Green Banana & Applesauce
Both green bananas and cooked and cooled apples are high in soluble fibers and resistant starches which help to slow down transit and soak up excess moisture which can be helpful if diarrhea is a concern. According to theUniversity of Wisconsin Health, applesauce is helpful for ulcerative colitis and are a rich source of vitamins and minerals like potassium.
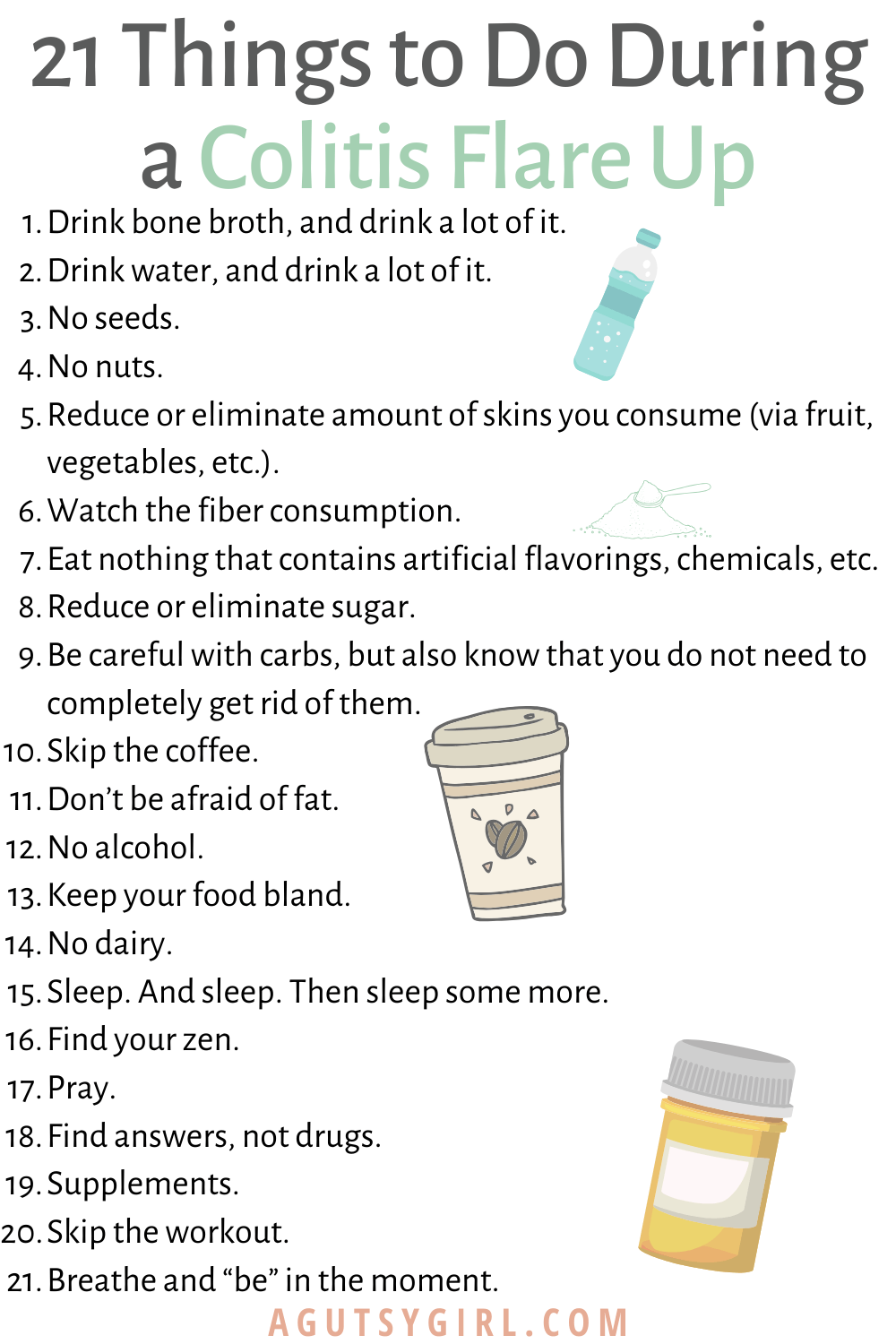
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Ulcerative Colitis Crohns Disease Or Something Else
The colon, also known as the large intestine, has three parts or section: ascending colon , transverse , descending colon , and the sigmoid colon just before the rectum.
Ulcerative colitis symptoms in each person will be different depending on where inflammation occurs and how bad it is. The most common symptoms include:
There are common complications that tend to come with UC, even though they are not actually a direct result of this chronic health condition. Fever, fatigue, and anemia are perhaps the most common additional symptoms. Additionally, inflammation beyond the colon often shows up as skin sores, skin rashes, mouth sores, joint pain, red and painful eyes, and sometimes even liver disease.
While both are referred to as inflammatory bowel disease or IBD, and Ulcerative colitis is related to Crohns disease, they are still different. Crohns disease, unlike ulcerative colitis, is not limited to the colon and is a chronic inflammatory disease of the intestines or the entire GI tract. Crohns often affects the small intestine and colon although occasionally it, too, is limited to the colon.
Also Check: Venous Stasis Ulcer Right Lower Leg Icd 10
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
What To Eat During Remission
Increase fiber and reintroduce whole grains — Slowly incorporate foods higher in fiber when gastrointestinal symptoms lessen.
Consume omega-3 fatty acids — Consider eating more fresh or canned fatty fish or taking a fish or flaxseed oil supplement.
Focus on wholesome foods in their natural state — This includes foods with minimal processing and minimum ingredients.
Dairy and lactose products will be better tolerated — If you have a lactose intolerance, avoid dairy or eat low-lactose or lactose-free products.
Added fats will be better tolerated — Continue to focus on using oils, such as olive oil or canola oil, instead of solid fats.
Continue to focus on protein foods — Consume beef, eggs, poultry and other lean meats or plant-based proteins, such as soy products.
Be sure to drink plenty of water — Drink water instead of fruit juices, soft drinks, alcohol and caffeinated beverages such as coffee or tea.
Don’t Miss: How Do You Diagnose A Stomach Ulcer
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
- Apple sauce
- Herbal or green tea.
Can You Eat White Bread With Ulcerative Colitis
Low-residue diet
Temporarily eating a low-residue or low-fibre diet can sometimes help improve symptoms of ulcerative colitis during a flare-up. These diets are designed to reduce the amount and frequency of the stools you pass. Examples of foods that can be eaten as part of a low-residue diet include: white bread.
Recommended Reading: Nutritionist Specializing In Ulcerative Colitis
You May Like: What Foods Should Be Avoided With Stomach Ulcers
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Challenges In Creating Evidence
Although there are diet intervention trials that show promise in maintaining remission, their efficacy remains in question. The short duration of the interventions , the lack of a proper control group in some instances, and the small sample sizes make it very challenging for clinicians to draw firm conclusions from existing data. There is an overall lack of objective clinical and endoscopic disease markers. For example, many studies are completed retrospectively and they rely on patient questionnaires regarding disease symptoms, such as pain and stool frequency. Well-designed clinical trials in IBD are urgently required to define the precise role of each of these diets in the prevention or management of IBD. Up until now, the role of diet in IBD is highly undermined by lay and anecdotal reports without sufficient scientific proof.
High quality diet intervention studies for the treatment of IBD need to include the following: quantification of baseline intake of the habitual diet monitoring of diet adherence through food recalls large prospective, control trials over a longer-term use of a control diet to determine the specificity of observed effects to the intervention use of a variety of endpoints to monitor response to diet interventions and consider the use of IBD animal models to discover the mechanisms of pathogenesis.
You May Like: Stomach Ulcer Foods To Eat
What To Eat On An Ulcerative Colitis Diet During A Flare:
Eating during an Ulcerative Colitis flare needs to be approached with caution. When you are in pain, feeling bloated, and just dont feel like eating, choose foods that are easy to digest.
-
Select refined grains. Refined grains are easier to digest than whole grains. So, select white bread, white rice, and white pasta. Yes, a dietitian is recommending you eat white grains! These foods are sources of B vitamins and Iron.
-
Choose low fiber vegetables and fruits. Low-fiber vegetables are well cooked or canned veggies, mashed potatoes without the skins, and string beans. Cooking veggies helps to break down the fiber. So, when you are flaring, avoid salads and other dishes with raw vegetables. Also, remove the skin from raw veggies and fruits and avoid produce that has seeds such as strawberries and raspberries. Low-fiber fruits are bananas or cantaloupes. For a nutrient-rich drink, reach for low-sodium vegetable juice.
-
Use unsaturated fats. Cook with small amounts of heart-healthy unsaturated oils. Try different oils to replace butter or stick margarine. Aim for a fat intake below 35% of your daily calorie intake. A low-fat diet may help to prevent bloating, cramping, and diarrhea.
-
Reach for calcium-rich foods. For example, low-fat dairy products , canned salmon, and soy products. Oat, soy, or rice drinks enriched with calcium are another option.
How To Identify Your Trigger Foods
Theres no way around this one: Youve got to track everything you eat and what, if any, symptoms result. Even if you work with an R.D. , this will be an important part of that process. For example, maybe you realize that every time you eat dairy, diarrhea follows a few hours later. Or maybe a night of drinking really sparked a flare-up. Watch for patterns like this and make note. And dont forget to take your food diary with you to your doctors appointmentsit can be a useful tool to help you and your health care team figure out how best to manage your UC. You can go the old-fashioned route and use a paper format or try an app like GI Monitor.
When youre planning your meals, forget about sticking to three squares. Eating large portions can overwhelm your already-sensitive digestive system. Instead, aim for smaller portions spread throughout the day instead of a few big meals. Downing your food too fast can also lead to discomfort, so eat slowly and mindfully and really concentrate on chewing your food thoroughlythat gives your gut a little extra help!
Read Also: How Do You Get Rid Of Leg Ulcers
What To Eat On An Ulcerative Colitis Diet And What To Avoid Eating
Andrea Jeffery, MS, RDN, LD , On January 4, 2022
Ulcerative Colitis Disease is a chronic inflammation of the digestive tract. The large intestine and the rectum are affected in Colitis. Inflammation affects the innermost lining of the colon. Colitis is found in large, continuous sections. The inflammation causes abdominal pain, cramping, and diarrhea. Living with this pain and GI distress can cause fatigue. You may lose weight or struggle to maintain a healthy weight.
How does your life work when your stomach is tied up in knots? If you have Ulcerative Colitis Disease, you may feel your life has been interrupted. How do you get back into the game? What can you eat on an Ulcerative Colitis Diet?
The cause of Ulcerative Colitis Disease is unknown. If someone in your family has Ulcerative Colitis, you may be more at risk. Researchers are studying the role of genes and the bodys immune systems. There are also studies on environmental factors such as smoking. Depression, sleep disturbance and stress are factors that may also increase the risk of Ulcerative Colitis Disease. Ulcerative Colitis is a type of Inflammatory Bowel Disease .
How Can I Live With Chronic Ulcerative Colitis
If you are struggling with colitis or another type of irritable bowel disease, help is available at Gastroenterology Associates of Southwest Florida, PA. Our team provides compassionate, expert care to help patients suffering from these types of chronic conditions. Find out how we can help you live with chronic ulcerative colitis
You May Like: Cbd Oil For Stomach Ulcers
Seek Out A Professional
Creating a diet plan isn’t easy, which is why it’s always a good idea to get professional help. Meeting, even just once, with a dietitian, can be a revelation in terms of diet and answering that question “what do I eat?” Our understanding of IBD and diet is always evolving, so fine-tuning a flare-up diet plan is an ongoing process, and checking in with a dietitian will be helpful.
Many people with IBD restrict foods when in a flare-up, but more calories are needed to prevent losing too much weight. A physician can help you understand weight loss and how much is too much.
What If Youve Had Surgery For Uc
If youve had surgery for UC, such as an ileostomy , your GI may give you specific guidelines regarding your diet and nutrition. For example, they may recommend you eat extra foods with vitamin B12 or take a supplement since removal of the ileum can make it hard for you to absorb the B12 you need. A lack of this vitamin can affect the health of your nerve and blood cells.
It’s also extra important to stay hydrated if youve had surgery for UC, so make sure youre drinking lots of water and eating foods with a high-water content. Talk with your health care team and registered dietitian to understand how your surgery may affect your dietary needs.
Read Also: Whey Protein And Ulcerative Colitis
Can Surgery Affect Nutritional Status
Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohn’s disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
Also Check: Aloe Juice For Ulcerative Colitis
Who Gets Ulcerative Colitis And Why
UC like all other health conditions is caused by various underlying factors including unresolved infections, toxins, nutritional deficiencies and emotional patterns.
Ulcerative colitis is an inflammatory bowel disease that occurs mostly in developed nations, and is more common in urban centers where the Western diet pattern dominates. It is estimated that approximately 1 million people in the U.S. alone suffering from the disease and its many gastrointestinal symptoms.
As a chronic illness, UC can be active at times and inactive at other times. If the symptoms are mild, they do not make the body burn out. The unpredictable nature of ulcerative colitis makes diagnosis very challenging.
The disease may start at any age, but individuals with the disease usually develop it between 15 and 25.
It seems that there is a genetic component to ulcerative colitis because individuals of eastern European Jewish lineage have a great risk of ulcerative colitis. While the cause is still unknown, research has hinted at a connection to irregular reactions to bacteria in the colon. Evidence does not indicate that ones diet is the cause of ulcerative colitis.
To diagnose ulcerative colitis a colonoscopy is usually ordered, during which an endoscope is passed through the anus and into the colon. While ulcerative colitis can be diagnosed by X-rays of a barium-filled colon, colonoscopy should be used because they are more sensitive and allow for biopsies to be taken of the lining of the colon.
What About A Low Fodmap Or Other Diets
FODMAP stands for fermentable oligosaccharides, di-saccharides, mono-saccharides, and polyols. They are the carbohydrates found in foods and they draw water into the colon, which can make you feel bloated and uncomfortable. FODMAPs also dont pass through your gut quickly but can ferment and hang around for a time, which can cause colitis symptoms.
FODMAPs include:
- Any foods with lactose, or dairy ingredients
- Foods with fructose, including natural fruits, honey, or processed high-fructose corn syrup
- Fructans like garlic, onions, or wheat
- Galactans, which are beans, lentils, or soybeans
- Polyols such as fruits with seeds like apples, avocados, cherries, figs, and peaches
There are other types of diets such as a specific carbohydrate diet that cuts starchy potatoes and grains. Some people have found relief on a Mediterranean diet that includes vegetables, whole grains, fruits, fish, and poultry. A gluten-free diet could also lessen your symptoms.
Recommended Reading: Herbal Medicine For Stomach Ulcer