How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Abdominal Pain And Stomach Cramps
It is normal to have abdominal pain from time-to-time, caused by gas, stomach bugs, or even food poisoning. However, if you or a loved one is experiencing abdominal pain that you would describe as intense, crampy, and the pain doesnt go away in a day or two, or has been present on and off for weeks or longer, its time to see a healthcare provider to find out whats wrong.
You May Like: Best Diet For Ulcer Patients
When Should You Call Your Doctor
If youre experiencing certain symptoms, chances are, your current treatment is not working and its time to consider a change in therapy, says Ha. Call your doctor if:
- Cramping is severe
- Youre experiencing a significant amount of abdominal pain that requires medication
- You have a fever that lasts longer than a couple of days
- You experience nausea or vomiting
- You have ongoing diarrhea or blood in your stool
Educate Yourself And Talk To Your Doctor
Learning more about your condition can help you feel more confident about what is happening inside your body and determining ways to manage your symptoms.
You also should look into whether you have other medical conditions that may be contributing to your IBD symptoms. Talk with your health care provider about your symptoms. You can discuss ways of treating or managing them together.
You May Like: What Foods To Avoid With Peptic Ulcer
Can You Fart In Your Sleep
People commonly fart in their sleep, although they usually are not aware of it. Research suggests pressure in the fluctuates in cycles throughout the day. This muscle is more relaxed during sleep, and it controls whether or not gas present in the large intestine is released. This muscle also spontaneously relaxes multiple times per hour in the morning. As a result, passing gas overnight or in the morning is common.
If you want to fart less during the night, it helps to understand what gas is, why humans pass gas, and what factors lead to excessive gas. By making lifestyle changes or addressing underlying health issues, you may be able to reduce your nighttime or morning flatulence.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
You May Like: Lion’s Mane Ulcerative Colitis
Adopt Better Sleep Habits
A regular bedtime routine promotes better Zzzs for everyone, but it may be especially helpful for those with UC. Thats because a nightly ritual signals your body that its time to calm down and relax, Javelli explains. Try to hit the hay at approximately the same time each night. In addition, avoid blue-lit screens within one to two hours of sleep, and keep your bedroom quiet, cool, and dark. A bedroom temperature between 60° and 67°F is optimal for sleep, according to the National Sleep Foundation.
You May Like: List Of Foods To Eat When You Have An Ulcer
Poor Sleep Patterns Could Increase Your Chance Of Developing Ulcerative Colitis
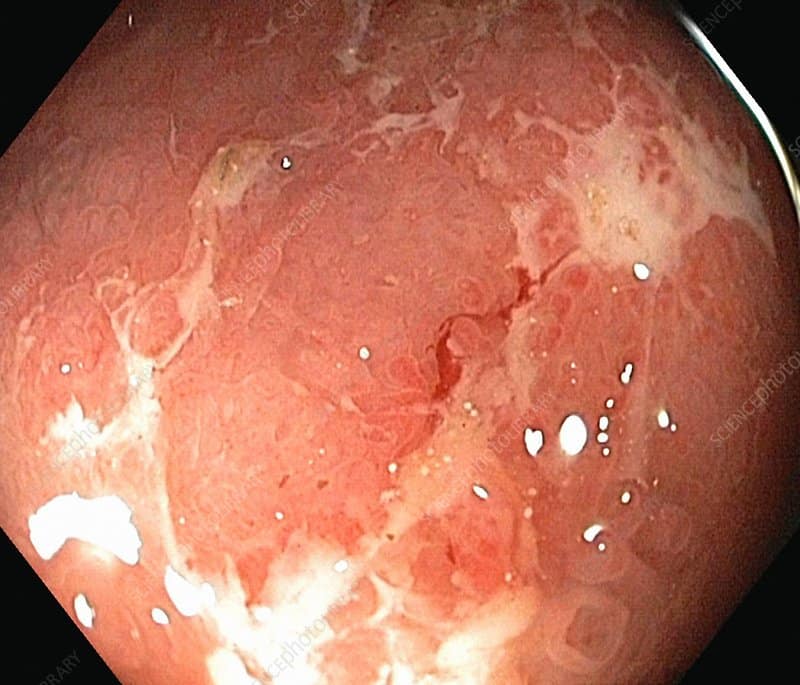
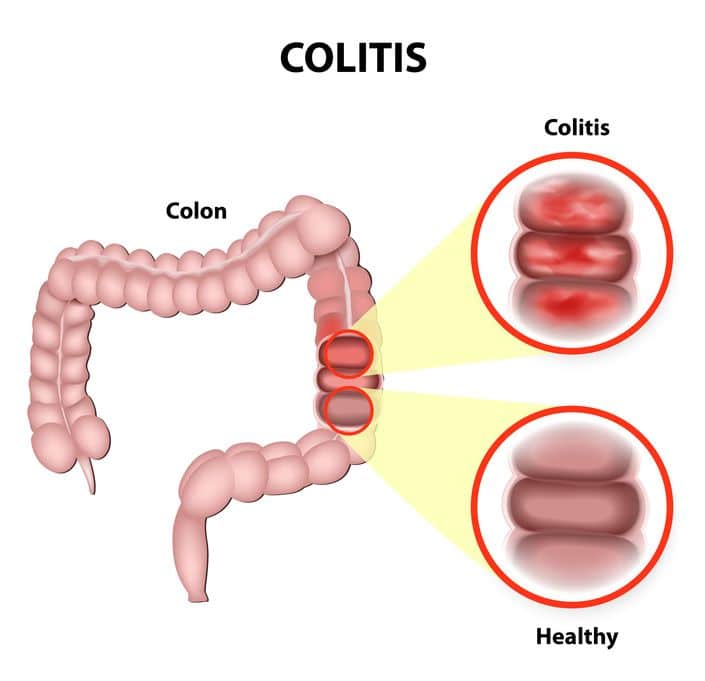
While it remains mostly a mystery why we need sleep, what we do know is that it is a crucial part of maintaining good health. Not getting the right amount of sleep can leave you feeling tired and groggy, it can affect your mood and appetite, make your concentration dwindle, and even exacerbate certain illnesses. On top of all this, new research shows that not getting enough sleep, or sleeping too much, can increase your chance of developing ulcerative colitis , a chronic inflammatory bowel disease , consisting of fine ulcerations in the inner mucosal lining of the large intestine. UC can be a devastating disease, with sufferers experiencing diarrhea, rectal bleeding, and abdominal cramping.
A well-known study, following more than 150,000 female nurses for more than 30 years, found that the women who slept on average 6 hours a night or fewer were slightly more likely to develop UC than those who slept for 7-8 hours each night.1 Even more alarmingly, was that those who slept for more than 9 hours each night were more than twice as likely to develop UC as those who slept the ideal amount.
If you are concerned about the effects that a lack of sleep could be having on you, then consult your physician.
First published in the Inside Tract® newsletter issue 192 2014
1. Ananthakrishnan AN. et al. Sleep Duration Affects Risk for Ulcerative Colitis: A Prospective Cohort Study. Clinical Gastroenterology and Hepatology. 2014 12:1879-86.
Image: Free-Photos from Pixabay.com
Don’t Miss: Nurses Role In Pressure Ulcer Prevention
Eat Earlier In The Day
The time you eat your meals can play a big role in how often you need to use the bathroom in the middle of the night, says Dr. Yen. Often, people have to go to the bathroom right after they eat. If you typically eat late, try moving up your dinner time, he advises. If possible, make lunch your largest meal, adds Diane Javelli, R.D., a clinical dietician at the Nutrition Clinic at UW Medical CenterMontlake in Seattle. Not possible? Eat dinner early in the evening and try to consume lighter, more easily digestible foods that are lower in fat and fiber.
Consider Your Sleep Position
Sometimes the way you sleep can worsen symptoms. For example, sleeping on the side where your bowel is most inflamed can cause some people to have diarrhea, Dr. Yen says. Some patients will realize this and figure out they can only sleep on their stomach, or on their back, or on their left side, Dr. Yen says. As with other sleep strategies for UC, it may take some trial and error to discover the right sleep position for you.
Also Check: Is Ulcerative Colitis A Serious Disease
Is Honey Good For Ulcerative Colitis
Is honey good for ulcerative colitis? Manuka honey has been proven to improve antioxidant status and reduce inflammation in rats with both IBS and ulcerative colitis, a type of inflammatory bowel disease . It has also been shown to attack strains of Clostridium difficile.
Can I have honey with ulcerative colitis? Honey may have some features in the treatment of colitis, but this issue requires further investigation. Honey, prednisolone and even disulfiram also have some value in preventing the formation of free radicals released from the inflamed tissues.
Is honey good for colon inflammation? According to a few scientific articles, Manuka honey may reduce inflammation in your digestive system, which could reduce symptoms of IBS . However, honey contains a lot of fructose. Fructose is a FODMAP, and can trigger IBS symptoms.
What foods heal ulcerative colitis? Can certain foods make ulcerative colitis worse? Diet will affect your symptoms, but its not going to affect the underlying disease. Its like putting lemon juice on a cut. Youll hurt more, but the lemon juice wont make the cut worse.
Recommended Reading: How Is Ulcerative Colitis Caused
A Healthy Digestive System
Intestinal gas is a normal part of digestion. While people may not like it when they do it, especially at inappropriate times, its just a sign of a regular, healthy digestive system at work, says Dr. Kyle Staller, a gastroenterologist with Harvard-affiliated Massachusetts General Hospital.
Gas is produced when bacteria in the digestive system break down food. Intestinal gas contains mostly hydrogen and methane, with small amounts of other gases like hydrogen sulfide, which give gas a bad odor. Yet most components of intestinal gas are odor-free.
But can you ever be too gassy and is frequent gas ever a problem?
Which foods you eat and how you digest them can increase gas production. For instance, as people age, they often have trouble digesting foods that contain short-chain carbohydrates called FODMAPs, a term that stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
These foods are either not digested or incompletely digested, which causes increased fermentation by gut bacteria and ultimately creates more gas, says Dr. Staller.
You May Like: How Do You Get Ulcerative Colitis
Fever Is A Common Symptom Of Inflammation
When inflammation occurs in your colon, it triggers your bodys immune response by raising the temperature. This temperature change can lead to fever and night sweats, which may need additional treatment or even a hospital stay to bring back under control.
The good news is that colitis can be treated to reduce and remove symptoms. While there is no cure for ulcerative colitis or inflammatory bowel disease, there are ways of managing the condition that can prevent these symptoms from becoming an issue for you.
When you visit us at Hawaii Gastroenterology Specialists, well guide you through the various treatment options that are available, depending on which will suit your needs best. This may be medication, immune-suppressing drugs, and diet and lifestyle changes.
If you believe you may have colitis, come and see us, the Hawaii Gastroenterology Specialists , by booking your appointment online today.
Be Aware That Steroids May Cause Sleep Problems
Corticosteroids, which act as anti-inflammatories, are commonly used to manage flares, according to the Crohns and Colitis Foundation. But according to the National Sleep Foundation, corticosteroids, which are stimulants, can interfere with sleep. Sleep disturbances are common in patients who are on steroids, says Hanauer.
Fortunately, these medications are typically used as short-term treatments, and once your disease is controlled and you stop taking steroids, your sleep issues should improve, says Hanauer.
Don’t Miss: Can Probiotics Make Ulcerative Colitis Worse
Articles On Ulcerative Colitis Overview
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
Symptoms Can Range Widely In Severity And Frequency Between People
Ulcerative colitis causes inflammation and ulcers along the lining of your intestines. This condition can be uncomfortable, but with effective treatments you can manage your symptoms with ease and focus o. Ulcerative colitis is a health condition that affects your digestive tract, and thats one of the main reasons why its important to watch your diet. Ulcerative colitis from the inside out written by elizabeth pratt a person living with ulcerative colitis is three times more likely to develop sacroiliitis written by jenna fletcher written by charlotte lillis 3 studies cited written by j. Wondering how much your medical care wil. Medication is one of many options to help treat ulcerative colit. The best treatment for ulcerative colitis depends on the severity of the condition. Ulcerative colitis is a form of inflammatory bowel disease. Many of its early symptoms resemble those of other conditions, which is why its important to learn more about what dist. Ulcerative colitis is a chronic condition that develops in your intestines over time and has symptoms that come and go. The colon carries waste to be expelled from the body. Can physical or cognitive activity prevent dementia? Overview of ulcerative colitis, an inflammatory bowel disease does your child need to bathe every day?
Read Also: Crohn’s And Ulcerative Colitis Diet
Sleep Struggles And Crohns Disease
Jan 23, 2019 | Crohns Disease, IBD
If you already suffer from Crohns disease, youre likely already experiencing some uncomfortable symptoms that can be hard to manage, such as abdominal pain and fatigue. However, beyond general malaise, researchers have recently discovered a link between moderate sleep disturbances and Crohns disease, especially if you have a persistent case of Crohns. Read on to learn more about Crohns disease and its symptoms, the result of this recent study, and how to manage your symptoms to improve your quality of life.
Read Also: Does Stelara Work For Ulcerative Colitis
Crohns Disease And Ulcerative Colitis
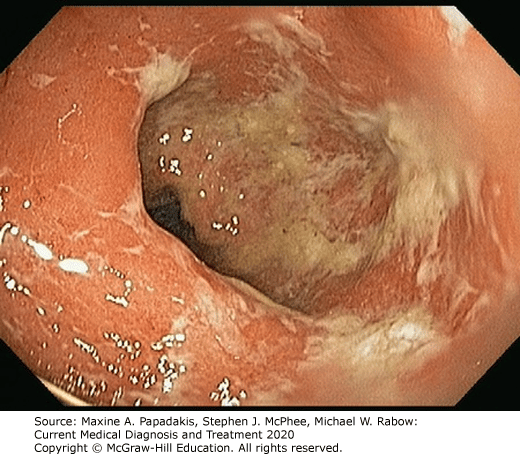
A serious but rare complication of these forms of inflammatory bowel disease is fulminant or toxic colitis, formerly called toxic megacolon.
The signs and symptoms of this condition can include bloody diarrhea along with fever, racing heartbeat , low blood pressure , metabolic acidosis , low urine output , and acute kidney failure.
Toxic colitis is more common with ulcerative colitis than it is with Crohns disease.
Read Also: Foods To Avoid With Peptic Ulcer
Recommended Reading: Wound Care Treatment For Diabetic Foot Ulcer
What Do I Feel And What Do I See
Rectal bleeding is usually the first and often the only sign you will see. Intermittent abdominal crampy discomfort is common. So is diarrhea, especially at night. When you have had the disorder for awhile, fatigue, weakness and even fever can occur.
Most importantly, these symptoms wax and wane. Even so and especially if rectal bleeding has occurred, medical attention should always be sought immediately.
Talk To Others Who Understand
On MyCrohnsAndColitisTeam, the social network for people with Crohns disease and ulcerative colitis and their loved ones, more than 155,000 members come together to ask questions, give advice, and share their stories with others who understand life with inflammatory bowel disease.
Is your IBD worse in the mornings? Share your experience in the comments below, or start a conversation by posting on MyCrohnsAndColitisTeam.
Don’t Miss: Ulcerative Colitis Abdominal Pain Relief
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I cant bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I cant fully stand upright sometimes for a minute or so. Its frustrating.
Sulphur And Hydrogen Sulfide
Some health experts believe that this bloating has to do with excess sulfur in the intestinal tract. Sulfur is found in many foods, like dairy products, soy milk, eggs, and others. When inside the digestive tract, sulfur ferments and converts to hydrogen sulfide. Too much hydrogen sulfide is known to cause stomach pain and diarrhea.
Research indicates that people with ulcerative colitis may produce more hydrogen sulfide than others. People with ulcerative colitis may also have more difficulty breaking down that gas, which means that it spends more time in the colon and can further damage the intestinal lining. If the gas builds up too quickly or cannot be broken down, it may produce the bloating symptoms that people with ulcerative colitis experience.
Its unknown if hydrogen sulfide buildup is entirely responsible for bloating in people with ulcerative colitis. However, it is one mechanism that may cause or make the problem worse. Eating a lot of fatty foods or being constipated may make bloating worse, too.
Note that bloating may also be caused by something other than ulcerative colitis. If you suddenly start experiencing bloating, talk to your gastrointestinal doctor. They can determine whether ulcerative colitis is the culprit or recommend testing to rule out other potential causes.
You May Like: How To Soothe An Ulcer