Favorite Orgs For Essential Uc Info
CCF is the leading nonprofit organization dedicated to finding the cure for UC and Crohns. The organization is at the forefront of IBD research and works to educate, empower, and support individuals afflicted with these diseases. Find your local chapter by visiting the CCF website.
This research institute at Virginia Mason in Seattle is one of the few establishments devoted to finding the causes of autoimmune diseases like UC and their cures. Benaroya has already helped advance research in more than 80 diseases of the immune system. The autoimmune life blog provides information on community events and personal stories from patients living with an autoimmune disease.
Dont Miss: What Does Ulcerative Colitis Affect
The 5 Goals Of Colonoscopy In Ulcerative Colitis
Stephen Hanauer, MD
This transcript has been edited for clarity.
Hello. I’m Dr Stephen Hanauer from Northwestern University in Chicago, speaking to you today about the role of colonoscopy in the management of ulcerative colitis.
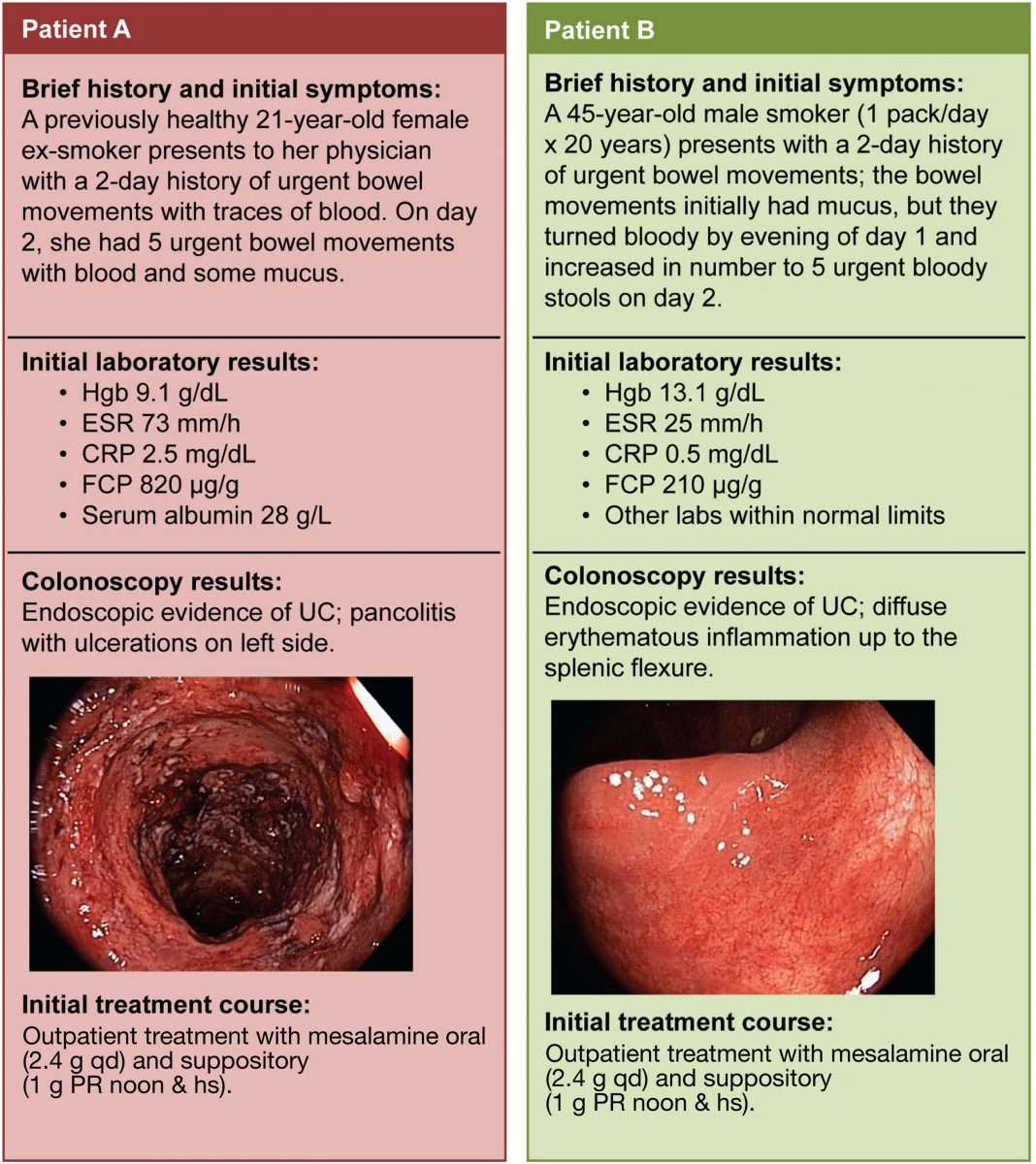
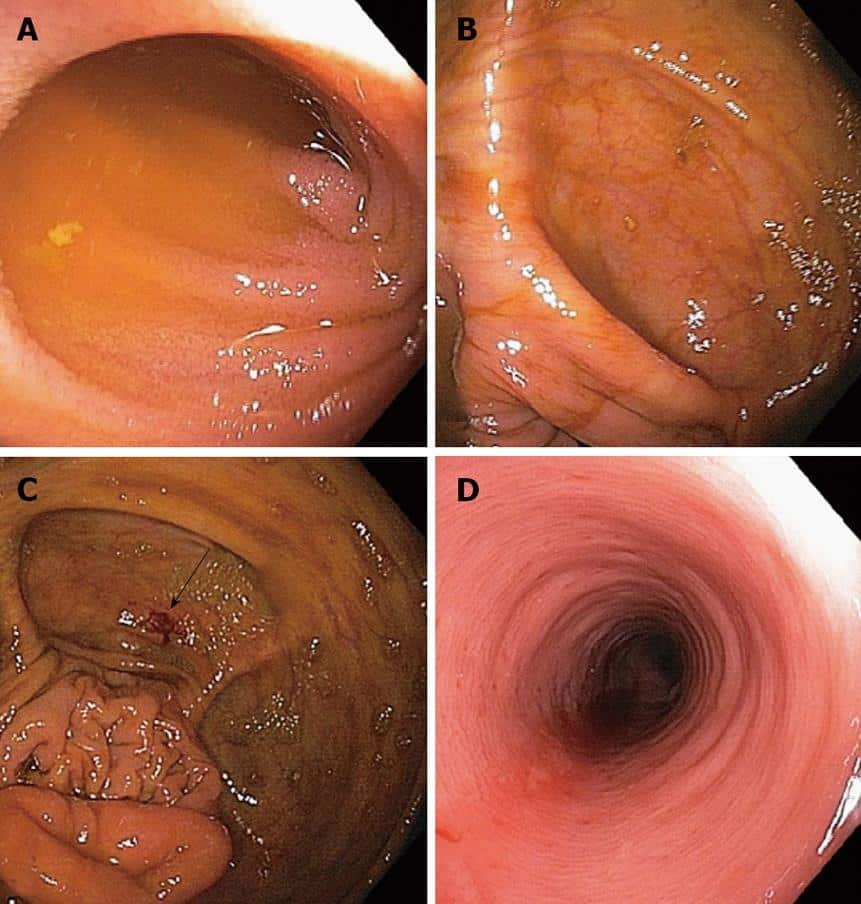
There are several indications for performing colonoscopy in patients with ulcerative colitis: confirming the diagnosis and separating ulcerative colitis from other inflammatory disorders assessing the extent and severity of disease to determine the treatment intensity therapeutic monitoring and treating to endoscopic targets to demonstrate endoscopic healing and finally, for cancer surveillance.
Confirming the Diagnosis
The diagnosis of ulcerative colitis is based on a combination of clinical, endoscopic, and histopathologic findings .
There are actually very few clinical manifestations of ulcerative colitis that could be noted on a physical examination. The exceptions are those patients with very severe disease, abdominal tenderness, or who appear anemic.
Laboratory studies are also nonspecific but should be performed to determine the blood count and to rule out infections.
Endoscopy, or colonoscopy, is the hallmark for the diagnosis of ulcerative colitis and separating it from other inflammatory disorders of the colon. This is due to the fact that performing colonoscopy provides the ability to take biopsies and the histologic confirmation of ulcerative colitis.
Figure 1. Clinical, endoscopic, and histopathologic findings.
Risk Stratification
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Recommended Reading: How Often To Reposition To Prevent Pressure Ulcers
Diarrhea And Rectal Bleeding
People with ulcerative colitis often experience watery diarrhea as well as frequent and sudden urges to have a bowel movement. For some people, the urge to have a bowel movement may occur so suddenly that it significantly disrupts their daily life. Some people need to have a bowel movement more than 10 times per day.
You may notice blood, pus, or mucus in your stools. You may also experience rectal bleeding if youre having a flare-up. Blood comes from ulcers along the surface of your rectum.
If you have uncontrollable diarrhea or notice blood in your stool, you should see a doctor. Diarrhea caused by ulcerative colitis can lead to medical emergencies like severe dehydration, a perforated colon, or .
Signs And Symptoms Of Ulcerative Colitis
Classified as an inflammatory bowel disease , ulcerative colitis is a disease that primarily affects the digestive tract, but usually also has an impact on other parts of the body. It can cause symptoms of bloody diarrhea, abdominal pain, and an urgent need to empty the bowels. Symptoms can cycle through periods of remission and active disease.
Symptoms may differ from person to person, which can make diagnosis and treatment challenging, but there are a few that hint at having the condition.
Don’t Miss: Signs Of An Ulcer In A Woman
Do I Need To Be Screened For Colon Cancer
Yes. Everyone needs to be screened for colon cancer beginning at 50 years old. But if you have IBD, your risk of colon cancer is higher. You might need to be screened at a younger age or more often than people without IBD.
- Talk to your doctor about when to begin colon cancer screening, what tests to get, and how often to have them.
- Your doctors suggestions will depend on your family health history, how long you have had IBD, whether your colon is affected by your IBD, and how severe it is.
- If you have had IBD for 8 to 10 years, your doctor may recommend a colonoscopy with biopsies every 1 to 2 years. This test checks for early warning signs of cancer.
Also Check: How Do You Check For A Stomach Ulcer
Don’t Delay Seeking Help
We know its not always easy talking about your bowel habits, but the sooner you get diagnosed, the easier your condition will be to treat.
Some important things to remember:
I always knew something wasnt right. Its not normal to bleed or feel like that. Initially, I felt scared and didnt want to tell anyone but being diagnosed helped me come to terms with it and get on with life.
ArizonaLiving with Indeterminate Colitis
You May Like: What Causes A Bleeding Ulcer In Stomach
The Day Of Your Colonoscopy
The big day is here: You have endured the prep and are ready to get your colonoscopy over with. In addition to details about what you can eat or drink on the day of your colonoscopy, your doctor should also let you know what medications you can and cannot take. Blood thinners such as warfarin and certain other medications should typically not be taken before your procedure. Make sure your doctor knows all of the medications and supplements you are taking so you can discuss ahead of time what you can and cannot take the day of your procedure.
What Are The Causes And Risk Factors Of Ulcerative Colitis
Ulcerative colitis is believed to be caused by an abnormal response by your bodys immune system.
Your immune system is supposed to defend you against harmful invasive bacteria and viruses. But in some people, the immune system mistakenly attacks the bodys own tissue.
While we dont know exactly what causes ulcerative colitis, there are two leading theories:
Experts believe that ulcerative colitis develops because of a combination of environmental factors and genetic predisposition.
Fatty cold-water fish such as mackerel, tuna, salmon, sardines, and herring are rich sources of omega-3 fatty acids.
Editor’s Picks
Read Also: How Do Stomach Ulcers Heal
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
While There Is No Cure For Ulcerative Colitis There Are Many Options To Help Treat It
The goals of treatment are to:
- Control inflammation, or swelling.
- Ease symptoms, like pain, diarrhea and bleeding.
- Fix nutrition deficiencies, if needed.
Treatment will depend on the severity of the disease, past complications and response to earlier treatments. Remember, everyone experiences symptoms of ulcerative colitis differently. If one treatment doesnt work as well, there are other options. Just be sure to be in touch with your gastroenterologist often.
Treatment options for ulcerative colitis involve medications, surgery or a combination.
Medications
The goals of using medications are to start or keep up remission and to improve quality of life. Each person reacts a little bit differently to each drug and many need a combination of drugs. While some of them have side effects, the benefits and symptom relief often outweigh those drawbacks. Learn more about each class of drug in theLiving with IBDpages.
Biosimilars have been approved by the U.S. Food and Drug Administration to use as treatment in place of existing biologic drugs.
They are based on an existing biologic but are not an exact copy.
Biosimilars work the same way as their originator biologics and are given the same way.Read more about biologics and biosimilars.
Your doctor can prescribe a biosimilar as a substitute for a biologic drug however, your pharmacist cannot change you from a biologic drug to a biosimilar without your doctors approval.
Other medications
Also Check: How Do You Treat Skin Ulcers
What Are The Causes Of Colon Cancer Vs Ulcerative Colitis
Colon Cancer Causes
Most colorectal cancers arise from adenomatous polyps. Such polyps are comprised of excess numbers of both normal and abnormal appearing cells in the glands covering the inner wall of the colon. Over time, these abnormal growths enlarge and ultimately degenerate to become adenocarcinomas.
People with certain genetic abnormalities develop what are known as familial adenomatous polyposis syndromes. Such people have a greater-than-normal risk of colorectal cancer. In these conditions, numerous adenomatous polyps develop in the colon, ultimately leading to colon cancer. There are specific genetic abnormalities found in the two main forms of familial adenomatous polyposis.
Adenomatous polyposis syndromes tend to run in families, which are referred to as familial adenomatous polyposis . Celecoxib has been FDA approved for familial adenomatous polyposis. After six months, celecoxib reduced the mean number of rectal and colon polyps by 28% compared to placebo 5%.
Other risk factors for developing colon cancer include:
- Ulcerative colitis or Crohn’s disease
- Breast, uterine, or ovarian cancer now or in the past
- A family history of colon cancer
- Colon cancer usually occurs before age 40 years.
Ulcerative Colitis Causes
Emotional stress or food sensitivities do not cause ulcerative colitis however, these factors may trigger symptoms in some people.
Risk factors for inflammatory bowel disease include:
When To See A Healthcare Provider
If you have any symptom that is troubling you, you should speak to a healthcare provider.
In particular, you should see a healthcare provider if you have symptoms like:
- Abdominal pain that does not improve
- Blood in the stools
- Diarrhea that does not go away
- Vomiting that does not go away
- Distended abdomen
Persistent abdominal pain is not normal, and bleeding from the rectum is not normal. If you have any doubts about your health, you should speak with your healthcare provider.
You May Like: What Is Infusion Therapy For Ulcerative Colitis
Favorite Ulcerative Colitis Blogger
Sam Cleasby created her blog in 2013 to raise awareness of IBD and her struggles with self-esteem. Cleasby also has a radio show on BBC Radio Sheffield in which she shares about modern family life, including relationships, disability, nutrition, and kids. You can subscribe to her blog via email or follow her on or .
Treatment Of Ulcerative Colitis
Treatment of ulcerative colitis generally involves trying to promote intestinal healing, suppress symptoms and avoid flare-ups. Medication is available for these purposes, including simple over-the-counter medicines for people who are only experiencing mild symptoms.
Treatment of ulcerative colitis generally involves trying to promote intestinal healing, suppress symptoms and avoid flare-ups. Medication is available for these purposes, including simple over-the-counter medicines for people who are only experiencing mild symptoms.
Some patients will require more aggressive medication management, and will need to discuss the risks and benefits of these medications with their gastroenterologist before starting any treatment. Patients who have already been diagnosed should keep track of what they eat and how their bodies react to certain foods, so that they know what foods to avoid. This can vary widely as well, depending on the case. While some patients find that foods with a high fiber content help ease the digestion process, fibrous foods might trigger bouts of diarrhea in another patient.
Overall, inflammatory bowel diseases such as ulcerative colitis can be an embarrassing and burdensome condition to deal withfeel free to ask a colonoscopy question to one of our medical experts if you need advice on how to live with IBD or if you feel you need to be diagnosed.
“*” indicates required fields
Read Also: Best Cure For Leg Ulcers
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
Rectal preparations are particularly good at treating urgency and bleeding, symptoms that often are very bothersome. A positive response often occurs within days of treatment.
What Does Ulcerative Colitis Look Like
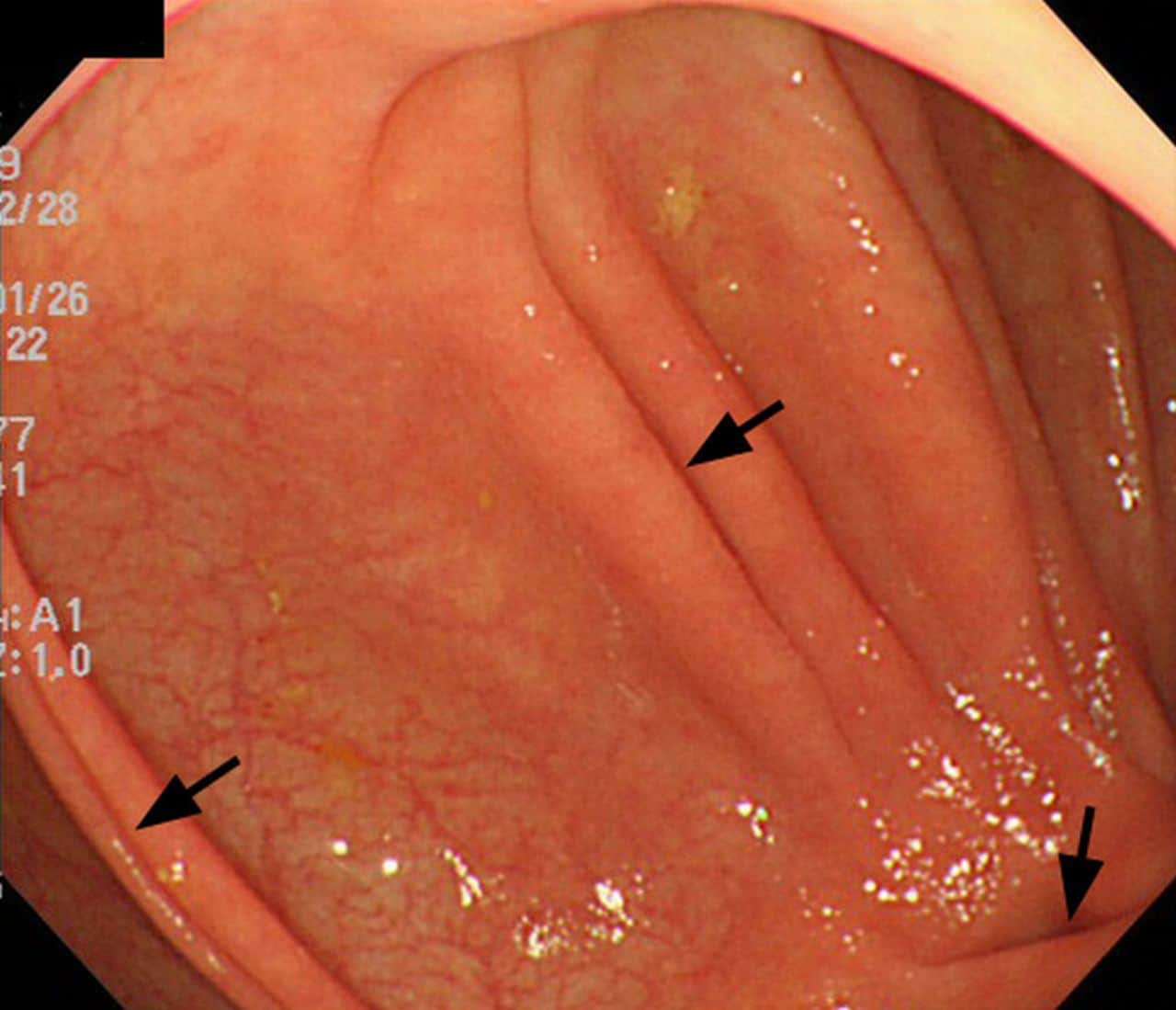
With UC there is a wide variation in the amount of inflammation from person to person, so that in mild cases the bowel can look almost normal but, when the inflammation is bad, the bowel can look very red and ulcerated. Ulcerative colitis usually affects the rectum, but occasionally there is no inflammation . Sometimes the inflammation is limited just to the rectum . However, the inflammation can involve varying lengths of the colon. When the whole large bowel is affected, this is called pan-colitis .
Also Check: How To Avoid Pressure Ulcers
Types Of Ulcerative Colitis
The different types of ulcerative colitis and symptoms are based on the location of inflammation within the colon or rectum. The types of ulcerative colitis include:
- Ulcerative proctitis: This is the mildest form of ulcerative colitis. Inflammation is in the rectal area and causes rectal pain and bleeding and an urgent feeling to move your bowels.
- Proctosigmoiditis: With this type, inflammation is in the rectum and lower area of the colon, causing stomach pain and cramping, bloody diarrhea and trouble moving your bowels despite the urge to go.
- Left-sided colitis: The inflammation of this type extends from the rectum through the sigmoid and descending colon in the upper-left abdomen. This type causes stomach pain and cramping on the left side, bloody diarrhea and weight loss.
- Pancolitis: This type causes inflammation of the entire colon that causes stomach pain and cramping, bloody diarrhea, significant weight loss and fatigue.
- Fulminant colitis: This is the rarest and most severe form of ulcerative colitis. It can cause extreme diarrhea, dehydration and shock, and it can be life-threatening.
Ulcerative Colitis And Covid
The coronavirus pandemic has forced everyone to take extra precautions when it comes to health and safety. This is especially true for individuals with a compromised immune system. Although research shows that people living with UC are no more susceptible to catching the virus than the general population, organizations including the American College of Gastroenterology and the Crohns and Colitis Foundation have issued guidelines to help limit the spread of the infection. Its also recommended that people with ulcerative colitis get a COVID-19 vaccine.
A number of resources are available to help people with UC manage these difficult times from medication assistance to virtual therapy for mental health.
You May Like: Foods To Eat With Bleeding Ulcer
Medications For Ulcerative Colitis
Medications can calm the inflammation inside your colon. The first one youâll usually try is from a group called aminosalicylates. If that doesn’t help, your doctor might prescribe a steroid like prednisone. A third option is an immune modifier, which lowers inflammation by changing the activity of your immune system. It can take up to 3 months before you feel the benefits.
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with Crohns disease and ulcerative colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 159,000 members come together to ask questions, give advice, and share their stories with others who understand life with Crohns disease and ulcerative colitis.
Have you had a colonoscopy for ulcerative colitis? Share your experience in the comments below, or start a conversation by posting on MyCrohnsAndColitisTeam.
You May Like: Are All Ulcers Caused By H Pylori
What Is Colon Cancer
Cancer is the transformation of normal cells. These transformed cells grow and multiply abnormally. Cancers are dangerous because of their uncontrolled growth and potential for spread. Cancer overwhelms healthy cells, tissues, and organs by taking their oxygen, nutrients, and space.
In colon cancer, these abnormal cells grow and eventually spread through the colon wall to involve the adjacent lymph nodes and organs. Ultimately, they spread to distant organs such as the liver, lungs, brain, and bones.
Most colon cancers are adenocarcinoma tumors that develop from the glands lining the colon’s inner wall. These cancers, or malignant tumors, sometimes are referred to as colorectal cancer, reflecting the fact that the rectum, the end portion of the colon, also can be affected. Anatomic differences in the rectum as compared to the rest of the colon require that doctors separately recognize these areas.