Nursing Home Neglect And Stage 3 Bedsores
When a lack of care causes a resident to develop a stage 3 bedsore, nursing home neglect may have occurred.
Neglect is not the same thing as making a simple, harmless mistake its a life-threatening error or series of errors. Sadly, poorly trained or inattentive staff can provide consistently poor care to residents, which can lead to bedsores.
Nursing home neglect often goes hand-in-hand with another issue: understaffing in long-term care facilities. When there are less staff members available, residents may have to wait long hours before their health care needs are addressed.
In chronically understaffed nursing homes, care problems can go unresolved for months making it more likely for bedsores to develop.
Understaffing may lead to stage 3 bedsores, as caretakers are:
- Less likely to notice or treat bedsores in their early stages
- At a greater risk of forgetting to care for every resident
- More likely to leave a resident in bed or a wheelchair for too long
Has your loved one suffered from a stage 3 bedsore?Get a free case review to get justice.
You May Like: Icd 10 Venous Stasis Ulcer
What Are The Symptoms Of Bedsores
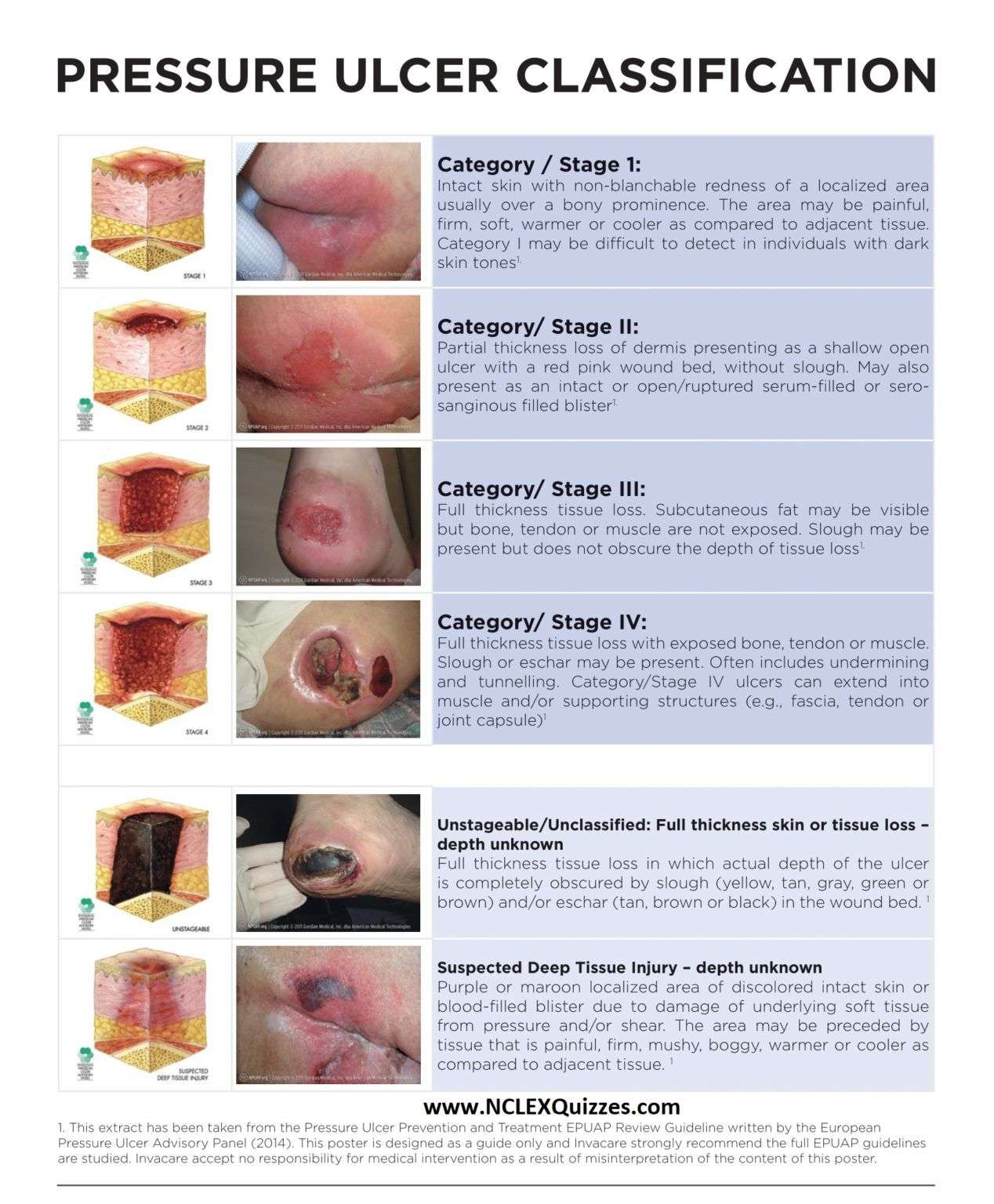
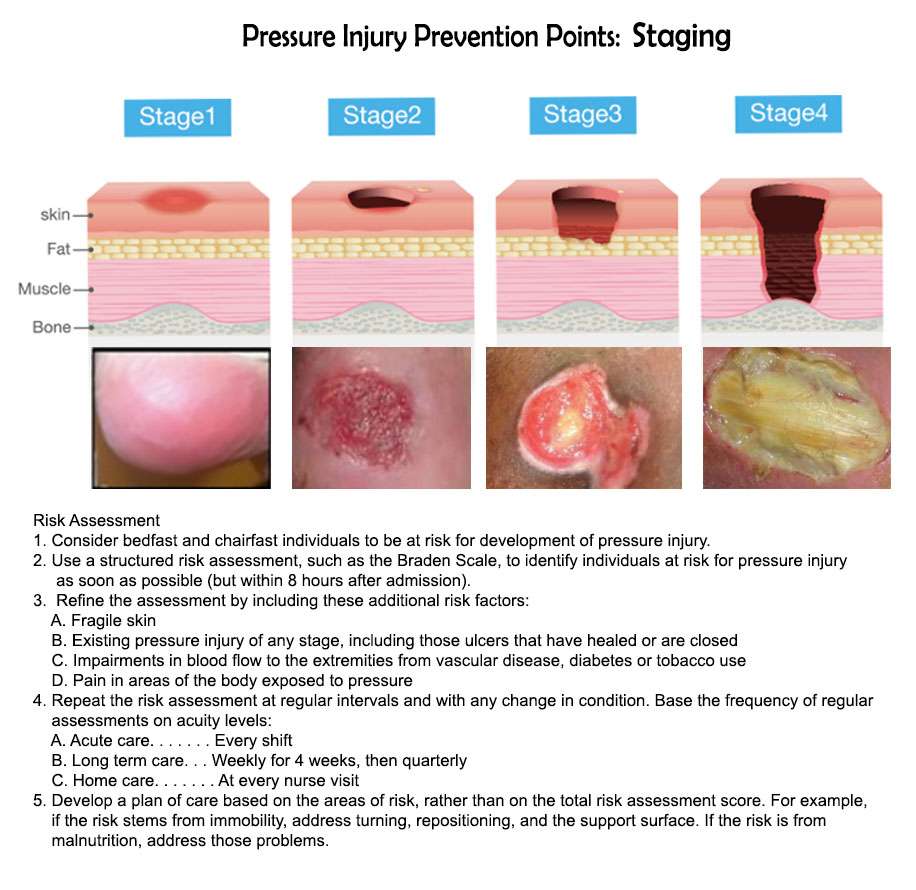
Bedsores are divided into 4 stages, from least severe to most severe. These are:
- Stage 1. The area looks red and feels warm to the touch. With darker skin, the area may have a blue or purple tint. The person may also complain that it burns, hurts, or itches.
- Stage 2. The area looks more damaged and may have an open sore, scrape, or blister. The person complains of significant pain and the skin around the wound may be discolored.
- Stage 3. The area has a crater-like appearance due to damage below the skin’s surface.
- Stage 4. The area is severely damaged and a large wound is present. Muscles, tendons, bones, and joints can be involved. Infection is a significant risk at this stage.
A wound is not assigned a stage when there is full-thickness tissue loss and the base of the ulcer is covered by slough or eschar is found in the wound bed. Slough may be tan, grey, green, brown, or yellow in color. Eschar is usually tan, brown or black.
The Nurses Role In Pressure Ulcer Prevention
Nurses have more touchpoints with patients than any other member of the care team. As a result, the nurses role in pressure ulcer prevention is greater than most. To prevent pressure ulcers from forming, nurses should:
- Check patients for factors that increase their risk of developing an ulcer
- Turn the patients every 2 – 6 hours, depending on their risk factors
- Use barrier creams to manage moisture
- Keep patients well-hydrated
- Ensure patients have good nutrition
You May Like: How To Heal Stomach Ulcers Naturally
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Risk Factors For Pressure Sores

A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.
Don’t Miss: What Is The Recommended Diet For Horses With Ulcers
What Increases The Risk Of Developing Pressure Ulcers
People who are confined to a bed or chair for example due to stroke, spinal injury or dementia are at greater risk of developing extensive pressure ulcers. Other risk factors include:
- immobility being confined to bed after an illness or surgery, or due to paralysis
- diabetes and other health conditions that can affect blood supply
Recommended Reading: How Do You Treat A Duodenal Ulcer
What Is The Outlook For Pressure Sores
The outlook for pressure sores is usually good if they are treated before they reach an advanced stage and before any complications develop.
The outcome can be much worse for advanced stages of pressure sores that arent treated early enough. The outcome will also depend on where the pressure sore is on your body, your general well-being and how well you respond to the treatments.
If you have a pressure sore, youre more likely to develop another pressure sore in the future.
Further reading and references
Read Also: What’s The Signs Of An Ulcer
How Can You Tell If You Have A Pressure Sore
Sometimes, a pressure ulcer can be difficult to identify, especially in the early stages. Here is some information about the symptoms and signs that may indicate that you have a stage 1 pressure ulcer.
- Discolored, reddened, or darkened skin is one of the first signs of a pressure ulcer. For individuals with darker skin, purple, bluish, and shiny areas are one of the first signs. The area may feel warm or hard.
- If you remove pressure from the afflicted area for 30 minutes and the skin does not go back to normal, a pressure ulcer has begun to form.
- Press on the afflicted area with your finger to do the blanching test. Once the area goes white, you should remove the pressure. If the area remains white, this means blood flow has been impaired. The blanching test may not be as effective when it comes to dark skin.
New Wound Therapytopical Pure Oxygenappears Effective In Healing Food Ulcers
Investigators from Midwestern University invited 73 people who had diabetes, both type 1 and 2, to participate in a study to test this new treatment for diabetic foot ulcers.
They found that nearly 42% of those who were randomly assigned to receive the oxygen therapy experienced significant symptom relief, compared to just 13.5% of those who were treated with regular room air for 12 weeks.2
This new food ulcer therapy is called TWO2 for Topical Wound Oxygen home care therapy. The treatment involves placing an inflatable chamber, similar to a large stocking, over the wound, and then an oxygen generator fills the chamber with pure oxygen administered under pressure.2
As a result of the oxygen therapy, Dr. Frykberg says, âit stimulates production of collagen, growth factor, new blood vessels and increased ability to fight infection.â
Oxygen has long been viewed as crucial in the wound-healing process,3-7 the researchers say. For years, hyperbaric oxygen therapy has been studied intensely to heal foot ulcers and prevent amputation. But results remain inconsistent, the researchers say.
However, Dr. Frykberg and his colleagues say that the use of topically administered oxygen therapy has been hampered by studies that werenât well designed and complicated by results that were inconsistent.8-10
Also Check: Ulcerative Colitis And Pain Medication
Slide 1: Existing Pressure Ulcers Report
Say:
The Existing Pressure Ulcers Report provides the clinician with a comprehensive list of all residents currently in the facility with at least one existing pressure ulcer during the report week. All ulcers being treated when the report is generated will display. For residents with more than one pressure ulcer, each pressure ulcer will be displayed separately.
Clinicians can use this report to track all residents in the facility with pressure ulcers. This report is also useful for administrators and other management staff who want at-a-glance information about the number of residents with pressure ulcers on specific nursing units or the facility at large and a limited set of ulcer details, such as ulcer age and whether the ulcer is improving or at risk for delayed healing.
The report is not intended to be used as a standalone report to support clinical decisionmaking and care planning regarding pressure ulcer treatment options and interventions and therefore does not display a wide array of ulcer details.
The Existing Pressure Ulcers Report displays weekly resident-level information. For each ulcer, the following information is displayed:
- Days from admission to ulcer onset.
- Ulcer onset date.
- At risk for delayed healing.
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Don’t Miss: Do Ulcers Make You Throw Up
Prevention: Mattresses And Cushions
Protection is the best way to prevent ulcers. Patients who are at risk of developing pressure ulcers should have the skin carefully inspected for any damage or redness twice daily. The skin should be kept clean and dry. Any pressure causing damage to skin or tissue should be immediately eliminated. This can be done with the help of special mattresses, cushions and by many protective devices that can relieve the external pressure on vulnerable areas of body limbs. These specially designed protective devices can be very helpful in patients who thought to be at risk of developing pressure ulcers, or who have pre-existing Grade 1 or 2 pressure ulcers. Classified by their static or dynamic nature, many advanced low tech and high tech support surfaces and overlays are available for patients bound to lie on bed for long periods of time. Static surfaces do not require electrical power, while dynamic surfaces require electrical power for shifting and redistributing the pressure within the surface. Other integrated electronic beds like air fluidised beds and electronic moving air mattresses require high technology and heavy machinery to let air and ceramic sphere particles support the object on a stream mechanically are often costly, noisy and not easily available. Due to lack of substantial evidences and researches, it is difficult to firmly conclude about relative effects of support surfaces.
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Read Also: What Foods Should I Avoid If I Have An Ulcer
You May Like: Can Ulcerative Colitis Come Back After Surgery
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
Cleveland Clinic Heart Vascular & Thoracic Institute Vascular Medicine Specialists And Surgeons
Choosing a doctor to treat your vascular disease depends on where you are in your diagnosis and treatment. The following Heart, Vascular & Thoracic Institute Sections and Departments treat patients with all types of vascular disease, including blood clotting disorders:
Section of Vascular Medicine: for evaluation, medical management or interventional procedures to treat vascular disease. In addition, the Non-Invasive Laboratory includes state-of-the art computerized imaging equipment to assist in diagnosing vascular disease, without added discomfort to the patient. Call Vascular Medicine Appointments, toll-free 800-223-2273, extension 44420 or request an appointment online.
Department of Vascular Surgery: surgery evaluation for surgical treatment of vascular disease, including aorta, peripheral artery, and venous disease. Call Vascular Surgery Appointments, toll-free 800-223-2273, extension 44508 or request an appointment online.
You may also use our MyConsult second opinion consultation using the Internet.
The Heart, Vascular & Thoracic Institute also has specialized centers and clinics to treat certain populations of patients:
Read Also: Liver Disease Associated With Ulcerative Colitis
Read Also: Crohn’s Ulcerative Colitis Recipes
Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
Questions For Your Doctor
- What should I do if I or a loved one has pressure sores and is too heavy to move?
- Does an adjustable bed help reduce the risk of pressure sores?
- Can you die from an infected pressure sore?
- Is diabetic foot ulcer the same as a pressure sore?
- Can you get pressure sores from sitting in the same position in your job for longer than 2 hours at a time?
You May Like: Nursing Diagnosis For Ulcerative Colitis
Causes Of Itchy Bumps On Buttocks
What causes water blisters on buttocks? There is an array of causes that might be causing you the bumps or the painful blister on buttocks. The symptoms in terms of how severe itching or pain is will depend on what the underlying cause of the blisters is.
Some causes might be mild and clear on their own without any medical treatment. For some causes, due to their infectious nature, urgent treatment to limit its spread is highly recommended. Some of the common cause of blister on buttocks might include the following.
Read Also: How To Manage Ulcerative Colitis Pain
Slide 3: Sample Weekly Wound Rounds Report
Instruct trainees to look at the Weekly Wound Rounds Report handout. Review the report contents and point out special features.
On-Time Weekly Wound Rounds ReportUnit: A
| X |
Key: SA = surface area MVI = multivitamin Prot = protein.POA* indicates that the pressure ulcer was present on admission but has gotten worse in ulcer stage since admission.
You May Like: Is Salmon Good For Ulcerative Colitis
How Does A Pressure Ulcer Heal
With careful and consistent care, a bedsore can heal fully. The larger the pressure sore and the more advanced it is, the more time it will take to treat it. Again, a pressure ulcer takes days/weeks to develop and will take equally as long to fully heal.
There are many treatments for bedsores, most of which you can do yourself at home. Here is how to properly care for a pressure ulcer in the early stages. If you think your pressure sore has progressed to a stage 3 or 4, it is important to work with a medical professional to ensure proper healing and prevention of infection. It is important to recognize that in its late stages, a pressure ulcer is an open wound that is susceptible to infection, especially in those who may be immune-compromised.
Treating Stage 3 Bedsores
Wound care is essential to start the healing process for a pressure injury. Those with stage 3 bedsores should go to a doctor right away for treatments.
Treatment of stage 3 bedsores may include:
- Antibiotics to fight infection
- A special bed or mattress to help with recovery
- Debridement the surgical removal of dead tissue
- Taking pressure off of the bedsore
Treating these injuries can be difficult because deep sores often require surgery and heal slowly. That said, its important to seek treatments because the alternatives a risk of stage 4 bedsores or life-threatening infections are much worse.
Do you or your loved one have a stage 3 bedsore? Learn if you qualify for compensation to cover medical bills. Call .
Also Check: Ulcerative Colitis Is It Deadly