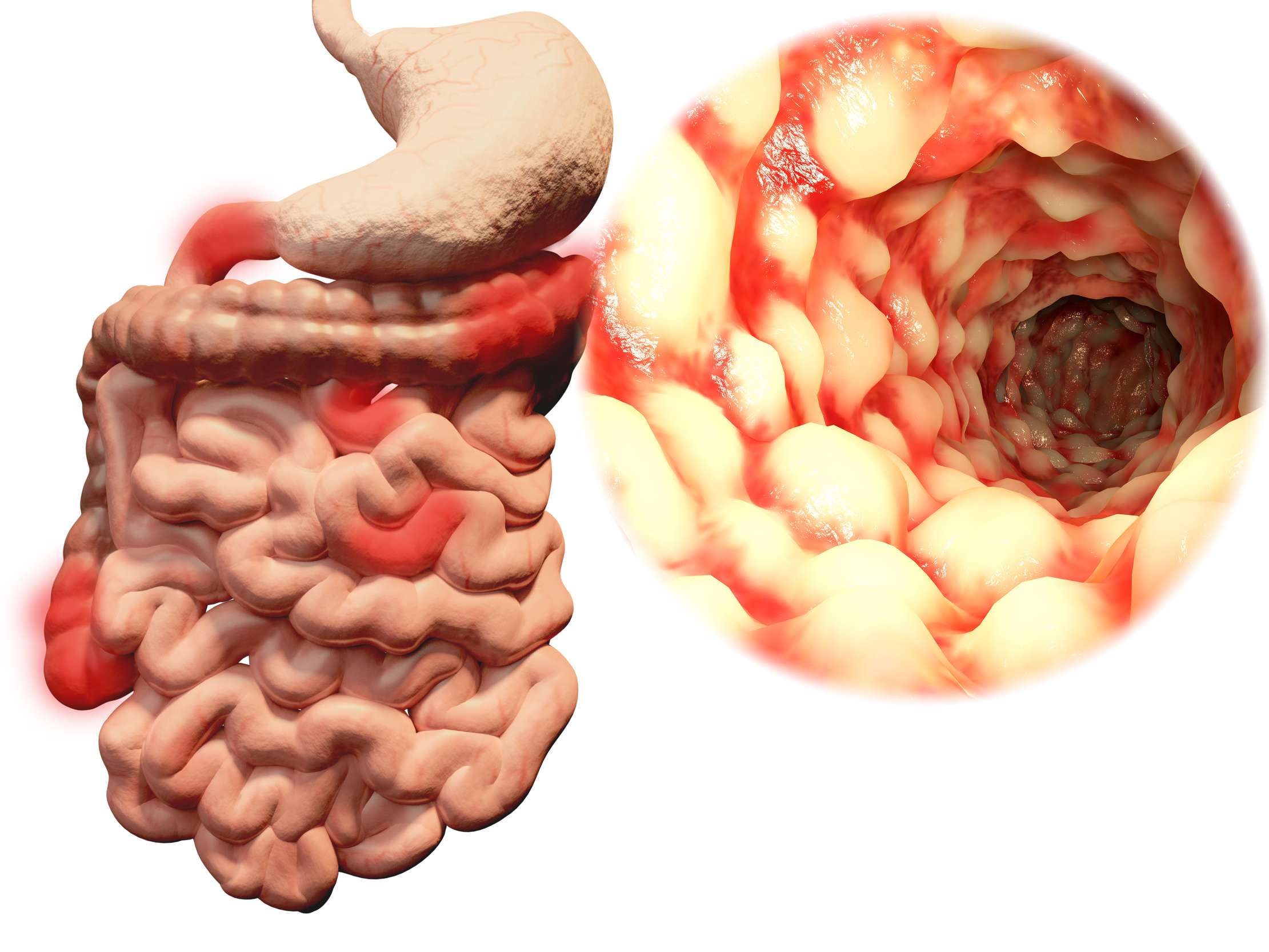
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Also Check: What Foods Can I Eat If I Have An Ulcer
Why Choose Mount Sinai
Mount Sinai has a unique and rich tradition of specialized and individualized treatment and scientific research and discovery in ulcerative colitis. The physicians/scientists in the Mount Sinai Health System are constantly conducting clinical trials and are developing new drug therapies to help patients manage their disease. Learn more about ulcerative colitis.
There are 3 basic tests for colon cancer a stool test , sigmoidoscopy , and colonoscopy . All 3 are effective in catching cancers in the early stages, when treatment is most beneficial.
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
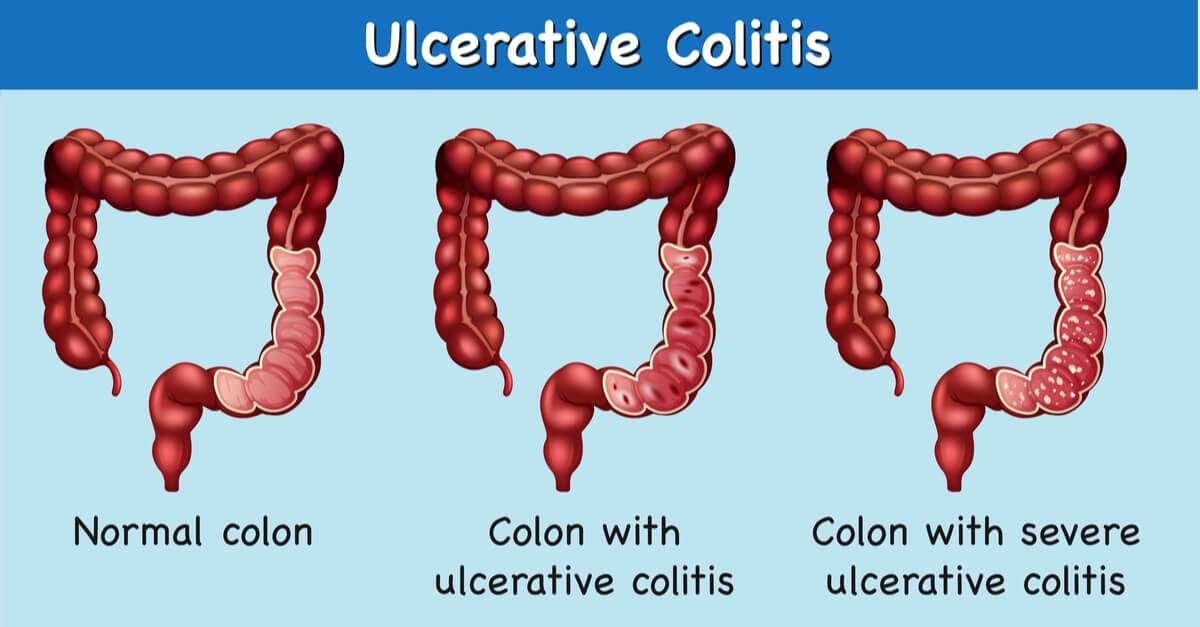
Ulcerative colitis is categorized according to location. Proctitis involves only the rectum. Proctosigmoiditis affects the rectum and sigmoid colon. Left-sided colitis encompasses the entire left side of the large intestine. Pancolitis inflames the entire colon.
You May Like: Is Colitis And Ulcerative Colitis The Same Thing
Treatment Of Ulcerative Colitis
Treatments for ulcerative colitis can control your symptoms and prevent flare-ups. The treatment you have will depend on several things. These include how severe your ulcerative colitis is and how much of your large bowel is affected. Youll be cared for by a team of healthcare professionals with specialist knowledge of inflammatory bowel diseases .
Do Different Types Of Ulcerative Colitis Cause Different Symptoms
Certain symptoms may point to different types of ulcerative colitis. These types, as outlined by the Mayo Clinic, are classified by location within the body:
- Ulcerative proctitis: With this form of the condition, which tends to be the mildest, a person has inflammation in the area closest to the rectum. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis: Inflammation with this form of the disease involves a persons rectum and lower end of the colon. Symptoms can include bloody diarrhea, abdominal pain, and an inability to go despite feeling like you need to let loose.
- Left-sided colitis: This involves inflammation from the rectum, through the lower colon, and into the descending colon. In addition to bloody diarrhea and abdominal pain on the left side, you may also experience weight loss. Most patients will have left-sided disease, Dr. Sinha says.
- Pancolitis: This usually impacts a persons entire colon, causing bloody diarrhea that can be severe, abdominal pain, fatigue, and rapid weight loss.
Also Check: What Is The Best Treatment For Ulcerative Proctitis
How Can I Find Support After An Ulcerative Colitis Diagnosis
When taking care of your physical well-being, dont forget that ulcerative colitis can take a toll on your emotional and mental well-being too. If it turns out your symptoms are ulcerative colitis, you can find a support group, or ask your doctor if they can connect you with a therapist or G.I. psychologist. Dr. Riehl, for example, works with patients on aspects of body image and even connects them with other patients who have experienced colectomy or ostomy . We talk openly about the impact that it can have on them from an intimacy perspective to how it impacts their self-identity, she says.
Since ulcerative colitis often starts at an age when people are thinking about their first job or starting a family, it can be particularly tough. One of the reasons that I and several of my colleagues went into this field is precisely because of thatso that we can hopefully make a difference in peoples lives early, and have them be able to lead productive and complete lives by putting their disease in remission, Dr. Sinha says.
What Uc Symptoms Are Cause For Concern
What’s not normal for UC, again, depends on the person. My abnormal symptoms have included:
-
Severely painful stomach spasms. So painful that I cried out and spent hours wrestling with the cramps to no avail.
-
Lots of blood in my stool. I saw tablespoons of blood with each bowel movement or in place of a bowel movement, only blood.
-
More than three watery bowel movements in a day. If I have more than three and they’re starting to become loose and watery, I know that’s not normal.
In these cases, I seek medical attention.
If you’re experiencing not-so-normal symptoms, I recommend avoid Googling your symptoms and visiting WebMD if a symptom is worth going to a hospital over. You’ll likely only see horror stories or hear about someone’s near-death experience, which isn’t typically indicative of what you’re experiencing.
Recommended Reading: How To Prevent Pressure Ulcers In Wheelchairs
Ways To Reduce The Risk Of An Ulcerative Colitis Emergency
While many patients with ulcerative colitis may experience only mild or occasional symptoms, emergency situations can develop suddenly in both the newly diagnosed and in people who have had ulcerative colitis for a long time.
Keep in mind that the duration of flare-ups can be unpredictable and that remissions can vary in length, which means you always need to be on alert for any new or different symptoms.
The most important control patients have to prevent flare-ups is to continue their maintenance medications, as directed,” says Hanauer. Antibiotics can also trigger flares, so they should only be used when appropriate not for colds or viral infections. Quitting smoking can also trigger flare-ups, so patients should discuss smoking cessation with their gastroenterologists.
Hanauer also recommends that patients with ulcerative colitis eat a healthy diet when theyre in remission to help ensure theyre meeting their nutritional requirements.
As the caregiver, you’re in a unique position to notice changes in the nature and intensity of your loved one’s ulcerative colitis symptoms. Always contact their medical team if you have any questions or suspect that the person with ulcerative colitis is experiencing an emergency. Your prompt action could save a life.
Additional reporting by Jordan M. Davidson.
Incidence Of Respiratory Diseases In Ibd And Of Ibd In Rd
Respiratory diseases are a possible complication of IBD, even if pulmonary alterations are often overlooked, especially when respiratory symptoms are already present before the diagnosis of IBD. The first recognition of a correlation between the diseases of the two districts is attributable to Kraft , who in 1976 reported a series of patients with unexplained bronchial suppuration. Since then, numerous reports have outlined the association between IBD and respiratory pathologies. The rate of extra-intestinal manifestations in patients with IBD ranges from 21 to 41% , increasing with the duration of the intestinal disease, and being greater in CD than in UC . However, the true prevalence of lung involvement in IBD remains unknown and it seems rather variable, because in some series only few cases of respiratory complications have been found. In fact, in 624 patients no respiratory complication was reported, and only 3/1400 cases of IBD were found by Rodgers et al. . On the other hand, it can be difficult to establish a relationship between IBD and RD in patients who are already affected with pulmonary disease at the diagnosis of IBD, or are current smokers.
Table 1 Respiratory Alterations in IBD
in untreated patients was significantly greater than in control subjects
Alterations affecting the lung parenchyma are relatively rare in IBD patients, and cryptogenic organizing pneumonia is the most common reported manifestation .
You May Like: Best Foods To Eat When You Have A Stomach Ulcer