Implications For Future Research
In general, there is a lack of studies examining turning frequency and its impact on the development of PU. The limited available studies have limitations in their methodological designs. There is a need for multiple welldesigned RCTs consisting of lesser methodological limitations with a large sample size that compare just the frequency of turning while making other variables constant.Further studies should focus on changing only 1 variable such as turning frequency so that lesser confounding factors exist, yielding more reliable results. This scoping review identified that patients nursed under pressurerelieving devices are less susceptible to PU development. Specifically, repositioning patients coupled with the use of pressurerelieving devices is one of the most promising interventions to implement. However, the challenge is to identify what exactly is the optimal repositioning interval with pressurerelieving devices. Hence, further RCTs need to be conducted to confirm the results from these studies to allow organisations to relook into their intervention guidelines and adopt EBP. Studies should also focus on repositioning intervals on different patient populations to allow for generalisability across different patient populations. This can improve patients quality of life and also relieve nurses of unnecessary workload.
Try To Maintain Nutrition
There is a strong correlation between nutrition deficits and pressure ulcer risk. If your loved one has an appetite, try to maintain adequate nutrition with nutrient-rich foods . If his appetite is waning, offer supplements such as Ensure or Boost to help bolster nutrition.
Nutrition is often a problem in palliative care patients and its important to note here that you should never try to force your loved one to eat.
Reduce Friction And Shear
Friction is the rubbing of skin on an external surface, usually bed sheets. Friction to the most commonly affected areas can be reduced with protective devices. Heel and elbow cradles are typically made of egg-crate material and Velcro on.
Skin protecting dressings, such as films and thin hydrocolloid bandages can protect the skin from repeated friction but wont help reduce pressure.
The most important thing you can do to prevent injury from the friction is to make sure you dont create any yourself when youre repositioning your loved one. Use a draw sheet to help you lift your loved one off the bed when you lift and reposition.
Shear is created when the deeper fatty tissues and blood vessels are damaged by a combination of friction and gravity. The best way to avoid this type of injury is to avoid a semi-Fowler and upright position in bed. A semi-fowler position is where the head is raised less than 30 degrees and upright positions more than 30 degrees.
Now, you obviously cant avoid these positions all of the time. Many patients need to be semi-Fowler to help ease shortness of breath or prevent gastric reflux and all patients need to be in an upright position to eat safely.
To minimize the risk of shear injury in a semi-Fowler or upright position, take precautions to prevent your loved one from sliding down in bed. You can do this by raising the foot of the bed and propping the knees up with pillows.
Don’t Miss: New Meds For Ulcerative Colitis
All Ages: Care Planning
-
Develop and document an individualised care plan for neonates, infants, children, young people and adults who have been assessed as being at high risk of developing a pressure ulcer, taking into account:
-
the outcome of risk and skin assessment
-
the need for additional pressure relief at specific at-risk sites
-
their mobility and ability to reposition themselves
-
other comorbidities
-
patient preference.
Treatments For Pressure Ulcers
Treatments for pressure ulcers depend on how severe they are.
For some people, they’re an inconvenience that needs basic nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning.
Ways to stop pressure ulcers getting worse and help them heal include:
- applying dressings that speed up the healing process and may help to relieve pressure
- moving and regularly changing your position
- using specially designed static foam mattresses or cushions, or dynamic mattresses and cushions that have a pump to provide a constant flow of air
- eating a healthy, balanced diet
- a procedure to clean the wound and remove damaged tissue
Surgery to remove damaged tissue and close the wound is sometimes used in the most serious cases.
Read more about the treatments for pressure ulcers.
Also Check: Home Remedies For Stomach Ulcer In Tamil
Bedsore Causes In Nursing Homes
Bedsores Caused by Nursing Home Neglect
Quick Answer
A 2019 report by the Sun Journal details eldersâ experiences in a Lewiston, Maine nursing home, specifically describing one residentâs death, which was attributed to a stage 4 bedsore. Sadly, this is not an isolated incident. Many underlying bedsore causes stem from nursing home neglect. Too often, nursing home residents suffer from preventable bedsores due to poor or improper care from staff members.
Read Also: Can Stomach Ulcer Cause Fever
Incidence Mortality And Costs
The incidence rates of pressure ulcers vary greatly with the health care settings. The National Pressure Ulcer Advisory Panel says the incidence ranges from 0.4 percent to 38 percent in hospitals, from 2.2 percent to 23.9 percent in skilled nursing facilities, and from 0 percent to 17 percent for home health agencies. There is ample evidence that the majority of pressure ulcers occur relatively early in the admissions process. For patients in the hospital, they can occur within the first 2 weeks. With the increased acuity of elderly patients admitted and decreased lengths of stay in hospital, new data suggest that 15 percent of elderly patients will develop pressure ulcers within the first week of hospitalization. For those elderly residents admitted to long-term care, pressure ulcers are most likely to develop within the first 4 weeks of admission.
Mortality is also associated with pressure ulcers. Several studies noted mortality rates as high as 60 percent for older persons with pressure ulcers within 1 year of hospital discharge., Most often, pressure ulcers do not cause death rather the pressure ulcer develops after a sequential decline in health status. Thus, the development of pressure ulcers can be a predictor of mortality. Studies further suggested that the development of skin breakdown postsurgery can lead elders to have major functional impairment post surgical procedure.
You May Like: What Is A Vascular Ulcer
Sample Size And Sampling Procedure
The sample size was determined using a formula of estimating a single population proportion for cross sectional study. Since the population size is less than 10, 000 , the final sample size was estimated using correction formula. The final sample size obtained including 10% non-response rate was 252. Then, the number of participants in each selected hospitals to obtain similar proportion of participants were determined using the population proportionate sampling . It is estimated using the formula: n=/N total, where, n=Proportion of nurses participate in the study in a given public hospital, nf=Final sample size obtained using correction formula , N=is the total number of nurses in the selected public hospitals .
Read Also: Hindgut Ulcers In Horses Treatment
First Cycle Of Unfreezing: Planning
In this stage, there were some activities to come up with a preliminary diagnosis of the problem, gather data, and giving feedback on the results and the plan for action. The first author and the trained research assistant met several key people including the in-charge and experienced HWs or nurses selected by the in-charge of each NH to learn the issues relevant to pressure ulcers in their homes. They reported on the existing PUs but did not have record of the incidence of PUs. The prevalence of PUs in these four homes ranged from 8 to 10%. Overall, the residence-staff ratio was around four to six. The turnover rate of care staff was acceptable, although this sometimes affected the care that was delivered. They agreed that the occurrence of PUs was an important issue in their homes, and efforts e.g., having a prevention protocol and training to care staff should be made to decrease them.
Read Also: Is Garlic Good For Ulcerative Colitis
Pressure Ulcers In Palliative Care
The prevalence of pressure ulcers is higher in patients receiving palliative care than in the general population . There are estimated to be as many as 40 million people who require palliative care support worldwide . Palliative care is a concept associated with the end of life, and focuses on relieving symptoms and enhancing quality of life. The aim of palliative care may be to heal, improve symptoms or prevent deterioration. The need for palliative care has continued to rise in the UK due to the number of older adults with chronic conditions such as diabetes and heart disease .
Although wound healing may ultimately not be possible in patients who are terminally ill due to time restraints, suboptimal wound care and symptom management can cause unnecessary discomfort and have a devastating effect on the quality of a patients death . By managing pressure ulcer symptoms in patients receiving palliative care, improvement and even healing may be achieved .
Although patients may develop a pressure ulcer at the end of life, this does not mean that it should be accepted as a normal development . Patients with pressure ulcers may experience distressing symptoms such as pain that affect their appetite, prevent them from assuming a comfortable position and cause physical impairment .
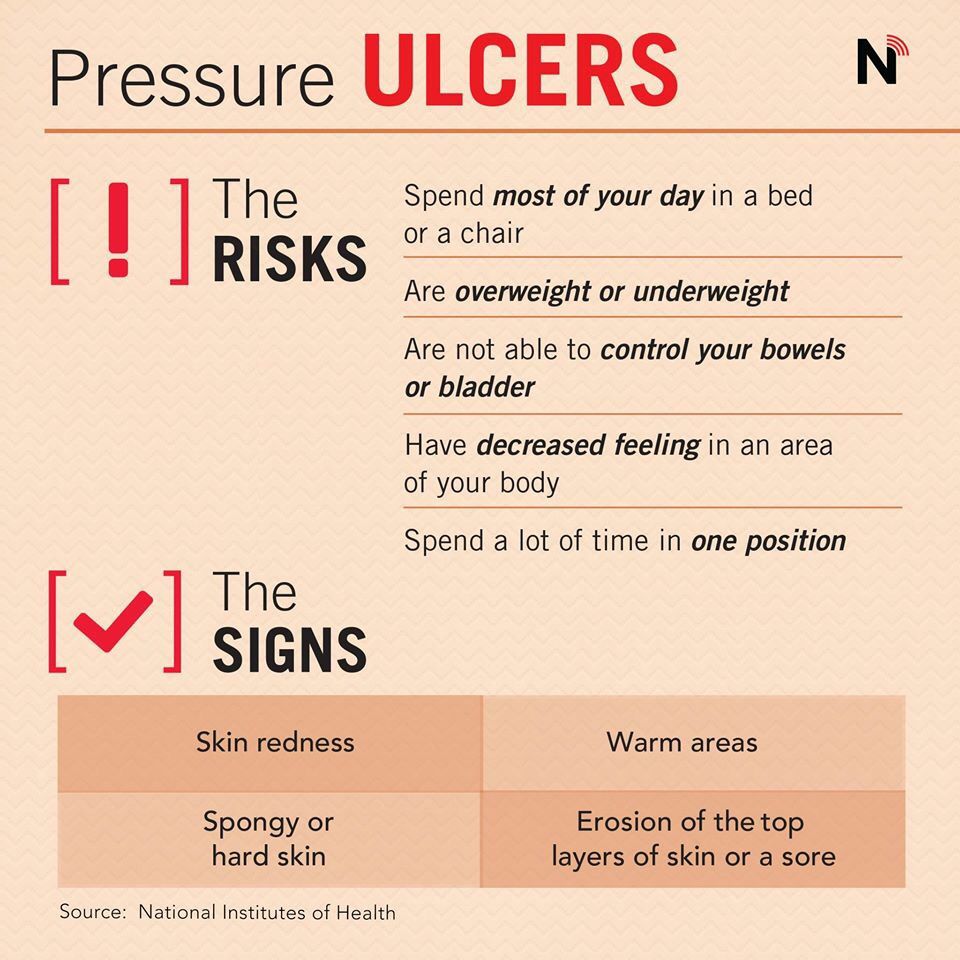
Who Is Most Likely To Get A Pressure Ulcer
Anyone living in a care home can develop a pressure ulcer, but some factors make it more likely.
Risk factors include:
- Limited mobility or being unable to change position without help.
- A loss of feeling in part of the body.
- Having had a pressure ulcer before, or having one now.
- Not having eaten well for a period of time.
- Thin, dry or weak skin.
- A significant cognitive impairment.
You May Like: Home Remedies For Stomach Ulcers During Pregnancy
Special Devices That Can Help You
In addition to turning and repositioning frequently, using a special surface to reduce or relieve pressure can help a great deal. The simplest of these is an egg crate mattress. Many hospice and home health agencies provide these free of charge but they are relatively inexpensive at your local department store.
If your loved one is spending a lot of time up in a chair, egg crate chair pads are also available. An egg crate surface helps distribute pressure more evenly, helping minimize the amount of pressure on one area.
A step up from the egg crate mattress is an air mattress overlay. This type of surface is placed on top of a mattress and typically alternates air pressure in various columns. When using an egg crate mattress or an air mattress overlay, its still important to maintain the turning schedule. These devices dont replace frequent repositioning.
The big guns of pressure-relieving devices are the fluidized air mattresses. These special mattresses contain silicone-coated glass beads that become fluid when the air is pumped through them. These mattresses do a wonderful job of relieving pressure but they have their downside.
The frame of the mattress makes transferring to and from bed difficult. And if the person wants to sit up in bed, a foam wedge would probably need to be used to help support their back. This mattress is really best suited for palliative care patients who are fully bed-bound, have severe pressure ulcers, and are in a lot of pain.
Study Setting And Sample
The study was in Addis Ababa, the capital city of Ethiopia which contains 13 public referral hospitals . There are 34 private hospitals, 86 health centers and various NGOs and health institutions. The data in this study included nurses working from patient admission units in six randomly selected public referral hospitals . The units included were medical, surgical, orthopedics, intensive care unit, gynecology, pediatrics, dermatology, burn and oncology.
You May Like: How Do You Know If You Have Ulcerative Colitis
Bedsores In Nursing Homes
According to the Centers for Disease Control and Prevention , bedsores occur in more than 1 in 10 residents in nursing homes. If left untreated, bedsores can be deadly. Since bedsores can often be prevented with proper care, they may be a sign of nursing home abuse or neglect. You can pursue financial compensation for bedsores by filing a nursing home abuse lawsuit.
You May Like: Budesonide Vs Prednisone For Ulcerative Colitis
Causes Of Pressure Sores
Pressure sores happen if you cant move around and so stay in one position for a long time. We normally move about constantly, even in our sleep. This stops pressure sores developing.
People who are unable to move around tend to put pressure on the same areas of the body for a long time. If you are ill, bedridden or in a wheelchair, you are at risk of getting pressure sores.
A number of things can increase your risk of pressure sores, including:
- being unable to move around easily due to old age or illness
- weight loss – you may have less padding over bony areas
- sliding down in a bed or chair – pressure on the skin cuts off blood supply because the skin is being pulled in different directions
- friction or rubbing of the skin, for example against sheets
- moist skin – for example, due to sweating or incontinence
- other medical conditions, such as diabetes
- having a previous pressure ulcer
You May Like: How To Treat H Pylori Ulcer
Treatment For Decubitus Ulcer
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Read Also: Imodium Ulcerative Colitis Toxic Megacolon
How To Prevent Pressure Ulcers Or Bed Sores
Pressure ulcers are a common problem in palliative care patients. Decreased mobility, increased time spent in bed, and altered nutrition make these patients prime targets for skin breakdown. Pressure ulcers are painful. As a caregiver, one of the most important things you can do to keep your patient comfortable is to prevent one from developing.
Pressure Injury Risk Assessment
The Norton pressure ulcer risk assessment scale was being used at KUH however, most ED nurses found it too long and time-consuming to use properly and consistently. Therefore, the scale was abridged to include minimal criteria for assessment of risk of pressure ulcer development . Posters showing these criteria were displayed prominently at the entrance to the ED alongside a digital screen showing a 45-second instructional video designed to educate and remind paramedics that when handing over patients to the triage nurses, they must communicate clearly if patients met the inclusion criteria and should be identified as at-risk. The triage nurse would then record this information in the patientâs electronic medical record , which would trigger fields and alarms prompting the nurse to undertake an initial skin assessment, ensure a turning and positioning system was in place, and ensure that prophylactic dressings were available.
Box 1.
Also Check: Can Foot Ulcers Be Cured
Classification Of Pressure Ulcers
Pressure Ulcers would be classified as grade I to IV according to The Pressure Ulcer Advisory Panel Consensus Development Conference 1989, and the National group for the study and counseling in Pressure Ulcers and Chronic Wound-Spain , 2003. We did not use the new pressure ulcer terminology and the updated stages provided by The National Pressure Ulcer Advisory Panel- NPUAP, given that all hospitals in our country follow the Ministry of Health Guidelines according to the primary pressure ulcers classification and also Pus are reported in this way.
This system, accepted until very recently, establishes four stages for pressure ulcers. The main objective of any classification system is to standardize the collection of information and provide a standard description of the severity of the ulcer for both clinical practice, evaluation, or research purposes.