How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
What Are The Symptoms Of Crohns Disease
The symptoms of Crohns disease vary, depending on which part or parts of the gastrointestinal tract is/are affected. Common symptoms include:
- Abdominal pain that comes and goes
- Blood in your stool
- Unintended weight loss
Other less common symptoms may include fever, joint pain, eye problems, skin problems, and feeling tired . The symptoms of Crohns disease may be mild or severe. Symptoms may also come and go. They can start suddenly or gradually.
Complications Of Ulcerative Colitis
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
“It’s easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,” says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
You May Like: Foods That Prevent Stomach Ulcers
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Proctocolectomy With Brooke Ileostomy
Description of procedure
Indications
Most patients are suitable candidates for this operation irrespective of age. The choice of this operation is often appropriate for patients who wish to avoid the problems associated with ileoanal pouch procedure or those who are not suitable candidates for a resortative procedure, especially in elderly patients and those with poor sphincter function.
Contraindications
IPAA is now the surgical procedure of choice in most patients with UC .
Contraindications
Operative factors
The ileal pouch is constructed using one of the several pouch designs, which include the J-pouch, S-pouch and W-pouch. The ultimate choice of pouch design is largely the surgeon’s preference, studies to date suggesting that J and W produce similar results. The S pouch is considered an inferior design, especially when there is a long exit spout, as this can cause obstructive defecation problems which at times require intubation of the pouch to empty it . The J-pouch design is the most commonly used in part due to the ease of construction.
Complications
Bowel obstruction is common following all types of surgery for UC. The annual risk for patients following IAPP is 1 in 25, 1 in 49 for a Kock pouch, 1 in 66 for a proctocolectomy and Brooke ileostomy, and 1 in 71 for colectomy and ileorectal .
Outcome
Recommended Reading: How Can I Tell If I Have An Ulcer
What Really Constitutes Laparoscopic Ipaa Variability Within The Same Definition
A variety of techniques is currently referred to as laparoscopic IPAA. In some cases, the dissection of the rectum and the transection at the anorectal ring are performed using standard laparoscopic techniques. The specimen is then removed through either a small lower midline incision, a Pfannenstiel incision, or through the site where a subsequent diverting loop ileostomy will be created. Some surgeons perform a completely laparoscopic rectal dissection, but prefer to transect the distal rectum through the extraction site using a conventional linear stapler. In other cases, the rectal dissection is not performed laparoscopically, rather it is performed under direct vision using the future extraction site and following complete laparoscopic mobilization of the abdominal colon.
Also Check: Diabetic Foot Ulcer Treatment Guidelines
What Causes Ulcerative Colitis In A Child
Healthcare providers don’t know what causes this condition. It may be triggered by a virus or bacteria. This interacts with your childs immune system and causes an inflammatory reaction in the intestinal wall.
Children with ulcerative colitis often have problems with their immune system. But healthcare providers don’t know if these issues are a cause or a result of the disease.
Theres no cure for this condition, except to take out your childs colon with surgery. However, the symptoms can be managed medically.
Recommended Reading: Why Do We Get Mouth Ulcers
Whats Recovery Like From An Ulcerative Colitis Colectomy
You may notice immediate improvements in your UC symptoms following a colectomy.
But as with any major surgery, youll need to take time off to recover and reduce the risk of infections and bleeding. Youll also have pain in your abdomen due to the incisions.
A doctor may recommend a liquid or soft food diet for a few days after your procedure. They may also advise against exercising for at least 6 weeks. You may consider taking a few weeks off work or opt for a work-from-home option, if available.
It may take up to 1 year to fully recover from a proctocolectomy. You may experience multiple bowel movements per day for several months.
Recommended Reading: How To Check A Horse For Ulcers
Home Remedies For Ulcerative Colitis
A number of lifestyle measures can help control ulcerative colitis symptoms and reduce the stress of living with this chronic condition.
Check with your doctor before trying any of the following approaches to managing your disease.
Eat small, frequent meals. Compared with eating three large meals each day, this lowers the likelihood of abdominal discomfort after eating.
Stay hydrated. CurcuminPharmaceuticsFish oilFoodsMind-body practices
Also Check: Signs Of Ulcers In Colon
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Elective Surgical Management Of Ulcerative Colitis
Surgical options for elective management of ulcerative colitis include total proctocolectomy with creation of an end ileostomy, total proctocolectomy with continent ileostomy, total proctocolectomy with IPAA, and total abdominal colectomy with ileorectal anastomosis. Among these, a creation of an IPAA is currently considered the preferred standard of care. Patients who are not suitable candidates for IPAA can be treated with laparoscopic total proctocolectomy and end ileostomy. On the other hand, laparoscopic surgery in the creation of an ileorectal anastomosis following total abdominal colectomy is technically feasible, but is rarely indicated. Similarly, total proctocolectomy and creation of a continent ileostomy is generally performed on patients who had previous surgical procedures for ulcerative colitis and is therefore typically performed using open technique. Ileorectal anastomosis and continent ileostomy will therefore not be further discussed in this review.
Read Also: What Are The Best Foods To Eat With An Ulcer
How Can I Minimise My Risk Of Getting Bowel Cancer
Its impossible to change some of the things which put you at an increased risk of bowel cancer , but there are some lifestyle factors which are thought to place anyone at a greater risk. Making some healthy lifestyle changes can help to mitigate against these risks. They include:
- Exercising regularly
How Long Will It Take To Recover
Recovery is a gradual process after UC surgery. You will stay in the hospital until your bowel function returns. This can take up to a week. During this time, you will not be able to eat solid foods. Its common to have IV nutrition for a short time after surgery. You will transition to clear liquids, soft foods, and finally solid foods as your intestines heal.
If you have an ostomy, you will meet with an ostomy nurse to learn how to care for your stoma. The ostomy is temporary if you had a sphincter-saving surgery. Full recovery can take 6 to 12 weeks. At that time, your doctor will decide if the ostomy is ready for closure.
You May Like: Does Aloe Vera Help Ulcerative Colitis
Can You Cure Ulcerative Colitis With Surgery
Surgery isnt usually done for mild colitis. The only cure for ulcerative colitis is surgery to remove the colon and the lining of the rectum. After the most common type of surgery, you will still be able to have bowel movements. After the less common type of surgery, you will wear an ostomy bag to remove body waste.
What is the best antibiotic for colitis?
Iron. Colitis may cause bleeding from the colon. If there is enough blood loss,it can cause anemia.
What are the early signs and symptoms of ulcerative colitis?
Fever
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
Recommended Reading: How To Treat A Diabetic Foot Ulcer On The Sole
Open Vs Laparoscopic Colectomy
The terms open and laparoscopic refer to how the colectomy surgery is performed. During an open colectomy, a surgeon makes a large incision in the abdomen to remove the colon tissue. In laparoscopic surgery, the surgeon makes very small cuts and uses flexible tools and cameras to see inside the body and remove the intestine.
Ask About Adding Another Medication
Sometimes one medication isnt enough to tackle severe UC symptoms. Your doctor might give you a second medication to help you manage your condition. For example, you might need to take both a biologic and an immunosuppressant drug.
Taking more than one medication can increase the odds of treatment success. It can also increase your chances of experiencing side effects. The doctor will help you balance the benefits and risks of the medications you take.
Also Check: Suggested Diet For Ulcerative Colitis
Does A Colectomy Cure Ulcerative Colitis
- One possible treatment for ulcerative colitis is a colectomy, in which all or part of the colon is removed.
- A colectomy will likely help relieve all colon-related symptoms.
- After a colectomy, people with UC may still have other health problems related to other organs, or they may experience lifestyle changes caused by the surgery.
Ulcerative colitis is a form of inflammatory bowel disease in which the immune system attacks the large intestine . UC causes inflammation and ulcers to form. If the large intestine becomes too damaged or causes severe health problems, your doctor may remove all or part of the colon and rectum in a procedure known as a colectomy, colon resection, or large bowel resection.
There are several types of colectomy procedures. For most people with UC, removing the full large intestine can resolve the majority of their symptoms. Moreover, most people who have a colectomy are able to resume their regular activities and hobbies. Still, undergoing the procedure may also require some lifestyle changes, which can take some getting used to. Understanding the options available and their potential impacts will help you engage in an informed conversation with your health care provider.
Your Uc Meds Stop Working
The drugs available to treat UC can be very effective at managing symptoms and preventing disease flares. However, for some people with UC, they can become less and less potent over time. Your medication is likely no longer helping if your UC flares and there are symptoms, including diarrhea and rectal bleeding, says Elena A. Ivanina, D.O., director of neurogastroenterology and motility at Lenox Hill Hospital in New York City.
Other signs to look for include abdominal pain, an uptick in the frequency of your trips to the toilet, and a return of the symptoms that you experienced before you started taking the medication, which likely included fatigue, fever, and bloody stools. For the most part, its a gradual process where patients start to notice worsening symptoms, explains Dr. Paluvoi.
Talk to your doctor if you notice such changes despite taking your Rx meds as prescribed. In addition to reviewing your symptoms, your doctor will run blood and stool tests to measure inflammation, an indicator that your medication has become less effective and disease activity is on the rise, says Dr. Ivanina.
Patients may consider different medications, unless their disease is severe and there is not enough time to wait for drugs to work, Dr. Ivanina elaborates. In such cases, it may be time to consider surgery.
You May Like: Ozanimod Ulcerative Colitis Phase 2
When You’re In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Can Ulcerative Colitis Be Cured With Surgery

Ulcerative colitis is a chronic inflammatory condition of the colon characterized by frequent bloody diarrhea throughout the day. Medicines can only reduce the intensity of its symptoms and surgery is the only option to cure it.
About 23%-45% of people with ulcerative colitis end up having surgery.
Surgery is needed in the following instances:
- Medicines fail to provide adequate relief of symptoms
- The patient is heavily dependent on steroids for ulcerative colitis
- Steroid therapy becomes ineffective
- There are intolerable side effects of medications
- The disease comes with a sudden onset and severe symptoms
- The affected colon tears or bleeds
- The growth of the child gets retarded
- Abnormal growths develop in the colon
Patients may choose surgery over medicines when
- they want to improve their quality of life,
- they want a permanent cure, or
- they want to reduce their risk of colon cancer .
Read Also: High Fiber Diet For Ulcerative Colitis
What Is Ulcerative Colitis Surgery
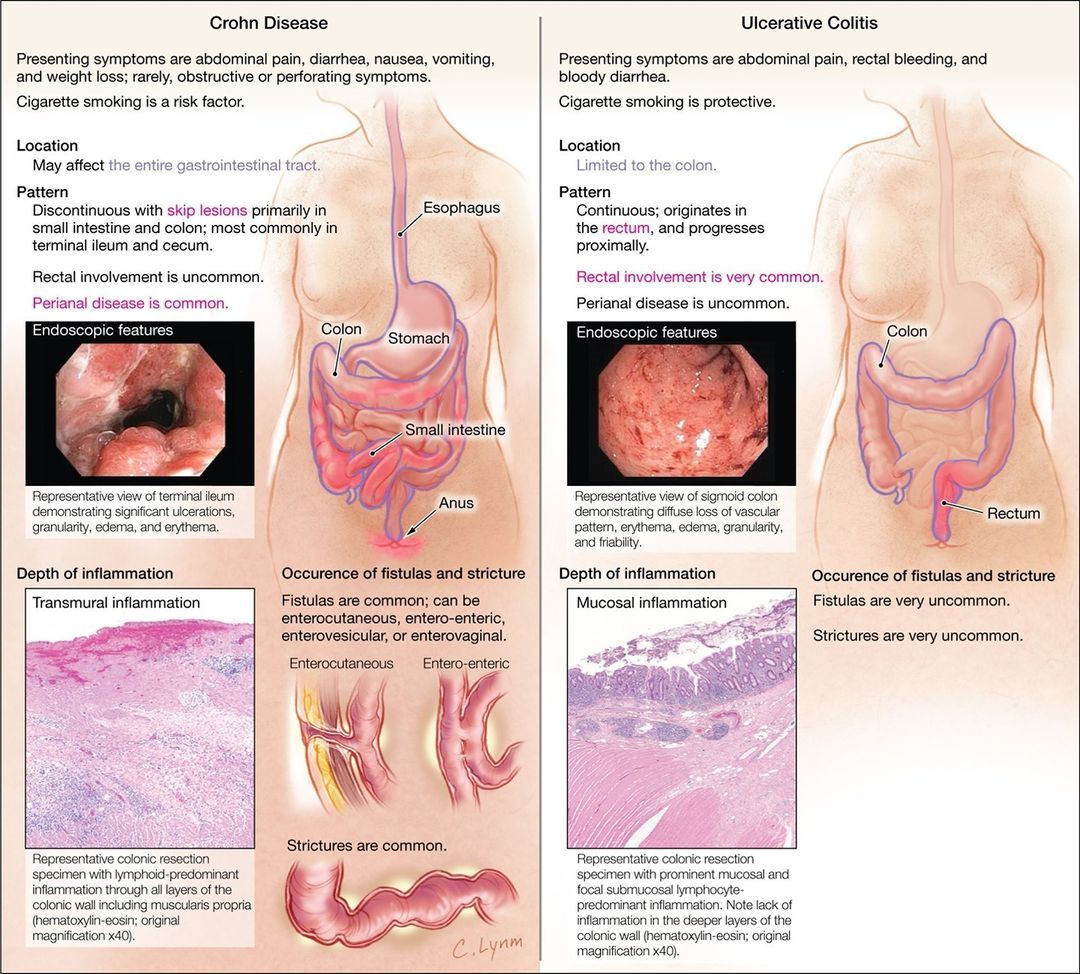
Ulcerative colitisor UCis a form of inflammatory bowel disease . The other type of IBD is Crohns disease. While Crohns can affect any part of the digestive tract, UC only occurs in the colon and rectum. As a result, surgery is a curative ulcerative colitis treatment.
There are four ulcerative colitis surgery options:
Each procedure has advantages and disadvantages. Talk with your doctor to find the option that best suits you.
Quality Of Life And Satisfaction With Colectomy
The majority of respondents reported that they were somewhat satisfied, satisfied, or very satisfied with colectomy. Most also reported an improvement in their quality of life post-surgery, with 46 % stating that their current quality of life was very improved.
The results of the various survey tools applied are shown in Table . The median IBDQ score was 172 , with clinical remission generally scoring above 170. The mean EQ-5D index score was 0.79 and the mean EQ-5D VAS score was 77.0 .
Recommended Reading: Over The Counter Medication For Ulcerative Colitis
Don’t Miss: What Foods To Avoid With Peptic Ulcer
Ulcerative Colitis Surgery Risks Complications
If you have any of these symptoms, get medical help right away:
- Infection or pouch inflammation . Signs: Diarrhea, frequent bowel movements, stomach cramps and pain, fever, joint pain. Treatment: Antibiotics.
- Blockage or bowel obstruction. Signs: Cramping, nausea, vomiting. Treatment: IV fluids and fasting, sometimes surgery.
- Pouch failure. Signs: Fever, swelling, pain. Treatment: Surgery and permanent ileostomy.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
You May Like: Peptic Ulcer Vs Gastric Ulcer