How Pressure Sores Develop
Blood flows through the bodys tissues, including the skin. If you press your finger down on a spot your arm and then quickly remove your finger, you will see that the skin changes color for a second or so in that spot because you stopped the blood flow. The longer your finger remains, the longer the blood flow stops. This is how a pressure ulcer forms.
Someone who cannot move about in bed or on a chair is at highest risk of developing pressure ulcers wherever their body is in contact with the bed or chair, no matter how soft the mattress or cushioning may be. Although a pressure sore can occur anywhere on the body, the most common places are the:
- Coccyx
- Ears
- Heels
- Ankles
People who use prosthetics after a leg or arm amputation are also at risk for pressure sores if their prosthetics dont fit properly or if there is a problem with the skin that comes in contact with the device.
Daily Skin Care To Prevent Pressure Sores
Ways to prevent pressure injuries include:
- Checking the skin at least daily for redness or signs of discolouration.
- Keeping the skin at the right moisture level, as damage is more likely to occur if skin is either too dry or too moist.
- Using moisturising products to keep skin supple and prevent dryness.
- Never massaging bony areas because the skin is too delicate.
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
What is a Pressure Ulcer?
There are many contributing factors.
Also Check: Why Do I Keep Getting Mouth Ulcers
Symptoms Of Pressure Ulcers
The parts of the body most at risk of developing pressure ulcers are those that are not covered by a large amount of body fat and are in direct contact with a supporting surface, such as a bed or a wheelchair.
For example, if you are unable to get out of bed, you are at risk of developing pressure ulcers on your:
- shoulders or shoulder blades
If you are a wheelchair user, you are at risk of developing pressure ulcers on:
- your buttocks
- the back of your arms and legs
- the back of your hip bone
Stage 4 Bedsore Therapy
Stage 4 bedsore treatment is more accurately described as stage 4 bedsore management for most elderly patients. Although stage 4 bedsore treatment can be aimed at actually healing the open wound, many elder patients are not healthy enough to fully recover from a stage 4 bedsore. As a result, there are many medical processes in place that focus entirely on minimizing pain and discomfort for an elderly person with stage 4 bedsores.
Stage 4 bedsore management may involve the following:
Berman, Kevin. Pressure Ulcer.Medline Plus. Atlanta: 2012. < > .
Bluestein, Daniel and Ashkan Javaheri. Pressure Ulcers: Prevention, Evaluation, and Management.American Academy of Family Physicians. 2008. < > .
FREE Case Evaluation
Read Also: Difference Between Colon Cancer And Ulcerative Colitis Symptoms
Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin < 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
You May Like: How Do They Treat Ulcerative Colitis
What Are The Risk Factors For Bedsores
Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care. People with diabetes, circulation problems and malnutrition are at higher risk.
Also Check: Foods To Avoid With Ulcerative Colitis
Notable Adverse Drug Reactions
- Vancomycin may be oto- and nephrotoxic it may also cause blood dyscrasias, rashes, Steven-Johnsons syndrome, toxic epidermal necrolysis muscle spasm, pain, phlebitis, vasculitis, severe hypotension and flushing of the upper body are otherpossible complications. Its use should be restricted to cases of MRSA).
Facts About Pressure Injuries
Pressure injuries are most likely to occur in older adults, particularly those who live in nursing homes. Studies show that more than 1 in 10 nursing home residents have suffered from a bedsore.
Those with chronic illnesses like diabetes and those who are under nourished are at greater risk. People who smoke or have fragile skin are also at greater risk for sores.
If found and treated quickly, pressure injuries should heal within a matter of weeks. But if left untreated, they can quickly worsen.
You May Like: How To Get Rid Of Mouth Ulcers Overnight
Clinical Case Presentation: Pressure Ulcer Management
Thorough wound assessments and sensible product selections are essential for preventing and treating wound infections, managing exudate and finally restoring skin integrity.
This is the clinical case presentation of Fernanda Cortes from Chile who explains step by step how she treated the stage 3 pressure ulcer of a 60-year-old family father. Through her commitment and the effective combination of Prontosan®, Askina® and Linovera® the patient eventually recovered.
Please note that the pictures in the video may be disturbing to sensitive persons.
Read Also: Diet When You Have An Ulcer
Enhancing Healthcare Team Outcomes
The primary goal is to prevent pressure ulcers through various means including the use of air-fluidized or foam mattresses, improving the nutritional status of the patients, proper placing of patients in bed, changing position frequently, and treatment of the underlying diseases. A treatment plan involves the removal of all devitalized tissue that may serve as a reservoir for bacterial contamination . Also, it involves dressing by utilizing hydrogels, hydrocolloids, or saline-moistened gauze to enable granulation tissue to grow and the wound to heal. Treatment of underlying infection by topical or systemic antibiotic medications might be needed to help in the healing process, but tissue culture should be obtained before selecting the accurate drug. Pain and discomfort can be controlled by analgesics. A dietary consult should be made to ensure that the patient is receiving adequate calories. When possible, the patient should be out of bed to chair, and physical therapy should be consulted for ambulation and/or exercise. Wound care specialty trained nurses should assist in dressing changes, debridement of wounds, and provide close followup care. The nurses should also assist the clinician in the education of the patient and family. Pressure ulcers are very difficult to treat, it is crucial that the nurses and clinicians work together as an interprofessional team to provide the very best care including treatment, monitoring, and followup care.
Outcomes
You May Like: What Causes Venous Stasis Ulcers
Failure Of Reactive Hyperaemia Cycle
It is a known fact that tissue distortion causes ischaemia that in turn stimulates protective movements to relieve pressure and circulatory activity to restore normal blood flow in the affected areas. These protective movements are often reflexes as the person is unaware of making them. However, if these prompt actions prove insufficient to relieve ischaemia, the central nervous system is stimulated by constant signals of discomfort and pain to make sure that the pressure is relieved before any permanent damage occurs. Once the pressure is relieved, and the circulation restored, local capillaries begin to dilate and increased blood flow takes place, referred to as reactive hyperaemia. As a result, a bright pink transitory patch appears on the skin, often called blanching erythema because it blanches on pressure unlike the dull red non-blanching erythema that indicates tissue damage . Reactive hyperaemia ensures a rapid restoration of oxygen and carbon dioxide balance it also flushes out waste products. Erythema subsides as soon as tissues are restored to their resting state.
Various grading of pressure ulcer . A very severe trochanteric pressure ulcer where destruction is so severe that the femoral head dislocated and came out
How Do Pressure Sores Begin
Pressure sores develop for many reasons, so hospitals should have strategies in place to screen for risks among all of their patients. However, there are certain environments that lend themselves particularly to pressure injury development, including moisture, shear, advanced age, limited mobility and lack of access to monitoring technology. Its important to be vigilant with proactive screening for bedsore development, especially with high-risk patients.
Here are the early warning signs of a pressure sore:
- Discoloration or dark skin, whether redder, bluer or more purple than usual
- An area of skin feeling warmer to the touch than surrounding skin
- Skin that feels firmer in one spot than usual
- Itchy, painful skin
- When the skin is pressed down on, it doesnt appear lighter
- Swelling on the skin
Recommended Reading: What Does An Ulcer Look Like
Some Areas Are More Prone To Infections
Any pressure sore where the skin has broken is susceptible to infection, but the risk is higher when the sore is located around the coccyx or buttocks, particularly if the patient is incontinent, unable to control bowel or bladder. Urine and stool are harsh on the skin and can contribute to the skin breaking down. Once there is a break in the skin, the constant moisture or irritation increases the risk of infection.
Deep Tissue Pressure Injury: Persistent Non
A deep tissue pressure injury presents as a localized area of persistent deep red, maroon, or purple discoloration that does not turn white when pressure is applied, or a separation revealing a dark wound bed or blood-filled blister. Pain and temperature change will often precede skin color changes. Discoloration may appear differently in darkly pigmented skin.
For more information on pressure injuries and preventive medicine, turn to MD at Home, the premier healthcare resource for primary care and geriatric medicine for homebound patients in the Chicagoland area.
Don’t Miss: Easy To Digest Foods For Ulcerative Colitis
Treating And Preventing Pressure Ulcers
Treatment for pressure ulcers includes the use of dressings, creams and gels designed to speed up the healing process and relieve pressure. Surgery is sometimes recommended for the most serious cases.
For some people, pressure ulcers are an inconvenience that require minor nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning or gangrene.
Read more about the complications of pressure ulcers.
Pressure ulcers can be unpleasant, upsetting and challenging to treat. Therefore, a range of techniques is used to prevent them developing in the first place. These include:
- regularly changing a personâs position
- using equipment to protect vulnerable parts of the body such as specially designed mattresses and cushions
Read about treating pressure ulcers and preventing pressure ulcers for more information.
Unfortunately, even with the highest standards of care, itâs not always possible to prevent pressure ulcers in particularly vulnerable people.
Negative Pressure Wound Therapy
This is an invaluable tool in the management of pressure sores and involves the application of sub-atmospheric pressure to a wound using a computerised unit to intermittently or continuously convey negative pressure to promote wound healing. NPWT, is effective for deep, cavitating, infected and copiously discharging pressure ulcers, particularly with exposed bone. With growing clinical experience it can be said with certainty that it assists wound healing, and its benefits can be summarised thus:
-
Assists granulation.
-
Applies controlled, localised negative pressure to help uniformly draw wounds closed.
-
Helps remove interstitial fluid allowing tissue decompression.
-
Helps remove infectious materials and quantifies exudates loss.
-
Provides a closed, moist wound healing environment
-
Promotes flap and graft survival.
-
Both hospital and domiciliary use.
-
Reduces hospital/dressings/nursing cost .
Read Also: Foods That Prevent Stomach Ulcers
Severity Of Pressure Ulcers
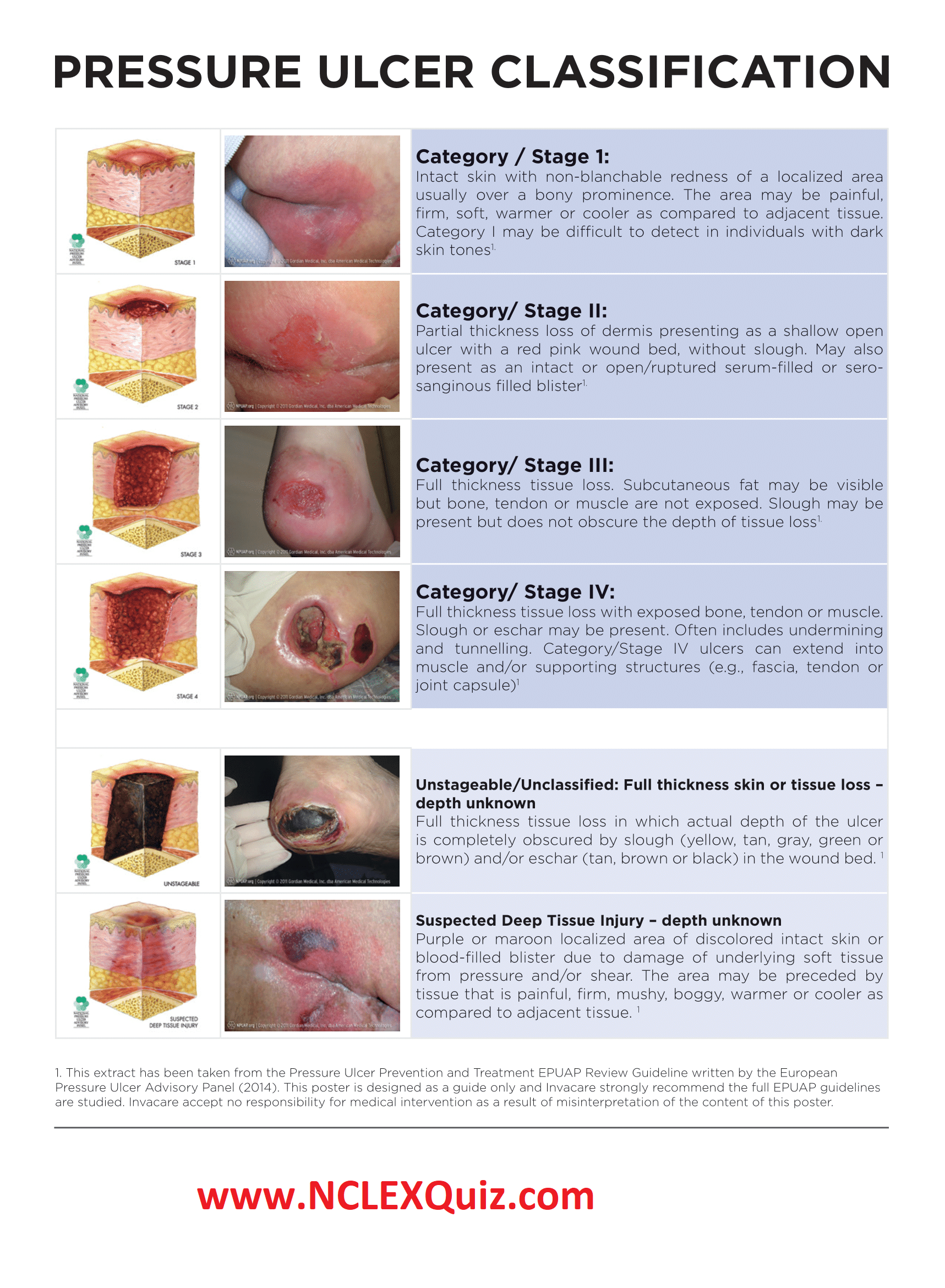
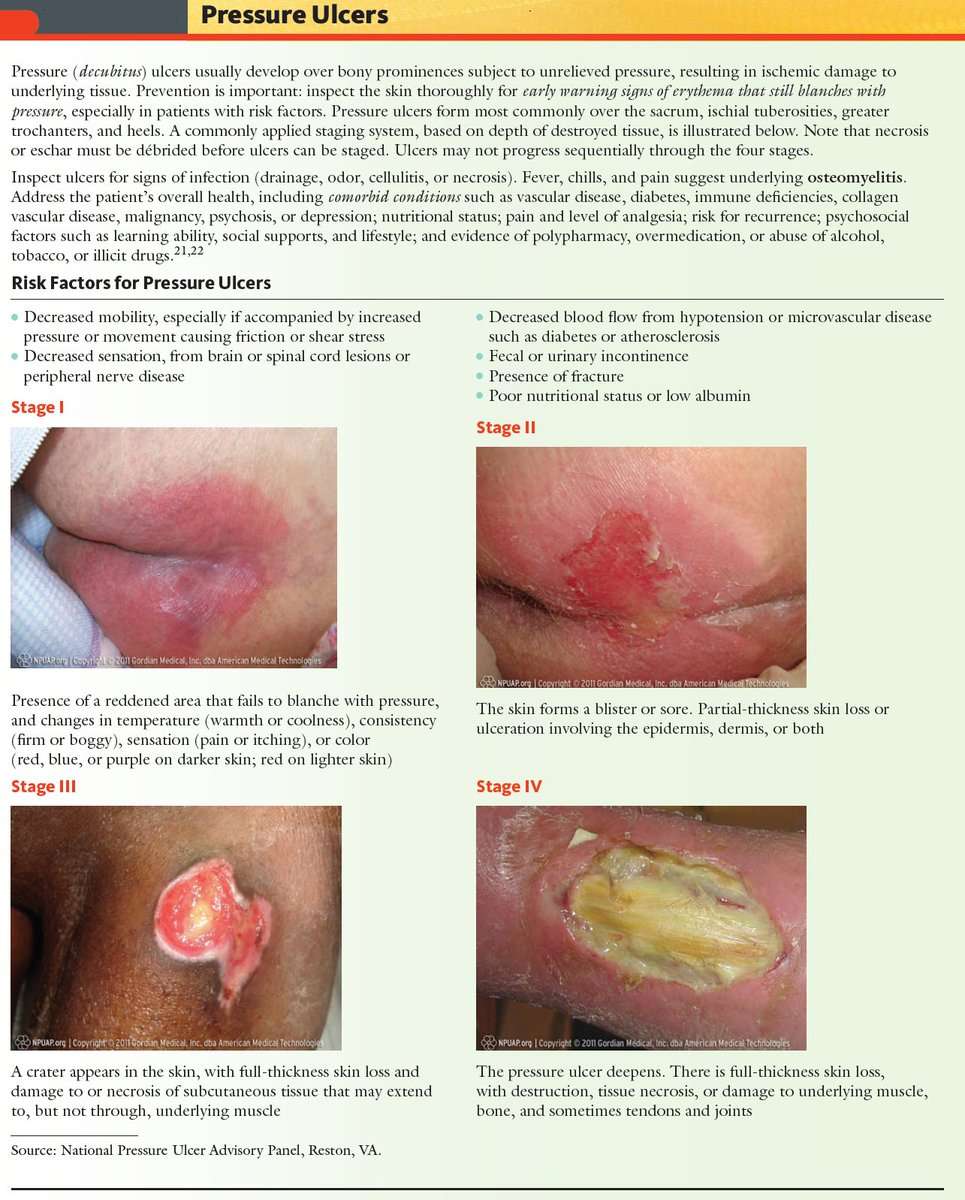
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
Stage 4 Bedsore / Decubitus Ulcer
Stage 4 Bedsore is the last and most serious stage of all bedsores. In a stage 4 bed sore the patient has large-scale destruction of tissue, muscle and skin occurs. Such massive loss of tissue can also include, along with damage to muscle, bone, and even supporting structures such as tendons and joints. Stage 4 bed sores or decubitus ulcers usually require surgery to remove decayed or necrotic tissue. If aggressive treatment of a stage 4 bedsore is not taken, then further necrosis and infection can lead to septacemia, possible needed amputation and even death.
Stage 4 medical treatment include debridement, constant changing of dressing & cleansing for proper wound care, electrical stimulation and surgery. Stage 4 surgery may consist of excising of pressure ulcer, surrounding scar, bursa, soft tissue calcification, and underlying necrotic or infected bone. On deeper stage 4 bedsores and decubitus ulcers a flap surgery is needed to close the wound, fill in the dead space thus enhancing vascularity of the healing wound, and distributing pressure off the bone. All stage 4 bedsore were Stage 3 bedsores at one time, but due to the lack of quality medical and nursing care, the pressure sore continued to get worse and progressed.
Neglect is the Major Cause of a Stage 4 Bedsore
Don’t Miss: Is Keto Good For Ulcerative Colitis
Whos At Risk Of Stage 4 Bedsores
Anyone with a lower-stage bedsore is at risk of a stage 4 sore. However, some patients may be more prone to this type of injury.
At particularly high risk are those:
- With Limited MobilityMovement is the key to preventing bedsores of any stage. If an older person cannot move on their own, they may sit or lie in the same position for hours. This can cut off blood flow to their skin and cause a bedsore.
- Who Are In Understaffed Nursing HomesNursing home residents with mobility issues must rely on staff members to prevent bedsores. Sadly, some care facilities may fail to prevent bedsores due to issues like understaffing and poor training.
- Who Have Alzheimers or DementiaIf residents with mental impairments develop a bedsore, they might not be able to tell anyone due to their condition. Theyll need to have someone else find it and help them get the proper care. Residents with these conditions may also have trouble sensing pain.
- Other FactorsResidents are at higher risk of bedsores if they have blood flow or circulation problems, diabetes, or poor nutrition or if they wear a cast.
Our trusted advocates can help you and your loved one take legal action. Call us today at .
Assessing Sacral Pressure Ulcers
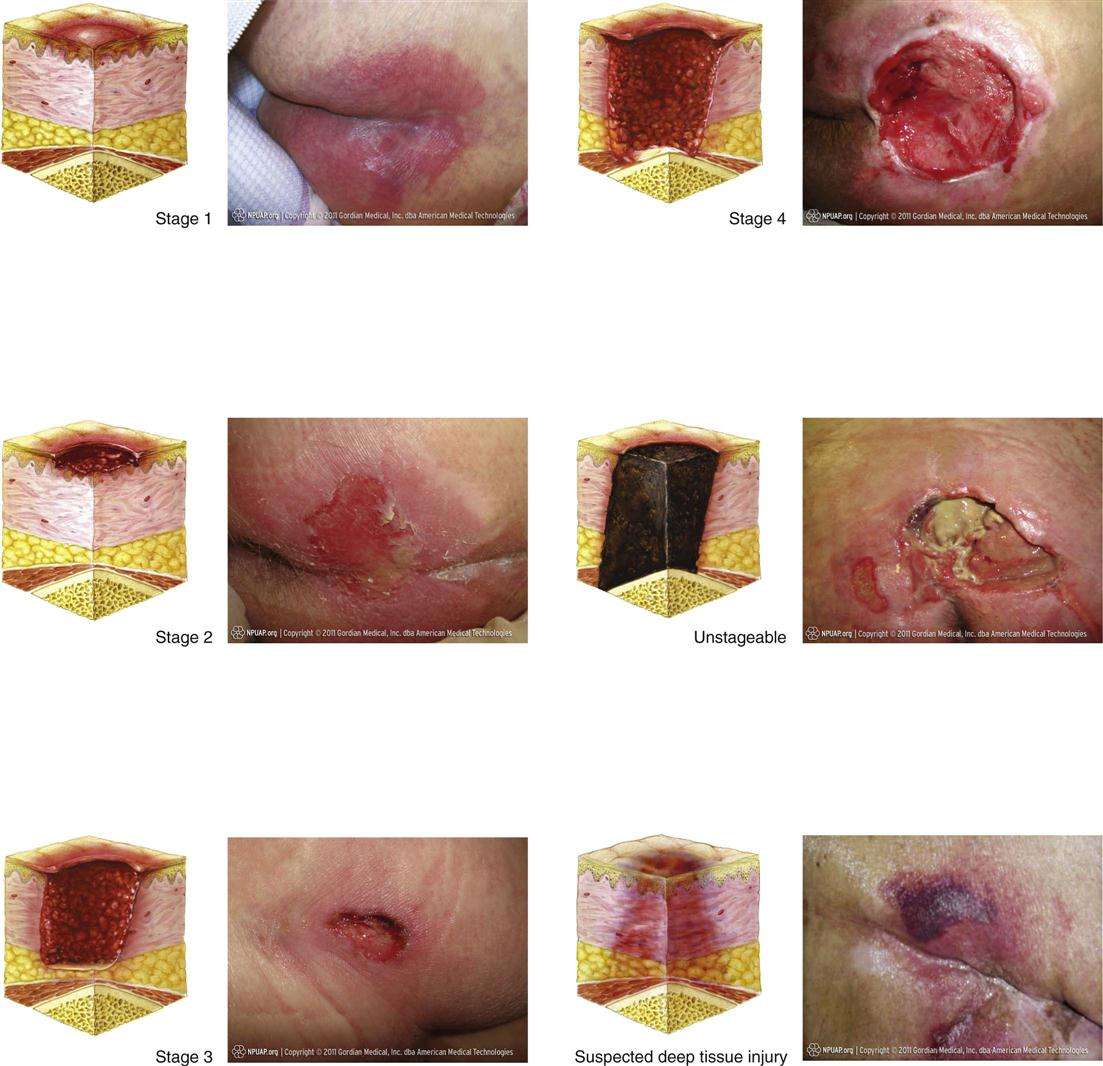
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Also Check: What Dies A Stomach Ulcer Feel Like
Stages Of Pressure Ulcers
Casey Gallagher, MD, is board-certified in dermatology and works as a practicing dermatologist and clinical professor.
If a loved one has been severely injured or is extremely ill, they may need to spend a significant amount of time in bed. Prolonged immobility, while beneficial to recovery, can become problematic if it places persistent pressure on vulnerable skin. Unless preventive steps are taken, pressure ulcers, also known as decubitus ulcers or bedsores, can develop.
Other Tips For Preventing Pressure Ulcer
1. Check the skin daily for any signs or symptoms of pressure ulcers. The patients can take the help of Bedside Wound Care Services for this. 2. Maintain a healthy and balanced diet that contains sufficient and enough protein with good sources of vitamins and minerals.3. Quit smoking. People who smoke are more prone to develop pressure ulcers due to the damage caused to blood circulation. 4. For repositioning, wheelchair push-ups are good where the person can raise their body off the seat by pushing on the arms of the chair. The use of cushions or special mattresses is also prescribed to release pressure and ensure a well-positioned body. Avoid doughnut cushions as they can put pressure on surrounding tissues.5. Ensure regular pressure ulcer dressings to avoid any type of infection and effective wound healing.
Recommended Reading: New Treatment For Ulcerative Colitis 2020