Is Ulcerative Colitis Genetic
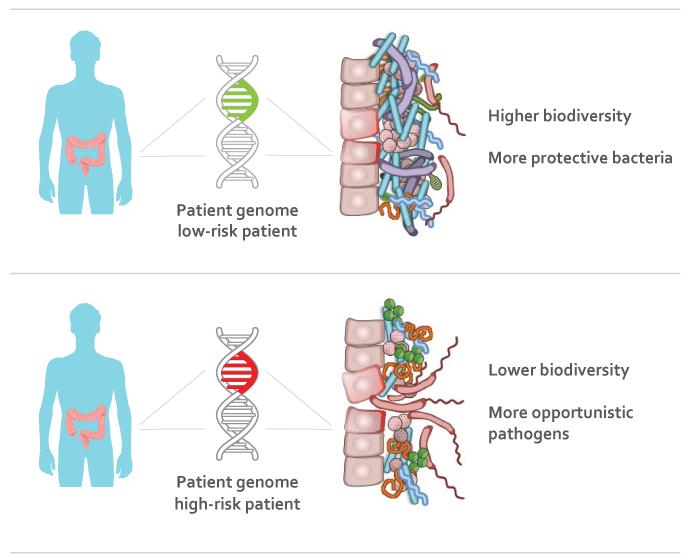
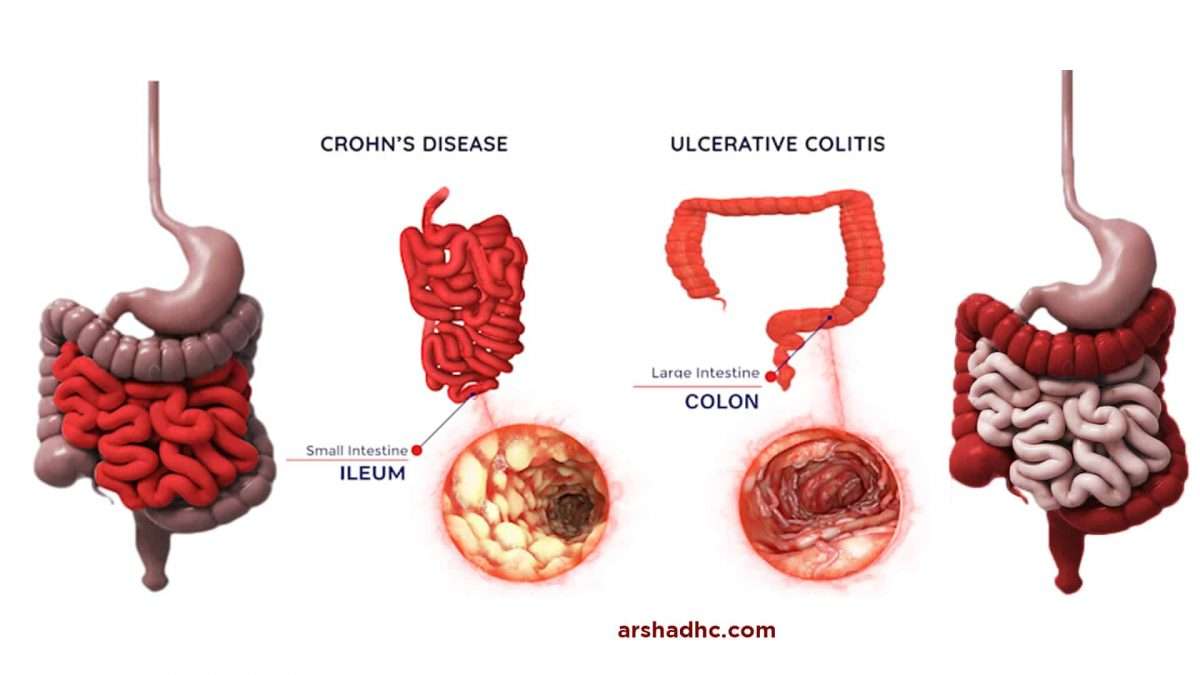
Ulcerative colitis is a form of inflammatory bowel disease thought to be brought on by immune system dysfunction. The causes of UC are complex, involving both genetic and environmental factors.
Researchers are still learning about what exactly causes UC. Studies of the human genome show that there is a genetic component to the disease, meaning some hereditary risk factors can increase the chance of developing UC. However, there is still a lot to learn about the specific genes involved and how they affect the pathogenesis of UC.
Although there is a genetic component to colitis, environmental risk factors seem to have a much bigger impact on the development of UC.
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
-
You may find a âLow Residueâ approach helpful. We have seen it work well for some people
-
Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day
-
Some studies show that a higher fiber diet can improve IBD conditions
A Twocomponent Hypothesis For Pathogenesis Of Ulcerative Colitis
This hypothesis was proposed based on experimental studies showing that intestinal microorganisms in severe ulcerative colitis are pathogenic, as evidenced by allergic and immunological reactions, proved by agglutination and skin tests.47 Similar results were obtained in other intestinal diseases, which point to the existence of a nonspecific inflammation owing to intestinal microorganisms acquiring pathogenicity. Such a process may be superimposed on primary lesions of various origins, including that in the disease inappropriately termed ulcerative colitis.
The potential weakness of this hypothesis might be the experience that patients with severe ulcerative colitis do not need antibiotics for treatment. By using this hypothesis, it is also difficult to explain the abrupt line of demarcation between normal and inflamed mucosa of the colon seen in patients with ulcerative colitis.
In view of this hypothesis, and to avoid incorrectness in and ambiguity of the term ulcerative colitis, the term idiopatic proctocolitis was proposed for the disease entity.51,53,56 This term covers both the mild haemorrhagic and the severe ulcerative form of the disease, and aptly states its main characteristicsnamely, the constitutional character and predilection for association of the rectum.
Read Also: Pressure Ulcer Interventions And Rationales
Box : Abnormalities Of Epithelial Cells In Ulcerative Colitis
- Deficient oxidation
- Abnormal permeability of the cell membrane
- Abnormal mucus composition
- Abnormal cellular responses to stress
- Inability to use butyratestarving colonocytes
- Polymorphisms in the tolllike receptor gene
- Deficiency of both defensins and cathelicidins
An understanding of the role of indigenous bacteria in promoting the development of healthy mucosal barrier function brings new light to the fundamental causes of ulcerative colitis. Manipulation of the intestinal microbial flora, by use of probiotics or antibiotics, may be to be a new and promising therapeutic modality in the near future.
Spoon Up Some Applesauce
Applesauce may be good for an ulcerative colitis diet, according to the University of Wisconsin Health. However, while apples are rich in vitamins and minerals like potassium, their high fiber content can make them difficult to digest, especially during a flare-up, says the Foundation. Go for unsweetened applesauce, or make your own by peeling and cooking apples . Flavor it with your own mix of spices just be sure to skip the sugar.
Recommended Reading: What Should You Eat When You Have Ulcerative Colitis
Genotype Of Top Hit Snp At Hla Loci Showed Significant Association With The Probability Of Colectomy
Using GWAS subjects, we analyzed the associations between the 8 top SNPs identified in GWAS and 3 clinical phenotypes: age at diagnosis, disease extension, and history of total colectomy. No SNPs were associated with age at diagnosis or disease extension. Only HLA loci were significantly associated with history of total colectomy . Based on these findings, we performed further analysis of associations between the genotype of rs117506082 and the probability of total colectomy using the Kaplan-Meier method with follow-up data for 30 years after diagnosis. The characteristics of UC patients in this analysis are shown in Supplementary Table S3. Although the difference was not significant , age at diagnosis tended to be earlier in patients with the GG genotype than in patients with the GA or AA genotype . There were significant differences in disease location between the GG and GA+AA genotypes , and patients with the GG genotype tended to have limited disease extension. We found that patients with the GG genotype rs117506082 at the HLA loci did not undergo colectomy, and those with the GG genotype had a significantly lower probability of total colectomy than patients with the GA or AA genotype of rs117506082 .
Colectomy-free probability stratified by genotypes of rs117506082 using the Kaplan-Meier method.
Role Of Epithelial Cells
Over the past two decades, many abnormalities have been described in the epithelial cells of patients with ulcerative colitis . This, conceptually, is based on the anatomical distribution of inflammation, which in the case of ulcerative colitis is associated predominantly with the rectum. Why such abnormalities are seen in patients with ulcerative colitis still remains elusive. The question is whether luminal factors, autoimmunity or a genetic basis is the major contributor to the aetiology of ulcerative colitis, or whether some combination of any or all of them accounts for the development of the disease.19,20
Figure 1Schematic view of the current concept of the aetiopathogenesis of ulcerative colitis and inflammatory bowel disease. Genetic susceptibility, bacterial antigens and disturbed mucosal immune response are the major factors of intestinal inflammation. Modifying factors may further serve as triggers or suppressors of the inflammation. HLA, human leucocyte antigen IFN, interferon IL, interleukin MDR1, multridrug resistance gene 1 NF, nuclear factor TNF, tumour necrosis factor UC, ulcerative colitis.
Don’t Miss: How To Tell If You Have A Stomach Ulcer
The Heredity Implications Of Pregnancy With Ibd
If you or a relative has Crohn’s disease or ulcerative colitis, you might wonder what role family history plays in IBD, especially when it comes to having children of your own. We’re here to help you understand how IBD can be passed down through families, so you can be informed as you prepare for the road ahead.
Of course, talking with a doctor who specializes in the treatment of IBD in pregnancy is the best way to understand your specific situation, but you can get more IBD information by exploring the questions and answers below.
Treatment Of Ulcerative Colitis
Part 8 of Is ulcerative colitis genetic?
There is no cure for the condition, but medications and lifestyle changes can help treat the symptoms and improve quality of life. Medications are generally prescribed based on the severity of the disease and often have to be tailored to the individual patient.
Recommended Reading: How Do You Get Rid Of Leg Ulcers
Proper Nutrition Is Important For People Who Have Ulcerative Colitis
Good nutrition is important for everyone, but even more so if you have an inflammatory bowel disease . When you have ulcerative colitis , it can be difficult to figure out what to eat which foods contain the valuable nutrients your body needs without putting you at risk for a flare up.
Proper nutrition can improve response to medication, reduce risk for flares, and improve recovery time when sick, says Kelly Issokson, RD, a clinical dietitian with the Nutrition and Integrative IBD Program at Cedars-Sinai in Los Angeles.
Healthy eating becomes especially difficult with UC when youre on the move, and who isnt these days?
To help keep you on the path to eating well, here are 13 dietitian recommended snacks for people with UC.
Also Check: Can Stomach Ulcer Cause Fever
Hygiene And Old Friends Hypotheses
A high frequency of ulcerative colitis in the industrialised countries supports the idea that environmental factors have a dominant role in its aetiopathogenesis. The hygiene hypothesis states that in raising children, an extremely clean environment negatively affects the development of the immune system and, thus, predisposes them to immunologically driven diseases, such as allergy or ulcerative colitis. An important role is assigned to the helminths, because until modern times, most children were colonised by them early in life. Helminths regulate the host’s immune system and prevent an excessive inflammatory reaction.57
Read Also: How Do They Check For Ulcers
Foods That May Fight Uc
Some research shows that certain nutrients may help fight the irritation and swelling in your gut caused by UC. Scientists have studied how linoleic acid affects people with the condition. Although everyone needs this âgoodâ fat, donât overdo it, since there is some evidence it may play a role in inflammation if you get too much.
Other studies show that an omega-3 fatty acid called EPA may fight inflammation. This is another âgoodâ fat that blocks certain chemicals in your body called leukotrienes. Fish oil is a good source of EPA. In some studies, folks with UC saw some benefits when they took high doses. Many people, though, didnât like the fishy taste. There is also some evidence that adding fish oil to aminosalicylates may be helpful, but this isnât proven. DHA is another omega-3 found in fish oil that can fight inflammation and is used by some people with UC.
Some research also shows that yogurt with gut-healthy bacteria, called probiotics, eases inflammation. Scientists are still studying how they may help people with UC and similar conditions. Some people also believe that a diet low in FODMAPs â a type of highly-fermentable carbs found in meats, fruits, dairy, and lots of other foods â may help ease UC symptoms. But the evidence is unclear if it does. And without close monitoring, any diet that restricts certain foods may lead to poor nutrition and other problems.
Show Sources
What Foods Should I Not Eat When I Am Having An Ulcerative Colitis Flare
Certain foods can exacerbate or aggravate an UC flare and should be avoided. They are more likely to trigger cramping, bloating, and/or diarrhea and are also not recommended in people diagnosed with a stricture, which is a narrowing of the intestine caused by inflammation or scar tissue, or in those who have had recent surgery. Examples include:
- Foods high in insoluble fiber that are hard to digest, such as seeds, raw green vegetables , whole nuts, whole grains, or fruits with a skin
- Lactose, which is milk sugar found in dairy products, milk, cream, cream cheese, and soft cheeses
- Non-absorbable sugars such as sorbitol, mannitol, and other sugar alcohols that are typically found in sugar-free gum, candy, ice cream, and certain types of fruits and juices such as pear, peach, and prune juice
- Sugary foods such as candy, pastries, and juices
- High-fat foods such as butter or margarine, coconut oil, or fatty, fried, or greasy food
- Spicy foods
- Alcohol such as beer, wine, or spirits
- Caffeinated drinks such as coffee or energy drinks
- Soda.
You May Like: Can You Feel A Stomach Ulcer
Our Bodies & Inflammation
Our bodies are amazing machines. Yes, I call them machines. They have the power to detoxify and fix small problems all on their own. However, sometimes we need to give it a little helping hand. Thats where nutrition comes into play!
Inflammation can also be caused by saturated fats. Think greasy food, pizza, cheeses etc. The best way to diminish this inflammation in the body is through consumption of omega 3 also know as a Healthy Fat. Omega 3 has anti-inflammatory properties that work on decreasing inflammation of fat tissues.
But that is enough of the science. While antioxidants and healthy fats are naturally occurring in the body, it is important to include them in your diet as well to assist your body!
Recommended Reading: What To Take For Stomach Ulcer Pain
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
Read Also: What Does An Ulcer Look Like
Read Also: Pressure Relieving Mattress For Pressure Ulcers
What Is The Role Of The Intestine’s Bacterial Contents In Ulcerative Colitis
Some of the similarities between ulcerative colitis and infectious colitides have led many investigators to search for the unidentified microorganism triggering the chronic inflammation in the large bowel. However, until now, no single microbial agent has been associated, unequivocally, with the development of ulcerative colitis. Many arguments exist against an infectious aetiology of ulcerative colitis .5
Over the past few years, we have gained considerable evidence that it is an abnormal mucosal immune reactivity, against enteric bacteria, that is the key event leading to intestinal injury in patients with IBD. Molecular biology techniques have shown that the intestinal space of an adult may contain > 500 different bacterial species some of them exert a protective role, whereas others are aggressive. The number of bacterial strains along the small bowel progressively increases, with the predominance of Gramnegative aerobes. The bacterial population in the large bowel reaches a density of around 1012 microbes per gram of luminal contents. More than 50% of the bacterial strains cannot be cultured under conditions currently available. In adults, the faecal bacterial composition is host specific and stable over time, with small fluctuations of the strains up to 20% .6
What To Eat On An Ulcerative Colitis Diet During A Flare:
Eating during an Ulcerative Colitis flare needs to be approached with caution. When you are in pain, feeling bloated, and just dont feel like eating, choose foods that are easy to digest.
-
Select refined grains. Refined grains are easier to digest than whole grains. So, select white bread, white rice, and white pasta. Yes, a dietitian is recommending you eat white grains! These foods are sources of B vitamins and Iron.
-
Choose low fiber vegetables and fruits. Low-fiber vegetables are well cooked or canned veggies, mashed potatoes without the skins, and string beans. Cooking veggies helps to break down the fiber. So, when you are flaring, avoid salads and other dishes with raw vegetables. Also, remove the skin from raw veggies and fruits and avoid produce that has seeds such as strawberries and raspberries. Low-fiber fruits are bananas or cantaloupes. For a nutrient-rich drink, reach for low-sodium vegetable juice.
-
Use unsaturated fats. Cook with small amounts of heart-healthy unsaturated oils. Try different oils to replace butter or stick margarine. Aim for a fat intake below 35% of your daily calorie intake. A low-fat diet may help to prevent bloating, cramping, and diarrhea.
-
Reach for calcium-rich foods. For example, low-fat dairy products , canned salmon, and soy products. Oat, soy, or rice drinks enriched with calcium are another option.
Recommended Reading: Is Soy Milk Good For Ulcerative Colitis
Recommended Reading: New Meds For Ulcerative Colitis
Crohns Disease And The Immune System
A persons immune system usually attacks and kills foreign invaders like bacteria, viruses, fungi, and other microorganisms. During a normal immune response, cells travel out of the blood to the intestines and produce inflammation. Under normal circumstances, harmless bacteria thats present in the GI tract are protected from an immune system attack.
Extraintestinal Manifestations And Complications
Aphthous ulcersPyoderma gangrenosum
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes. Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Uveitis and iritis are more commonly associated with ulcerative colitis, whereas episcleritis is more commonly associated with Crohn’s disease.
Recommended Reading: Nanda Nursing Diagnosis For Ulcerative Colitis