How Do You Treat Diabetic Foot Ulcers
When a DFU is present, attempts to treat at home should not be made. Patients must seek medical attention to be sure that the ulcer or wound is not a venous ulcer, an arterial ulcer, a malignant melanoma, or another issue. Additionally, the risk of being too submissive in the treatment of a DFU without seeing a physician for care can result in the risk of compromising the extremity.
Once a physician has been consulted and diagnosis is confirmed, treatment will consist of three basic approaches: debriding the wound, keeping weight off the wound, and controlling the risk of infection.
Debridement of the wound involves the removal of necrotic tissue on the foot. Periwound callus must be removed as well. Once these two steps have been taken, the critical step of removing foreign bodies must be carried out. The debridement process needs to be ongoing until viable tissue is present. This will reduce infection risk and ease peri-wound pressure . Once debridement is complete, the ulcerated area should be thoroughly rinsed with an irrigation agent such as saline, followed by the application of a wound dressing. If an abscess is present, the ulcer will be incised and drained before the abscessed tissue is removed via debriding. If treatment is swift and accurate, amputation can be avoided. Antibiotics alone will not prevent morbidity and mortality.
- Staphylococcus aureus
- Bacteroides
- Peptostreptococcus
What Wounds And Ulcers Are Commonly Confused With Diabetic Foot Ulcers
There are several types of ulcers and wounds that can mimic a diabetic foot ulcer. Venous and arterial ulcers are both open sores that are often found on the lower extremities of the body, frequently the feet. Arterial ulcers are the resulting development from arterial damage from inadequate blood flow to the tissues.
Physicians must exercise high levels of attention to detail when assessing the difference between a diabetic foot ulcer and malignant melanoma. Malignant melanoma on the foot is frequently mistaken for a diabetic foot ulcer. There is a great need for biopsy in the early stages of foot ulcers. This is the only way that the rate of misdiagnosis can be reduced, and this erroneous diagnosis can be critical.
Tip #: Check Your Feet Daily
Touch and inspect the skin on your feet and lower legs each day to watch for any scrapes, bruises or swelling.
On the other hand, remove or rearrange household items that could cause you to trip or fall. Similarly, if you do frequently bump into furniture with the same part of the body, protect that part of the skin with a wrap or brace.
You May Like: Symptoms Of Having Ulcers In Your Stomach
How Can Diabetic Foot Ulcers Be Prevented
Looking after your feet can help prevent foot ulcers and avoid serious complications. Good foot care includes checking your feet every day, keeping them clean and dry, wearing proper footwear and trying to avoid doing things that could damage them.
Get a foot check at every healthcare visit and seek urgent medical advice if you notice a cut, ulcer or other injury on your foot.
Learn more about diabetes and foot care.
Preventing Diabetic Foot Infections
See related article on diabetic foot infections
If you have diabetes, you can develop sores or wounds on your feet. These sores are called ulcers. If a foot ulcer does not heal, it could get infected. However, if you watch your diabetes carefully and take good care of your feet, you can usually prevent infection. Here are some tips to help you avoid an infection.
Don’t Miss: How To Relieve A Stomach Ulcer
How To Promote The Healing Of Chronic Wounds And Diabetic Ulcers
Diabetes is the leading cause of foot amputation in the United States, which is why immediate treatment is essential with chronic wounds like diabetic ulcers. At the first sign of a chronic wound or diabetic ulcer, see your doctor as soon as possible. Diabetes causes healing impairments and its always better to seek professional help. The sooner your wound is treated, the lower your risk for complications. Wound Care Centers are the best place for chronic wound treatment, so talk to your doctor for recommendations as a proactive measure.
To promote the healing of chronic wounds and diabetic ulcers, your doctor will assess the wounds seriousness and create a treatment plan. Some of the treatment options include the following:
The best way to promote healing in chronic wounds like diabetic ulcers is to properly manage your diabetes. Byram Healthcare has a range of products to help you monitor your blood glucose levels with ease. If youre faced with healing a chronic wound, our wound care product selection guide has everything you need to support your doctors treatment plan.
Tell Us About The Skin
Our research, for the first time, uncovered a skin-to-brain signaling pathway. It showed that the wound itself could cause subsequent central nervous system and behavioral changes.
We, and others, have observed behavioral and cognitive changes in our patients who have chronic wounds. It is unknown if the wound causes these changes, or they are just associated findings. The idea we proposed is that when a patient gets a wound that heals right away, there is not much sustained signaling of stress to the brain. But a chronic wound keeps activating the sensory receptors for painful stimuli , sending a more continuous skin-to-brain relay. This continuous flare generates brain signals of stress that are translated into behavioral changes.
We carried out research in mice and found that skin wounds result in a relay to the brain. This relay leads to the activation of stress markers, alteration of inflammatory mediators and changes in behavior and cognition. Mice with wounds showed more signs of despair and impaired memory than those with no wounds.
We often see similar behavior in patients with chronic wounds that need daily wound care. Some seem unable to attend to their wounds despite the serious risk of losing their foot to amputation. We also observe depression and cognitive disability reflected in the perception of inability to take care of their wounds. Some even seem to be disassociated from the reality of the serious nature of this problem.
Also Check: Ulcerative Colitis Medication Not Working
Causes Of Diabetic Foot Ulcers
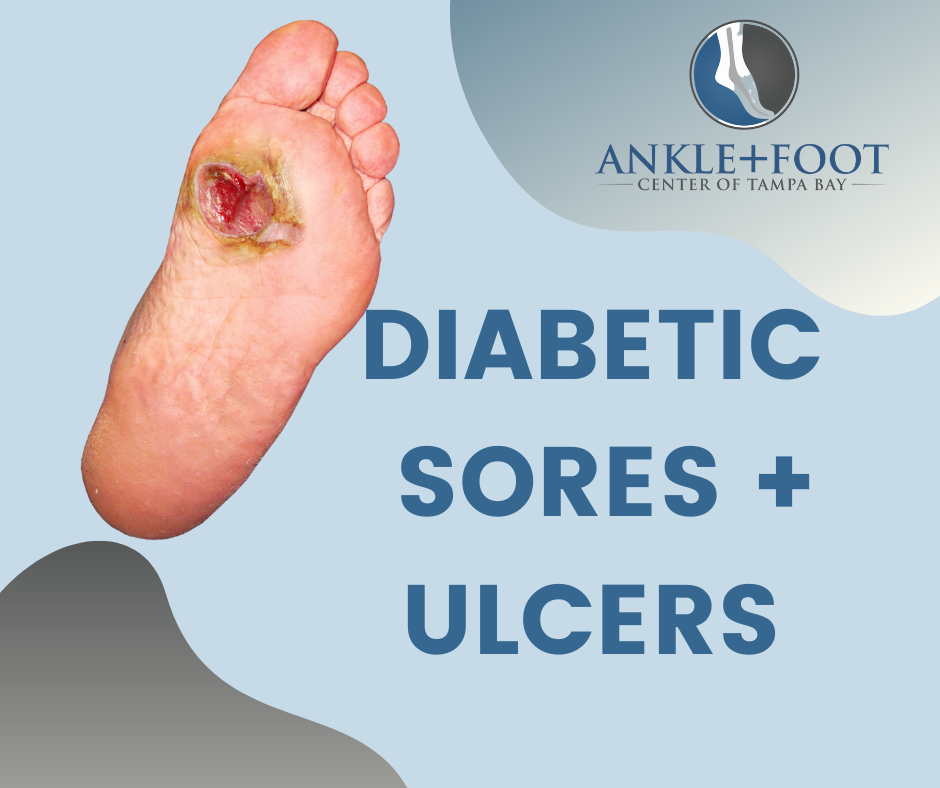
An ulcer is an open sore or wound on the skin. Ulcers on the feet are particularly common in those who have diabetes. Complications from the disease such as poor circulation and loss of feeling in the feet due to diabetes-related nerve damage make it more likely for a wound to develop, and also harder to heal.
People with diabetes who use insulin, have diabetes-related kidney, eye or heart disease, or who are overweight, use alcohol or tobacco have an even higher risk of developing foot ulcers.
Prevention And Management Of Diabetes Complications
Diabetes is a chronic metabolic disease, which affects the vascular system extensively throughout the body. The metabolic complications of DM should be treated concomitantly with no bias in treating one metabolic complication over others. The metabolic diseases secondary to DM should be controlled and the target values should be kept below the recommended standard. As a result, the preventive measures should be taken in order to control the neuropathy and PAD, which are the main cause of DFU.
The preventive measures and management of diabetic complications consists of the following:
-
Life style modification
-
Smoking cessation.
Read Also: Stage 3 Pressure Ulcer Treatment
History Of Foot Ulceration Or Amputation
Previous ulceration or amputation are recognised as the most significant risk factors for developing further ulceration.6This probably represents the underlying limb pathology, and may also be related to gait changes that result from an amputation.7,8.
A person with diabetes and a history of foot ulceration or amputation must be considered at ongoing high risk for developing further ulceration and be referred to a podiatry service for monitoring and management. There is evidence to support reduced re-ulceration and amputation rates in people with diabetes who access regular podiatry care.9,10,11
What Causes Foot And Toe Ulcers How Do You Get An Ulcer
There are many possible causes. The most common include:
- Neuropathy from diabetes.
- Peripheral arterial disease.
- Deformed toes.
- Walking in an odd way where you put too much pressure on one part of your foot or toe.
- Friction. Your foot or toe may rub against the toebox of your shoe.
Although they dont cause ulcers, foot and toe ulcers are often found alongside toe deformities such as hammertoe, mallet toe and clawtoe.
Don’t Miss: Ulcerative Colitis Diet Plan During Flare Up
Do You Have To Be Diabetic To Have Ulcers
Ulcers can happen to almost anyone. Since there are a variety of different ulcers, many individuals can find themselves needing treatment at some point in their life. Diabetic ulcers, however, are specific to those who have diabetes.
There are two types of diabetes: diabetes 1 and diabetes 2. Type 1 diabetes is diagnosed when a person is unable to produce insulin. Because the body cannot produce any insulin at all, those diagnosed with this type of diabetes must rely on insulin injections to stay alive. Type 2 diabetes occurs when the individual produces but cannot helpfully respond to insulin.
Those who are diagnosed with either type 1 or 2 diabetes are at risk for diabetic ulcers. Because diabetes can reduce nerve functioning due to its neuropathy, nerves that are typically used to send pain sensation to the brain from the feet cannot function properly. Not only does this mean that a foot ulcer may go unnoticed, but in conjunction with reduced blood flow, diabetic ulcers are less likely to heal without proper treatment.
Treatment For Vascular Ulcers

Its important to note that not all skin ulcers are caused by diabetes, and that even people who dont have diabetes can suffer from chronic wounds. Even people without diabetes can be susceptible to vascular ulcers. Vascular ulcers are caused by problems with the vascular system .
These types of ulcers can happen to people who suffer from veins or arteries that dont function properly, causing blood flow in the legs to be limited. This can lead to an increased risk of wounds that may not heal normally and can become infected.
The Wound Care Center at Harrington also provides full service care for these types of wounds, including on-site X-rays, MRI and lab work.
To make an appointment at the Harrington Wound Care Center, call 248-8105. You can also learn more on our website here.
Read Also: Foods To Avoid With Peptic Ulcer
Clinical Pathways And Assessment Forms For Diabetic Foot
Our Testimonials
-
I don’t have time to assess the quality of the many websites out there I would want to refer people to. Health Navigator solves this in one easy step. It is my “go to place” to send people for great information and self-management support.
Dr David Codyre
Primary care psychiatrist
-
Health Navigator provides the whole package of information on a topic. There is a high level of health literacy for the website itself and the information provided.
Christine Andrews
Quality Improvement Manager, Marlborough PHO
-
I was really impressed because health is covered in its entirety. Its a very useful site for clinicians or anyone interested in gaining knowledge around the current status of indigenous wellbeing here in Aotearoa.
-
I always recommend Health Navigator resources to my patients. It provides high quality, reliable, NZ relevant information in a clearly organized and easy to understand way. This means people can quickly get the key information or dig deeper when needed.
Dr Rebecca Grainger
Rheumatologist & researcher, University of Otago, Wellington
-
Health Navigator is such a valuable resource. Its useful for consumers, health professionals and health students as it covers a diverse range of topics, the explanations are easy to understand, and most importantly is credible and NZ focussed.
Dr Michelle Honey
How Does This Insight About The Skin
As physicians who treat chronic wounds, we generally don’t assess the mental status of our patients. We often just focus on healing the wound. We can be more aware of the patients mental health and recommend intervention if they show depression or cognitive disability.
Ideally, we should have mental health specialists in our clinics to address the mental health needs of patients. Patients need additional education on how their mental health can affect their healing, and conversely, how the non-healing wound may be affecting their mental health. These interventions could help the overall healing process and result in better outcomes for our patients with chronic wounds.
To learn more about Isseroffs study on skin-brain connection, read her article in Brain, Behavior, and Immunity- Health.
Read Also: What Is The First Sign Of Stomach Ulcer
Tip #: Wear Shoes That Fit Properly
“Don’t just go out and buy random shoes,” she warns. Wearing shoes that are ill-fitting or put a lot of pressure on your foot may result in a pressure ulcer. If you don’t know your correct shoe size, have a professional assist you.
You should also steer clear of shoes with pointed or open toes, such as high heels, flip-flops or sandals. Also, wear shoes made of breathable fabrics, like canvas, leather or suede.
- Related post:Foot Problems? Swap Your Shoes
Who Can Get A Diabetic Foot Ulcer
Anyone who has diabetes can develop a foot ulcer. Native Americans, African Americans, Hispanics and older men are more likely to develop ulcers. People who use insulin are at a higher risk of developing a foot ulcer, as are patients with diabetes-related kidney, eye, and heart disease. Being overweight and using alcohol and tobacco also play a role in the development of foot ulcers.
Read Also: Bone Broth And Ulcerative Colitis
How Are Foot And Toe Ulcers Treated
The goal of treating a foot or toe ulcer is to relieve pain and heal your wound. Your treatment plan will be individualized based on what medical condition is causing your ulcers. If you cant correct the cause of your ulcer, its likely to come back after treatment.
There are both surgical and nonsurgical treatments for foot and toe ulcers. For simple, early stage foot and toe ulcers, nonsurgical treatments may work. Ulcers that are more advanced, especially ones that are infected, may require surgery.
Diabetic Ulcers: Prevention And Treatment Strategies
Foot ulcers are a huge problem for people with diabetes, neuropathy, poor circulation, and other related conditions.
How huge? Consider that around 100,000 Americans must get part of a foot or leg amputated each year as a direct result of diabetic foot wounds that never properly healed. And the five-year survival rate after these amputations hovers around just 50 percent.
When you consider whats at stake, its clear that anybody with diabetes should make the following commitments to themselves for their future health and happiness:
- Do everything they can to stop serious ulcers from developing in the first placewhich includes seeking a foot and ankle specialist at least once a year for a comprehensive diabetic foot checkup.
- If an ulcer does form, seek out professional care from a diabetic wound care expert as soon as possible.
Fortunately, you dont have to look far to get the quality comprehensive care you deserve. Waco Foot & Ankle can help you manage all aspects of diabetic foot and wound care, helping you protect and preserve your feet for years to come.
How to Prevent Diabetic Ulcers from Forming
Prevention is always preferred over treatment.
Fortunately, most diabetic wounds can be prevented. And furthermore, the most serious complications from diabetic wounds can almost always be prevented if you follow your diabetic foot care routine faithfully and seek intervention as early as possible when you spot issues.
What to Do If You Spot a Potential Diabetic Foot Ulcer
Recommended Reading: How To Get Rid Of Tongue Ulcers
Diabetic Foot Ulcer Prevention
Prevention of DFUs often goes hand in hand with intervention. The ultimate goal is to allow the ulcer to heal properly and avoid future complications such as amputation.
Glycemic control. Individuals with diabetes must monitor their blood glucose closely to prevent hypoglycemic or hyperglycemic episodes. These events can have long-term consequences, including a DFU.
The human body requires balanced blood glucose to heal appropriately. Recent literature suggests that a hemoglobin A1c value between 7.0% and 8.0% is optimal for facilitation of ulcer healing.4 However, this is dependent on the individuals glycemic control at baseline. Additionally, an individual who has a DFU, an HbA1C of over 8.0%, and a fasting blood glucose greater than 126 mg/dL is more likely to have a lower extremity amputation.5
Other studies also indicate that strict glycemic control after a DFU has formed can lead to better healing rates. This was true for DFUs that did not respond to conventional care.6 Better glycemic control leads to improved healing and prevention.
Proper footwear. As discussed earlier, individuals with diabetes may not be able to feel the touch or pain of a sharp object or pressure point on their foot. Therefore, proper footwear is essential to preventing ulceration initially. Proper footwear includes:
- Sufficient coverage of the foot
- Appropriate sizing of footwear
- Walker
- Orthotic
- Total contact casting
What To Expect At Home

Diabetes can damage the nerves and blood vessels in your feet. This damage can cause numbness and reduce feeling in your feet. As a result, your feet are more likely to get injured and may not heal well if they are injured. If you get a blister, you may not notice and it may get worse.
If you have developed an ulcer, follow your health care provider’s instructions on how to treat the ulcer. Also follow instructions on how to take care of your feet to prevent ulcers in the future. Use the information below as a reminder.
You May Like: Ulcerative Colitis Rectal Pain Relief