Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Ulcerative Colitis Symptoms And Causes
Ulcerative colitis is thought to develop when a person at genetic risk is exposed to certain environmental stressors.
These environmental stressors either change the ratio of gut bacteria or alter the way the immune system responds to bacteria .
As a result, the immune system attacks the intestinal lining causing inflammation and other symptoms, including:
Also Check: Artificial Sweeteners And Ulcerative Colitis
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, thesymptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
How A Professional Can Help

Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
You May Like: Foods That Cure Ulcerative Colitis
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohn’s disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Vitamin And Mineral Supplementation
Nutritional supplements are great for patients with inflammatory bowel disease who may need a bit of extra help preventing a nutritional deficiency.
Your healthcare providers may also recommend a vitamin and/or mineral supplementation plan if your tests show you already have a nutritional deficiency.
You may be able to get all your necessary vitamins and minerals from eating a well-balanced, nutrient-rich diet. But flares, severe symptoms, surgeries, and other complications may make it difficult for some patients with Crohns disease or ulcerative colitis to get enough nutrients from food alone.
Check with your doctor or other healthcare providers before taking any supplements, including over-the-counter medications, herbs, and other complementary therapies.
-
Some supplements can cause gastrointestinal symptoms, including nausea and diarrhea.
-
Check the labels on your supplements for lactose, artificial colors, sugar alcohols, or preservatives, all which can aggravate your IBD, especially when you are in a flare.
-
Most supplements should not be taken on an empty stomach.
Video Length00:02:00
Vitamin and Mineral Supplementation in IBD Often times, when you have Crohn’s disease or ulcerative colitis, you may need to take vitamins or minerals to prevent or make up for a nutritional deficiency. Watch and listen this video to learn more about common vitamin and mineral supplements for IBD patients.
Also Check: How To Treat Skin Ulcer On Leg
What Is Ulcerative Colitis
Ulcerative colitis is a chronic type of inflammatory bowel disease , like Crohns disease and microscopic colitis that affects the colon .
Recent studies estimate that IBD affects 2 million people worldwide .
Ulcerative colitis causes inflammation and sores in the inner lining of the colon. Inflammation often begins in the rectum, but it can spread throughout the large intestine.
Summary: Ulcerative colitis is a type of inflammatory bowel disease that causes inflammation and sores in the colon.
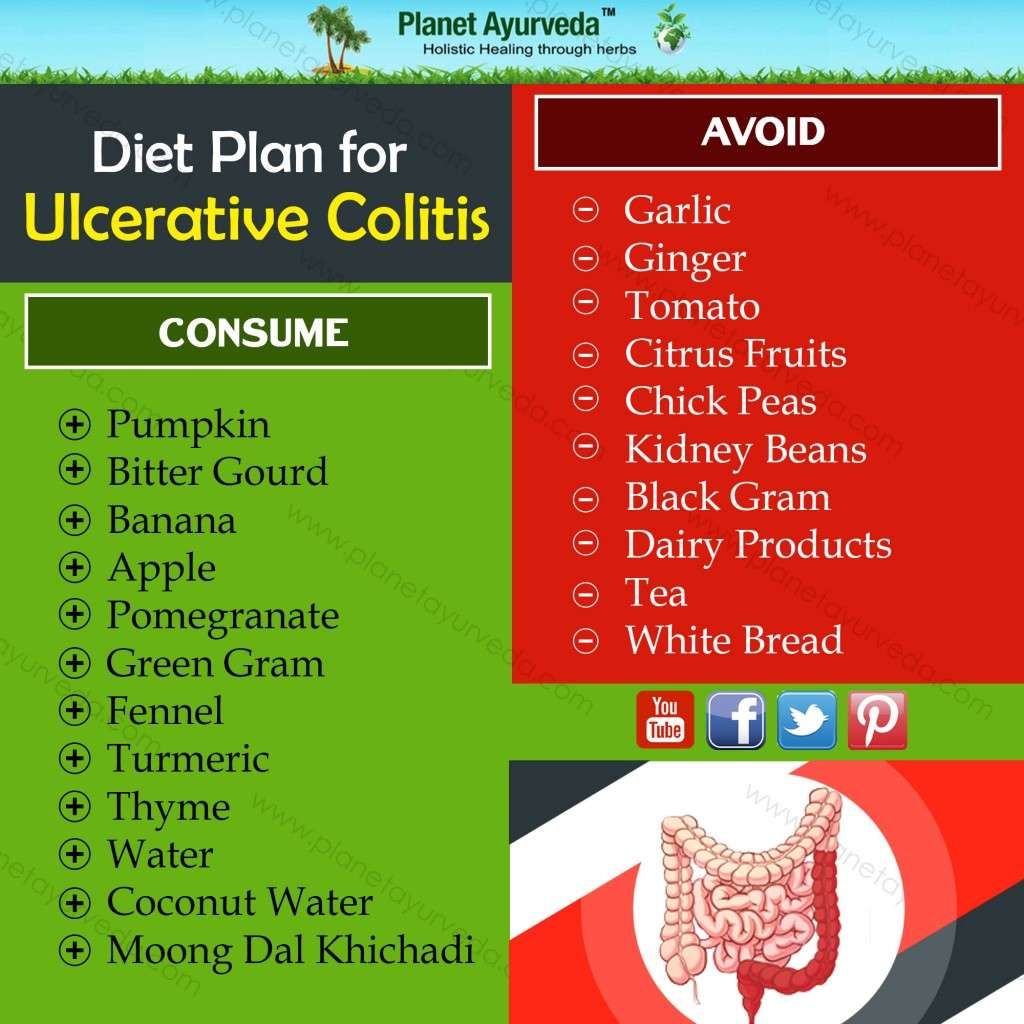
What Foods Should I Not Eat When I Am Having An Ulcerative Colitis Flare
Certain foods can exacerbate or aggravate an UC flare and should be avoided. They are more likely to trigger cramping, bloating, and/or diarrhea and are also not recommended in people diagnosed with a stricture, which is a narrowing of the intestine caused by inflammation or scar tissue, or in those who have had recent surgery. Examples include:
- Foods high in insoluble fiber that are hard to digest, such as seeds, raw green vegetables , whole nuts, whole grains, or fruits with a skin
- Lactose, which is milk sugar found in dairy products, milk, cream, cream cheese, and soft cheeses
- Non-absorbable sugars such as sorbitol, mannitol, and other sugar alcohols that are typically found in sugar-free gum, candy, ice cream, and certain types of fruits and juices such as pear, peach, and prune juice
- Sugary foods such as candy, pastries, and juices
- High-fat foods such as butter or margarine, coconut oil, or fatty, fried, or greasy food
- Spicy foods
- Alcohol such as beer, wine, or spirits
- Caffeinated drinks such as coffee or energy drinks
- Soda.
Don’t Miss: Ulcers In Small Bowel Crohn’s
Ulcerative Colitis Crohns Disease Or Something Else
The colon, also known as the large intestine, has three parts or section: ascending colon , transverse , descending colon , and the sigmoid colon just before the rectum.
Ulcerative colitis symptoms in each person will be different depending on where inflammation occurs and how bad it is. The most common symptoms include:
There are common complications that tend to come with UC, even though they are not actually a direct result of this chronic health condition. Fever, fatigue, and anemia are perhaps the most common additional symptoms. Additionally, inflammation beyond the colon often shows up as skin sores, skin rashes, mouth sores, joint pain, red and painful eyes, and sometimes even liver disease.
While both are referred to as inflammatory bowel disease or IBD, and Ulcerative colitis is related to Crohns disease, they are still different. Crohns disease, unlike ulcerative colitis, is not limited to the colon and is a chronic inflammatory disease of the intestines or the entire GI tract. Crohns often affects the small intestine and colon although occasionally it, too, is limited to the colon.
Foods To Eat With Ulcerative Colitis
Understanding inflammatory bowel diseases like ulcerative colitis can be difficult, especially knowing what foods to eat. An ulcerative colitis flare can be exacerbated when eating inflammatory foods. Likewise, one can easily become nutrient deficient if there is a lack of variety in the diet. Here we look into some recommended foods to eat when you have an ulcerative colitis flare.
Your nutrition affects your overall health and well-being. When you do not get the proper nutrients, you can experience ulcerative colitis complications like weight loss, malnutrition, and nutritional deficiencies. Before we dive into the foods that you should eat, here are a few tips that can help improve your health and reduce the frequency of flare ups.
You May Like: Best Ulcerative Colitis Diet Book
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
An Ulcerative Colitis Diet: Summarizing The Evidence
Despite many reports online that certain diets or supplements can cure ulcerative colitis, the only known cure is total removal of the colon and rectum.
Those with digestive symptoms during remission may find relief from a low FODMAP diet to identify trigger foods.
A semi-vegetarian diet has also shown promise in maintaining remission in Crohns disease and may be helpful for ulcerative colitis, but we cannot make firm conclusions.
Even without following elimination diets, certain patterns have been shown to reduce symptoms:
- A diet that is rich in fruits and vegetables provides fiber and antioxidants, which are linked to lower disease risk. Reducing intake of high-fiber fruits and vegetables may increase comfort during flares.
- Limiting dietary fat, especially fatty meats, may be beneficial.
- Certain probiotics are helpful in bringing about and maintaining remission. Ask your doctor for a recommendation.
- A few herbal supplements show promise but lack sufficient scientific evidence to support their use.
- Avoid foods that irritate the gut during flares, including fatty foods, caffeine and alcohol.
A registered dietitian can help you identify foods that trigger your symptoms and design a well-balanced meal plan.
If you would like more information on how to eat for Ulcerative Colitis, which involves what we call a low FODMAP diet, tap the button below to download our Eat This, Not That list as well as additional resources for Ulcerative Colitis
SEND ME THE LIST
Recommended Reading: How To Cure Tongue Ulcer
Ulcerative Colitis Diets You Might Try
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Can Food Cause Crohn’s Or Colitis
We dont know what causes Crohns and Colitis but we do know that a combination of the following factors are likely to play a part:
- Genetics
- A problem with the immune system, where the body attacks its own cells
- Changes in the bacteria in the gut.
These, together with environmental factors, like food and stress, may trigger the conditions.There isnt any clear evidence that specific foods cause Crohns or Colitis. Some researchers think a diet low in fruit and vegetables may increase the risk of Crohns and a low intake of vegetables may increase the risk of Colitis for some people. Theres also some evidence that eating a lot of meat or table sugar, called sucrose, may increase the risk of Crohns and Colitis. But there isnt enough evidence yet to say for certain whether food affects the risk.
Recommended Reading: What Medicine Is Good For Ulcers
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
Eating During Remission From Uc
During remissionthat blissful time when your insides arent rioting against youyou may wonder if you can relax a little bit more about the foods you eat. In general, move slowly when adding new foods to your diet during remission. In fact, its best to do it one at a time so you can monitor any reaction. Otherwise, aim to hit the main points of a Mediterranean diet to get the nutrients you need. Your doctor or R.D. can offer more advice too. In the meantime:
-
Prioritize whole grains, non-cruciferous vegetables and low-fiber fruits, and healthy fats
-
Incorporate poultry, fish, beans, and eggs weekly
-
Add moderate portions of dairy if you can tolerate lactose
-
Limit your consumption of red meat
-
Limit processed foods
Recommended Reading: What Foods Can I Eat If I Have An Ulcer
The Best Foods To Eat And Avoid For Inflammatory Bowel Disease
Inflammatory bowel disease is a treatable, yet chronic and lifelong condition. IBD is a broad term that refers to the inflammation of the gastrointestinal tract and includes specific conditions such as ulcerative colitis and Crohns disease.
No plan has been proven to prevent or control IBD. But managing your diet can help manage your disease during flares and periods of remission. Be sure to talk to your physician or a registered dietitian about your nutrition needs and managing IBD.
Here are diet recommendations for managing IBD flares and remissions from UH Outpatient Nutrition Services.
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
Watch out for items that can be troublemakers if you have UC, including:
- Alcohol
You May Like: What To Take For Stomach Ulcer Pain
Fight Anemia And Fatigue With Iron
Flares wear you out. One reason can be anemia, when your body doesn’t have enough healthy red blood cells. If you have long-term, low-level bleeding from your colonâs lining or bloody diarrhea, you may get iron deficiency anemia and need iron supplements. Food sources include lean meats, seafood, spinach, raisins, and fortified breakfast cereals. Egg yolks and artichokes are other options that may be easier on your stomach.
3
Tips For Meal Prepping

Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
Recommended Reading: How To Check A Horse For Ulcers
The Worst Foods For Those With Ulcerative Colitis
Ulcerative colitis is an inflammatory chronic disease of the colon and rectum where ulcers develop inside the lining of the large intestine. It is an inflammatory bowel disease along with Crohns Disease which causes a multitude of painful and unpleasant symptoms. Since dietary habits can contribute to ulcerative colitis symptoms, lets look at the worst foods for those with ulcerative colitis.