Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
Can Bedsores Be Prevented
Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas. Other methods of preventing bedsores and preventing existing sores from getting worse include:
- Turning and repositioning every 2 hours
- Sitting upright and straight in a wheelchair, changing position every 15 minutes
- Providing soft padding in wheelchairs and beds to reduce pressure
- Providing good skin care by keeping the skin clean and dry
- Providing good nutrition because without enough calories, vitamins, minerals, fluids, and protein, bed sores cant heal, no matter how well you care for the sore
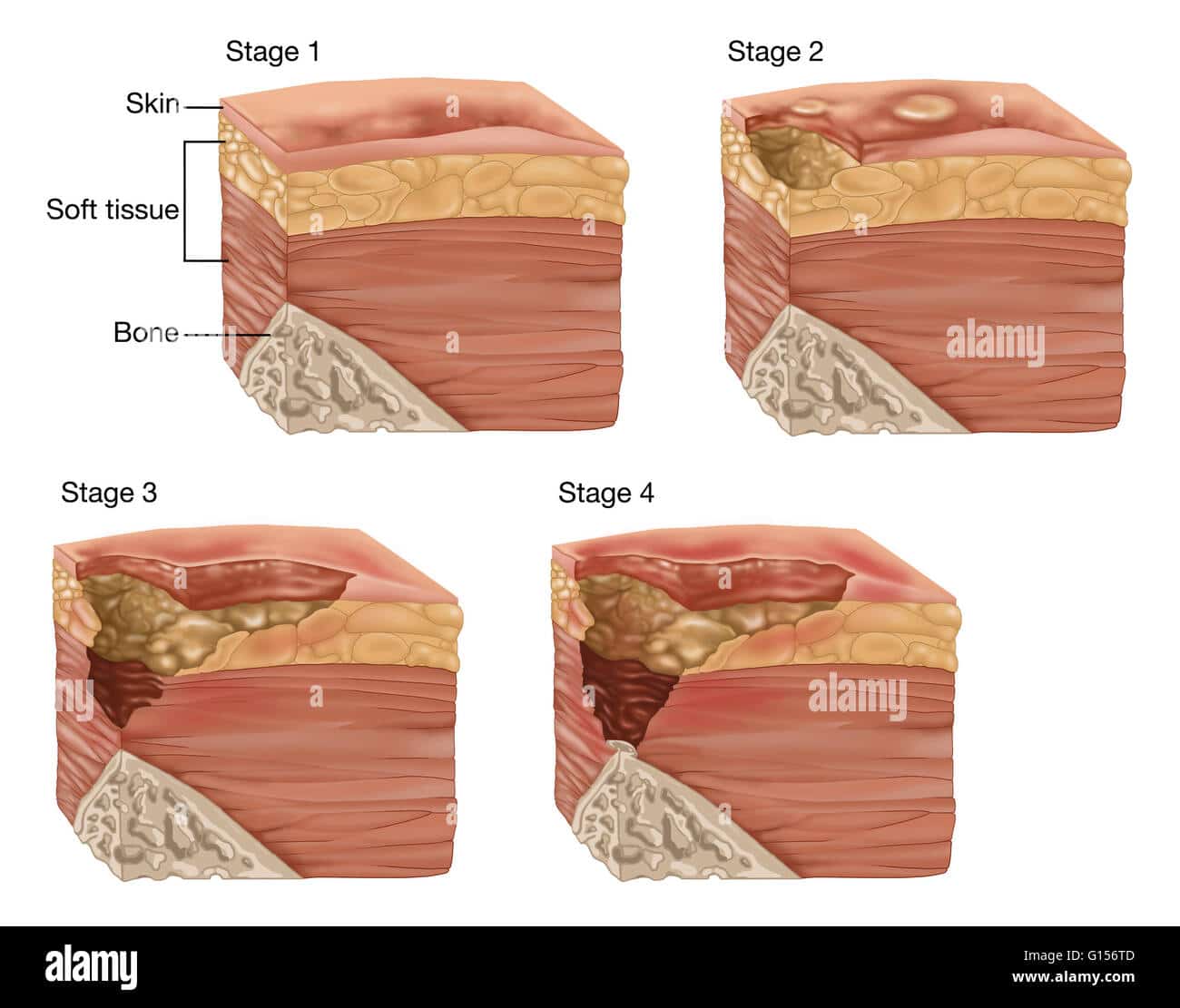
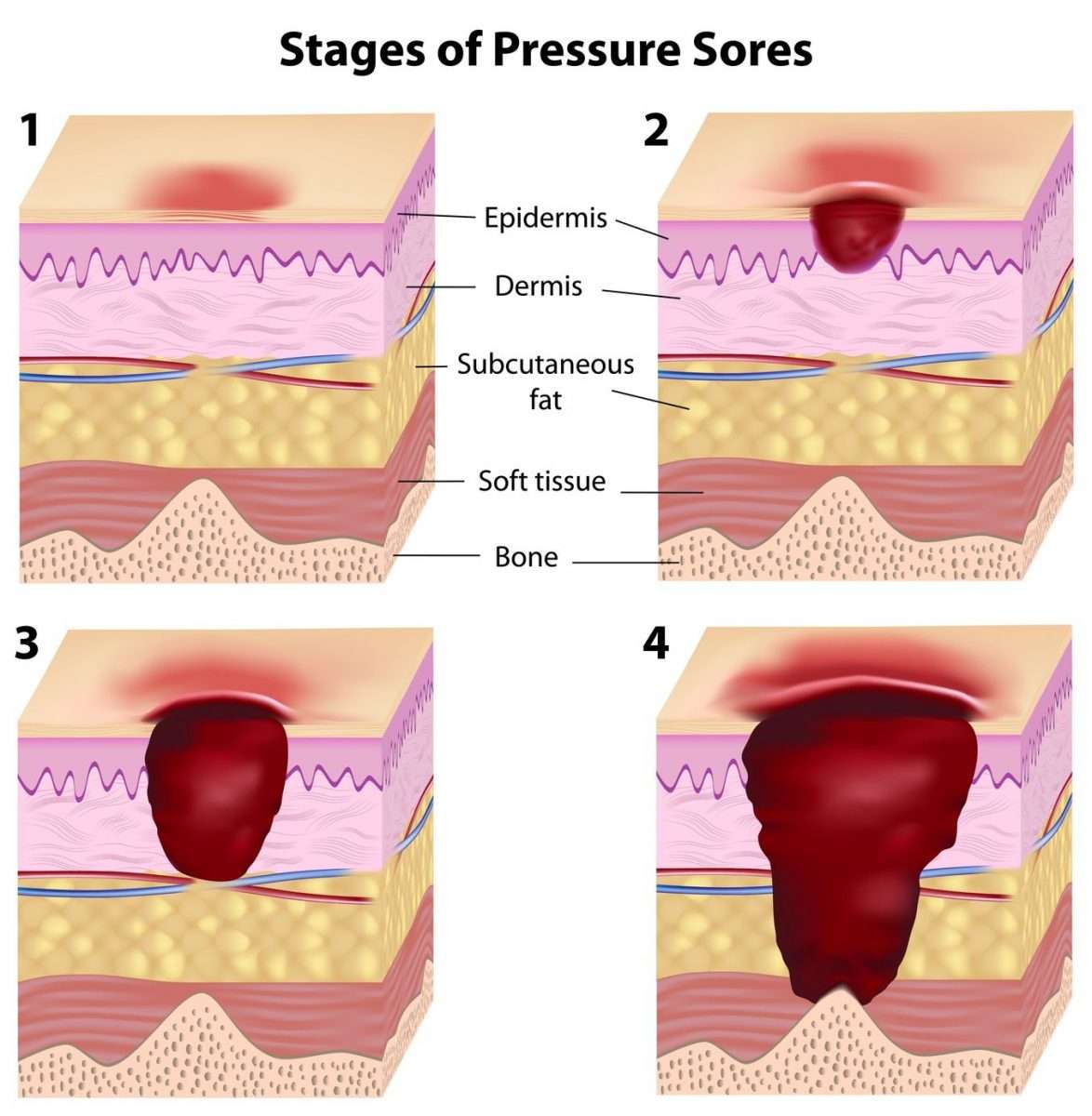
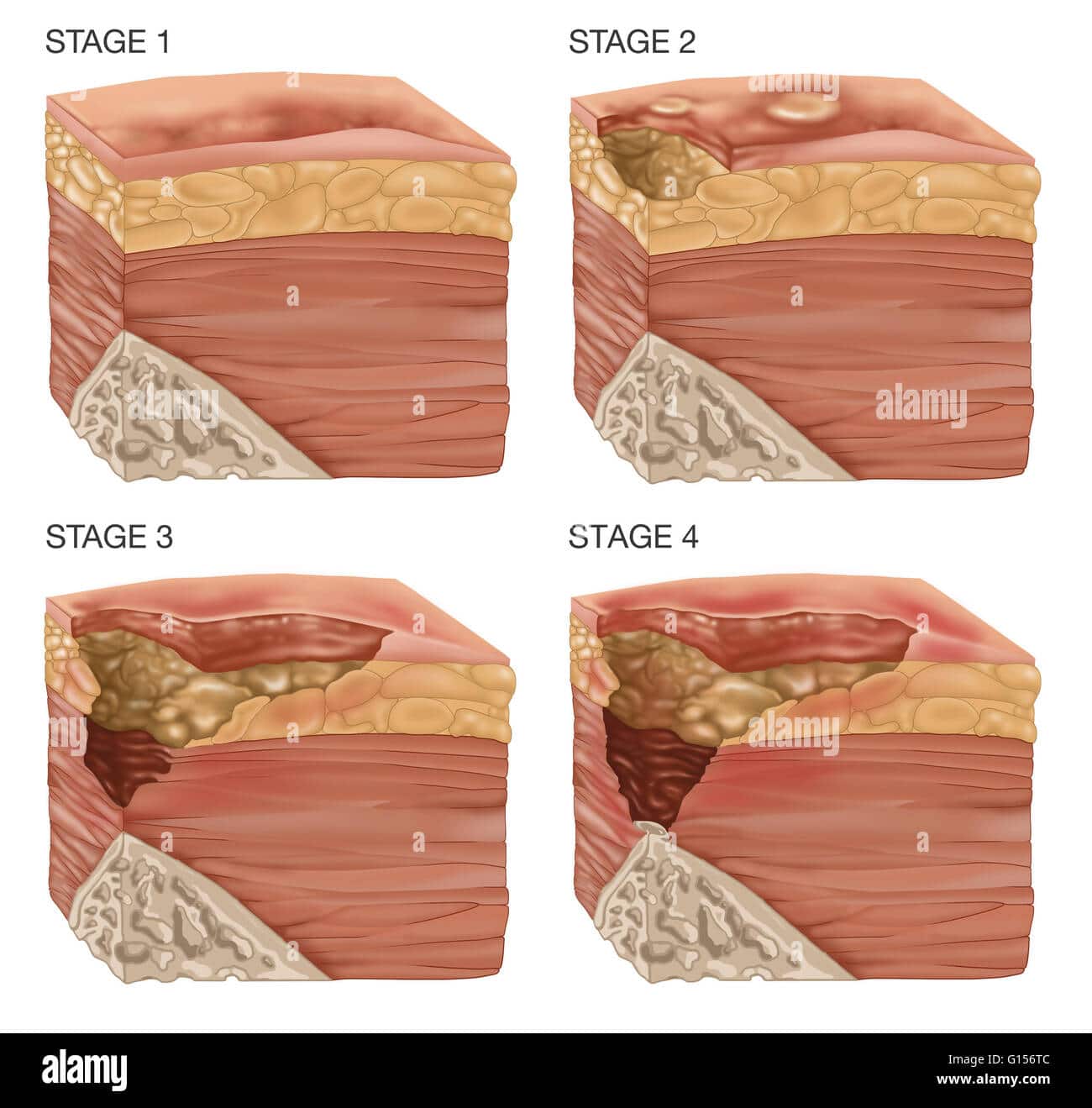
Severity Of Pressure Ulcers
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
Don’t Miss: How To Get Rid Of Stomach Ulcer Pain
Pressure Ulcer Of Sacral Region Stage 4
- 2016201720182019202020212022Billable/Specific Code
- L89.154 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.154 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.154 â other international versions of ICD-10 L89.154 may differ.
- Healing pressure ulcer of sacral region, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, sacral region
- Applicable To annotations, or
The Icd Code L89 Is Used To Code Pressure Ulcer
Pressure ulcers, also known as pressure sores, bedsores and decubitus ulcers, are localized injuries to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. The most common sites are the skin overlying the sacrum, coccyx, heels or the hips, but other sites such as the elbows, knees, ankles or the back of the cranium can be affected.
| Specialty: |
Also Check: How Do I Tell If I Have An Ulcer
Hygiene And Wound Dressings
Practice good hygiene. For stage I ulcers, wash the area with water and mild soap, rinse well and pat the area dry gently and carefully. Do not rub forcefully on the area directly over the wound. Usually Stage I decubitus ulcers will not need to be covered.
For Stage II and III ulcers, use saline solution to clean the wound and dry it carefully. Apply either gauze dampened with saline, a hydrocolloid dressing , or a thin foam dressing such as Allevyn. The latter two dressings can be left on until they loosen or wrinkle for up to five days. If gauze is being used, the dressing should be changed twice each day and should stay damp between the times the dressing is changed. Always check to see if the ulcer is healing every time you change the dressing.
The best treatment for decubitus ulcers that are stage IV is to consult a physician for instructions. Many times these types of wounds require surgery and dressings for this kind of ulcer should be applied by a professional. A surgery called debridement is utilized to remove all dead tissue so that the wound will not become infected. Some minor debridement can be done at the bedside but larger areas need to be done in the operating room. The physician will medicate the patient because this is usually a painful procedure.
How Do I Get Rid Of An Ulcer On My Butt
Caring for a Pressure Sore
Recommended Reading: Are Fermented Foods Good For Ulcerative Colitis
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Who Is Most Likely To Die From Bedsores
Although bedsores can kill persons of all ages and backgrounds, there are certain populations that are more susceptible.
- Advanced Age.People 64 years or older are more likely to suffer from bedsores and death.
- Nursing Home Residents. Recent studies show that over one quarter of all instances of pressure ulcers occur in nursing homes. In fact, in 2004, 11% of all nursing home residents in the country had bedsores. Most nursing home residents have multiple risk factors, including immobility, sensory deficiency, and incontinence.
- Circulatory Problems. Bedsores are more likely to occur when blood flow is already impaired due to a chronic illness associated with circulation.As such, persons with a diagnosis of stroke, hypotension, diabetes of any type, coronary artery disease, and hypoxia are at heightened risk.
- Pulmonary and Renal Problems. Bedsores tend to develop more often when blood cannot be oxygenated, or when red blood cells are prevented from being generated by the body. Therefore, persons with pulmonary disease, end stage renal failure, or severe anemia are at increased risk.
- Malnutrition. Nutrition plays a large part in healing wounds. When a resident has chronic conditions that impair nutrition intake, the likelihood of death increases. Persons with dysphagia, diarrhea, and cancer may be at increased risk of death from bedsores.
Donât Miss: How To Treat Rodent Ulcers In Cats At Home
Read Also: Does Turmeric Help With Ulcerative Colitis
The Stages Of Decubitus Ulcer
There are several stages of decubitus ulcer. The first is called Stage One. At this stage, fatty tissue surrounding the pressure sore may become exposed. At stage three, the pressure sore may be larger and may even affect surrounding tendons and joints. In stage four, the skin tissue surrounding the pressure sore may be seriously damaged. The patient may even contract a blood or bone infection.
Selecting The Right Dressing For Sacral Ulcer Management
A tremendous number of dressings are available for different types of wounds, and variousguidelines are available to help wound care professionals determine which type of dressing should be used in various circumstances. For example, petrolatum-impregnated dressings are nonadherent dressings that are useful in wounds with minimal exudate. Conversely, alginates and hydrofiber are moderately or highly absorbent, respectively, which makes them useful in wounds with excessive exudate production.
Don’t Miss: Ozanimod Phase 2 Ulcerative Colitis
Pressure Injury Stages: When To Seek Medical Help
Pressure ulcers can occur in anyone who sits for prolonged periods or is confined to bed rest. The best way to prevent pressure wounds is to alternate how you sit or lay in bed. While you can treat stage 1 and stage 2 ulcers at home, if you do not see any change in your symptoms within two to three days, you should see your doctor.
The longer bed sores go untreated, the more likely they will advance into later stages and cause significant tissue, muscle, tendon, and bone damage.
A personal injury lawyer can help you create a case if youre dealing with injuries due to neglect or abuse. The team at Jack Bernstein, Injury Attorneys have extensive experience in dealing with personal injury claims due to accidents, neglect, medical malpractice, and more. Contact us today for a free consultation.
Which Doctors Treat Bed Sores
Bed Sores Doctors in India
- 95% Dr. Shaila Welling. General Surgeon. …
- 91% Dr. Jugal B Agrawal. Laparoscopic Surgeon. …
- 91% Dr. Ramesh Dumbre. General Surgeon. …
- 91% Dr. Jamshed D Sunavala. Critical Care Specialist. …
- 91% Dr. MG Bhat. General Surgeon. …
- 97% Dr. V Jinadas. …
- 91% Dr. Tallam Prem Kumar.
Read Also: Crohn’s Disease And Ulcerative Colitis
Stage 4 Bedsore Therapy
Stage 4 bedsore treatment is more accurately described as stage 4 bedsore management for most elderly patients. Although stage 4 bedsore treatment can be aimed at actually healing the open wound, many elder patients are not healthy enough to fully recover from a stage 4 bedsore. As a result, there are many medical processes in place that focus entirely on minimizing pain and discomfort for an elderly person with stage 4 bedsores.
Stage 4 bedsore management may involve the following:
Berman, Kevin. Pressure Ulcer.Medline Plus. Atlanta: 2012. < > .
Bluestein, Daniel and Ashkan Javaheri. Pressure Ulcers: Prevention, Evaluation, and Management.American Academy of Family Physicians. 2008. < > .
FREE Case Evaluation
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a if a nursing home patient dies from an untreated bedsore.
Also Check: What Do You Do If You Have An Ulcer
Recommended Reading: Extra Virgin Olive Oil And Ulcerative Colitis
Stage 3 Pressure Ulcer
A stage 3 ulcer expands into the lower layers of the skin and fat tissues. The skin around the wound will start to turn black as it dies. The center of the wound will begin to form a crater. Other symptoms you may notice are:
- Foul-smelling pus
The wound can also feel warmer to the touch than the surrounding skin. Additionally, there may be very little pain at this stage because the tissue around the wound is dying.
Treatment for a stage 3 wound requires seeing your healthcare provider. The dead skin tissues have to be removed. You also may require an antibiotic to eliminate the infections. With proper medical care, the wound will heal but can take as long as four months.
How Does Bad Nursing Home Care Cause Bedsores
Every nursing home is required by Federal and state law to take precautions aimed at reducing bedsore occurrences. In fact, the Centers for Medicare and Medicaid Services may cite a nursing home for failing to take the proper precautions. So what are those requirements?
- Comprehensive Assessment. Every resident admitted to a nursing home must be assessed from head to toe for skin impairments. Also, the facility must calculate the residents risk level for developing bedsores.
- Care Plan. Once the assessment is conducted, the data acquired is used to create an action plan. Called a care plan, this document details the ways in which the nursing home should prevent bedsores. For example, a proper turning/repositioning regime or an increase in protein intake at meal time.
- Update Care Plan. Assessment does not stop after the care plan is created. If problems arise afterwards, then the nursing home is obligated to update the care plan with new ideas and interventions.
Bad care means that the nursing home fails to complete one of the three steps above. Essentially, the resident that comes into the nursing home with no bedsores should leave the nursing home with no bedsores.
Also Check: What Medicines Are Used To Treat Ulcerative Colitis
What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
Read Also: Ulcerative Pancolitis With Rectal Bleeding
What Qualifies As An Open Wound
Unlike closed wounds, such as bruises or closed fractures, open wounds are injuries that involve a break in the skin and leave the internal tissue exposed. The skin has an important role in protecting the organs, tissues, and other structures inside the body, so a breach of the skin can potentially invite infection.
Read Also: What To Eat To Help Stomach Ulcers
What Are The Stages Of A Bedsore Or Decubitus Ulcer
,are one of the most common forms of nursing home neglect. They are often caused when a patient is not turned on a regular basis resulting in pressure on the bony prominences of the body. The pressure reduces the blood flow to the area causing the surrounding tissue to die. Decubitus ulcers are usually located on the lower back near the tail bone, upper back near the shoulder blade area, buttocks, heels, knees, elbows, and sometimes ankles.
There are four generally accepted stages of bedsores however, a fifth stage is sometimes used to explain exceptionally deep decubitus ulcers. The descriptions are as follows:
Stage I A Stage I decubitus ulcers usually appears as a red spot on the skin that fails to disappear once the pressure from the area is relieved. It may appear as a small rash. Stage I decubitus ulcers can usually be eliminated with proper treatment and turning by the healthcare provider.
Stage II A Stage II decubitus ulcer may appear as a small blister or slightly broken skin. A Stage II should be carefully monitored by the healthcare staff. The staff may provide additional conditioning of the skin and may request an air mattress to alleviate the pressure on the affected area. Stage II decubitus ulcers are sometimes unavoidable depending on the patients condition and co-morbidities.
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debrideand dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
- Use positioning devices to prevent prolonged pressure bony prominences.
- Keep the head of the bed as low as possible to reduce risk of shearing.
- Keep sheets dry and wrinkle free.
Also Check: Crohn’s Versus Ulcerative Colitis Pathology
Prevention Of A Decubitus Ulcer
At risk individuals should be checked for signs of the development of a decubitus ulcer every day. Caregivers need to examine the person’s body from head to toe, paying particular attention to bony areas where decubitus ulcers tend to develop. They should look for areas of skin that don’t turn white when pressed. Other preventative measures include:
- Changing the person’s position every two hours
- Using supporting items like pillows or foam pads reduce pressure over pressure points
- Keeping skin clean and dry and applying moisturizing lotions made especially for fragile skin
- Providing the person will well-balanced, nutritious meals and 8-10 glasses of water daily
- Helping the person do daily range-of-motion exercising
- Cleaning carefully after urination or bowel movement and applying cream formulated for fragile skin if necessary