What Are The Complications Of Ulcerative Colitis Surgeries
Complications from ileoanal anastomosis may include:
- More frequent and more watery bowel movements
- Inflammation of the pouch
- Blockage of the intestine from internal scar tissue, called adhesions, caused by surgery
- Pouch failure, which happens within 5 years in about four out of every 100 patients with IPAA
If your pouch fails, youâll need a permanent ileostomy.
A hemicolectomy has some of the same risks as other surgeries. Your doctor will give you anesthesia to put you to sleep. Itâs safe for most people, but you could have a reaction that makes you feel sick for a few days. Itâs rare, but some people may feel confused for a week or so.
You could also get blood clots in your legs or lungs. To lessen the chances of this, a doctor or nurse will get you to walk around every hour or so in your hospital room.
Other possible problems include:
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
What Is Surgery For Ulcerative Colitis
Surgery for ulcerative colitis means removing the large intestine, or colon . After the large intestine is gone, there needs to be another way for stool to leave the body. The two most common ways of achieving this are either by placing an ileostomy or creating a j-pouch.
In an ileostomy, a part of the small intestine is brought through the abdomen. This is called a stoma. Stool leaves the small intestine through the stoma and collects in an appliance . The ileostomy appliance is emptied into the toilet several times a day.
In an IPAA, or a j-pouch, the end of the small intestine is attached to the rectum. This is usually achieved through a series of two or three surgeries, although some surgeons will do it in a single operation. When done in more than one surgery, the first surgery is always a colectomy with placement of a temporary ileostomy.
These surgeries can be done through an open incision, or, as is more often the case now, laparoscopically . Ideally, the surgery is scheduled but is sometimes an emergency operation.
Read Also: Does Ulcerative Colitis Cause Acne
In Ibd Patients Discussion Of Surgery Provides Valuable Education
We were unable to process your request. Please try again later. If you continue to have this issue please contact .Amy L. Lightner
In inflammatory bowel disease, as in most areas of medicine, surgery is reserved as a later option for cases that are unresponsive to less invasive treatments. However, for many patients, the conversation about surgery is best initiated earlier in their management instead of as a last resort.
When these patients get admitted with a severe flare, surgeons should be consulted sooner rather than later,Amy L. Lightner, MD, colon and rectal surgeon at the Mayo Clinic, said, referring specifically to ulcerative colitis . Even if the patient doesnt need surgery at admission, and they improve and respond to medical therapy, they are still overall at a higher risk of eventually needing surgery. I think, at least, that the education up front doesnt hurt.
The timeline for discussing surgery with an IBD patient often depends on whether the patient has UC or Crohns disease. Another factor is whether a patient presents electively in an outpatient setting, or whether the patient is admitted to the hospital in an emergent or urgent situation. In these situations, the goal is to arm the patient with knowledge of available options without causing undue alarm.
Healio: The conversation about surgery differs between patients with UC and those with Crohns. Can you discuss each condition?
Healio: Overall, do these surgeries turn out well?
Elective Surgical Management Of Ulcerative Colitis
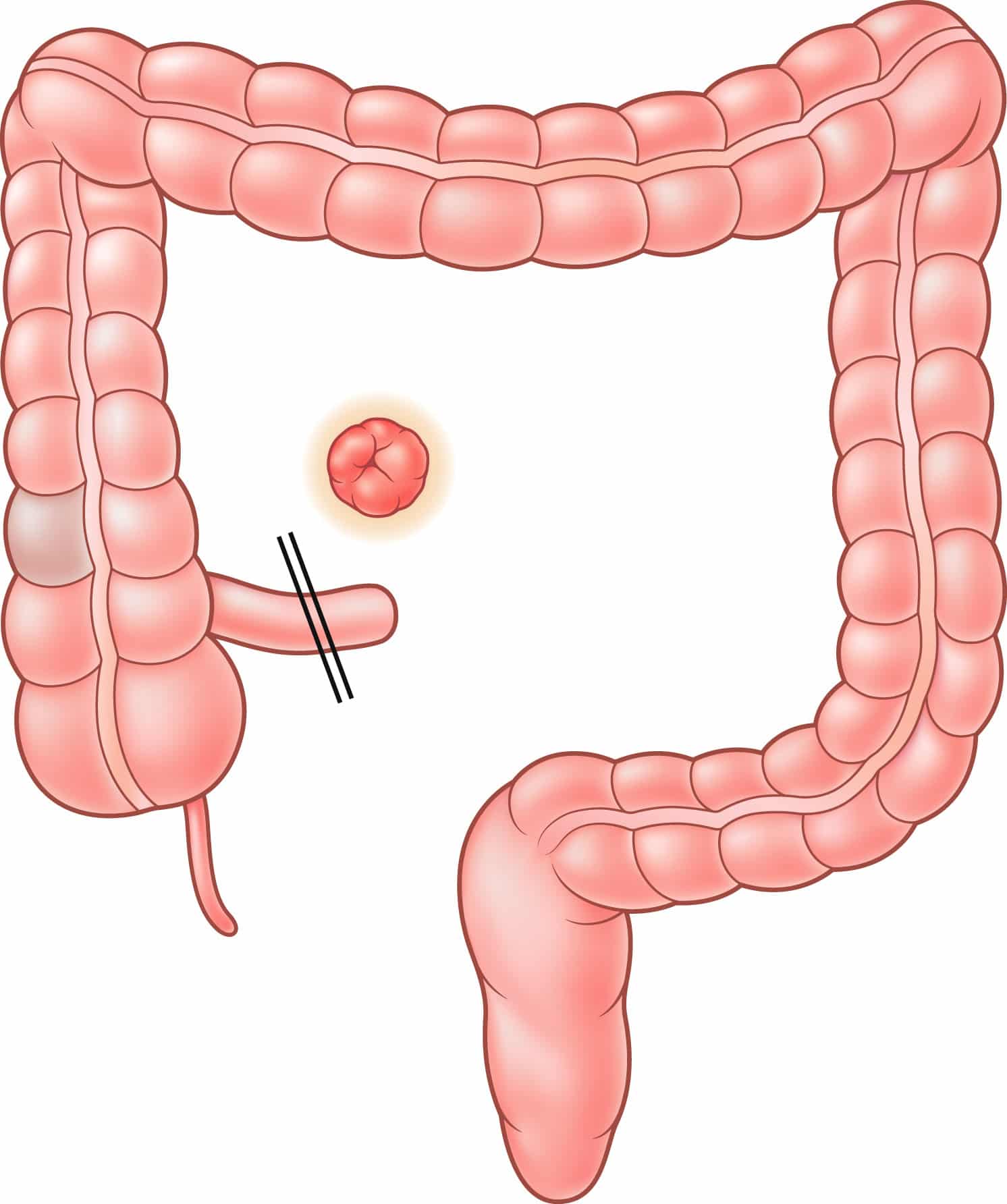
Surgical options for elective management of ulcerative colitis include total proctocolectomy with creation of an end ileostomy, total proctocolectomy with continent ileostomy, total proctocolectomy with IPAA, and total abdominal colectomy with ileorectal anastomosis. Among these, a creation of an IPAA is currently considered the preferred standard of care. Patients who are not suitable candidates for IPAA can be treated with laparoscopic total proctocolectomy and end ileostomy. On the other hand, laparoscopic surgery in the creation of an ileorectal anastomosis following total abdominal colectomy is technically feasible, but is rarely indicated. Similarly, total proctocolectomy and creation of a continent ileostomy is generally performed on patients who had previous surgical procedures for ulcerative colitis and is therefore typically performed using open technique. Ileorectal anastomosis and continent ileostomy will therefore not be further discussed in this review.
Don’t Miss: Treatment Of Ulcerative Colitis In Child
Joint Pain Common Among Uc Sufferers
As numerous articles relate, yes, joint pain is a common symptom of UC affecting the body outside of the stomach and intestines . My throbbing elbows as I type this article also confirm what I read in various medical journals. It seems that the inflammation of the intestines opens the door to inflammation spreading to other areas of the body. Well, thank you, colitis! You have punched me again with yet another issue.
On a good note, treatment is available. Sometimes just taking pain relievers like ibuprofen or aspirin can help. But someone living with an IBD has to be careful with these over-the-counter treatments. Often, they irritate the stomach lining. Intestinal irritation is what we folks living with IBD are avoiding.
Instead, I now have a new issue to discuss with my gastroenterologist. Hopefully, he can assess whether my pain results from colitis or not. More importantly, I trust he offers treatment options that wont exacerbate my intestinal issues.
Dont Miss: What Does Ulcerative Colitis Stool Look Like
What Is Ulcerative Colitis
Ulcerative colitis is a chronic disease of the colon or large intestine. It is marked by inflammation and ulceration in the colons innermost lining. Tiny, open sores form on the surface of this lining they bleed and produce pus and mucus. Because the inflammation makes the colon empty frequently, symptoms include diarrhea and, often, abdominal cramping.
The inflammation usually begins in the rectum and lower colon, but it may involve the entire colon. When it affects only the lowest part of the colon the rectum it is called ulcerative proctitis. If it affects only the left side of the colon, it is known as limited or distal colitis. Ulcerative colitis involving the entire colon is called pancolitis.
Also Check: Bowel Ulcers Signs And Symptoms
Functional Results Cosmesis And Body Image
It is important to point out that both in case-matched studies and especially in purely retrospective analyses, patient selection could explain at least some of the differences in favor of laparoscopic IPAA. The evidence to date suggests that there might be some functional and quality of life benefits associated with laparoscopic IPAA. However, the consistency and relevance of these benefits remains questionable and will require further evaluation with longer follow-up.
How Is Ulcerative Colitis Different From Crohns Disease
Ulcerative colitis is different from other inflammatory bowel diseases like Crohns disease. Crohns can affect any area of the gastrointestinal tract, including the small intestine and colon. Ulcerative colitis, on the other hand, affects only the colon. The inflammation involves the entire rectum and extends continuously up the colon. There are no normal areas of the intestine between the areas of ulceration. In Crohns, the inflamed areas are scattered and can affect the entire thickness of the bowel wall.
Don’t Miss: What Can Cause Ulcers In The Intestines
Surgery Can Truly Help
While surgery is always a major step and not without risks and complications, UC is principally surgically curable when the large intestine is removed because its limited to the colon and rectum, according to a study in Viszeralmedizin. While chronic pouchitis is one of the main factors limiting surgical success in curing UC, theres still a long-term pouch success rate of > 90%, 10 and 20 years later, researchers found. For most patients, when they get the surgery, there is actually a sense of relief, says Dr. Bedford. No more bloody stools. And typically no more abdominal pain and steroids.
Caring For An Ostomy Bag
If you need this bag after your surgery you’ll get advice from your medical team about how to care for it and the stoma. You can empty or throw out the bags when you need to. Irrigating the stoma can help you control the timing of bag changes. To prevent leaks, the pouch system that connects the stoma to the bag needs to be changed every 4 to 7 days. Call your doctor if you notice a change in color, bleeding, or swelling.
Also Check: Dakin’s Solution For Pressure Ulcers
When Is Surgery Needed For Ulcerative Colitis
In severe cases, or when a patient doesnt respond to medication, surgery may be necessary to remove part or all of the colon.
At WakeMed, ulcerative colitis patients can have minimally invasive, laparoscopic-assisted surgeries. This allows a patient to have less pain and discomfort, smaller incision, quicker recovery and fewer complications.
Learn more about what to expect from colorectal surgery.
How Common Is Surgery For Ulcerative Colitis
About 25% to 40% of people with ulcerative colitis will have to have surgery to remove their colons. The reasons that surgery becomes necessary include:
- Medical treatment for instance, drug therapy fails to provide results.
- There may be a risk of cancer without surgery.
- The colon has ruptured.
- The patient experiences a severe, sudden onset of the disease.
- There is extensive bleeding.
- Treatment causes side effects severe enough to compromise the patients health.
- Toxic megacolon has set in. In this dangerous condition, the muscles of the large intestine are dilated, and the colon can rupture.
In some cases, surgery to remove the colon is recommended if other treatments do not work or if the side effects of medications are harming the patient.
Recommended Reading: Hydrocolloid Dressing For Stage 1 Pressure Ulcer
What Can Be Expected After Ileal Pouch Surgery
In most cases after ileal pouch surgery, quality of life improves over time. Patients can usually resume normal work and activities about 4-8 weeks after surgery. What ulcerative colitis patients like most about having any kind of pouch is that they no longer have the severe urgency or need to run to the bathroom.
After ileal pouch surgery, the patient must have an examination of the inside of the pouch with an instrument called an endoscope every year or every other year for the rest of his or her life to watch for the development of precancerous cells. In addition, all types of pouches can develop pouchitis, an irritation and inflammation of the inner lining of the pouch. Pouchitis is very common, but usually responds to oral antibiotics within 24 hours.
Overall, the long-term success rate of the pouch procedure is approximately 95%. However, there is a 5-10% chance of failure after pouch surgery. Most failures are due to the wrong diagnosis , persistent severe pouchitis, or complications of surgery.
In some cases, the pouch may need to be repaired or removed and replaced with a new pouch. Another option is to convert the pouch to a permanent ileostomy .
You May Like: L Glutamine Ulcerative Colitis Dosage
What To Eat After Surgery
Ask your doctor when itâs safe to eat solid meals. It will take some time for your intestines and gut bacteria to digest food as normal. While you recover, your colon may also have trouble absorbing water. Make sure to drink 8-10 glasses of water or other fluid a day.
You might have:
- Smelly or frequent gas
To give your gut a rest, your doctor may have you follow a low-residue diet for about 4-6 weeks. This will make you have smaller bowel movements and go less often. It cuts out most fiber as well as some dairy. Some âlow-residueâ foods include:
- Tofu or meat that is easy to eat
Some foods you should avoid include:
- Processed meat like hot dogs or sausage
- Beans, peas, lentils, and legumes
Also Check: Homeopathic Medicine For Ulcerative Colitis
Inflammation From Ulcerative Colitis
It seems that arthritis, or inflammation of the joints, is a common IBD complication. This problem limits ones mobility and potentially causesdaily pain that, in turn, affects work, exercise, or life in general.
For me, I detect it most at night. The throbbing pain awakens me many times throughout each night. If I lie in certain positions too long, my elbows shoot pain up my arms. Often, it hurts to move and stretch my arms out fully. Sometimes, my fingers and elbows seem to be at war with one another as in which area wants to cramp and hurt the most.
But this pain doesnt just occur at night. During the day, I also experience the aches, screams, and complaints of my elbows, ankles, and fingers. I never even realized the connection between my IBD and joint pain until a friend of mine with Crohns happened to mention it one day.
In my head, I thought, Really? As if a life of bloating, gut pain, diarrhea, and rectal bleeding arent enough with colitis? So, my online investigation on the connection between joint pain and ulcerative colitis began.
What Are Other Peoples Experiences With Colectomies
The idea of a colectomy can be scary, and its normal to feel emotional before surgery. One MyCrohnsAndColitisTeam member shared, Im really nervous for the moment Im fully awake after surgery as I dont know how my body will physically be feeling, and that scares me. I am basically saying goodbye to my old stomachs appearance and adjusting to a completely new way of living.
Along with its benefits, a colectomy may cause several problems. Some people find the surgery painful. I first had a total colectomy. The second surgery was to build a J-pouch, remove my rectum, and place another ostomy, wrote another member of MyCrohnsAndColitisTeam. It was so painful, and removal of the drain was terrible.
A member shared that surgery led to problems being intimate. I have an ileostomy. It does not bother my husband at all. I, on the other hand, feel a lot less sexy. And I have to be careful of the different positions because it will pop my seal, they wrote.
However, many MyCrohnsAndColitisTeam members have reported that colectomies and ostomies have greatly improved their life. It came to a point where my son was suffering almost every day, said one member. It was no way to live. Now my son has a chance at a healthy life.
A different member shared, I personally feel like I have my life back.
Recommended Reading: Interprofessional Care For Ulcerative Colitis
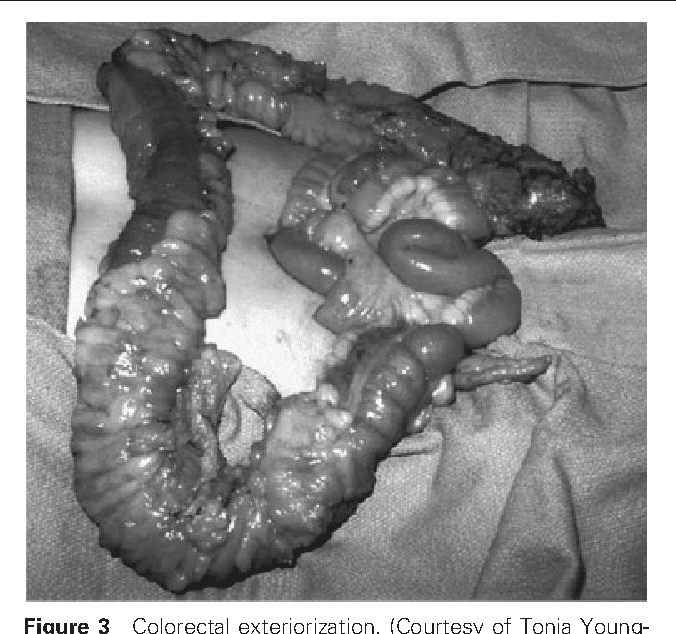
Timing Of Surgical Intervention
Timing of the surgical intervention is the major preoperative concern in UC. Emergency surgery should be avoided if possible, but if it is indicated, most advocate use of a staged procedure. Initially, emergency total colectomy with end ileostomy is performed to alleviate the major symptoms of the disease, including bleeding and pain, and allows the patient to be weaned from steroids.
Later, an IPAA is created, if the patient desires it, with removal of the remaining rectum. Most advocate leaving the rectum in place during the initial emergency operation to prevent disruption of the pelvic tissue planes, with the aim of making the subsequent pelvic dissection safer. If the patient has mild disease or disease in remission, total proctocolectomy with the creation of an IPAA may be performed as the initial definitive procedure.
Lifestyle Changes After A Colectomy
Once a person is healed from a colectomy, they can usually go back to being active, going to work, and taking part in their regular hobbies and activities.
In one study of people with UC who had had a colectomy, 81 percent of participants said that they had problems such as:
- Being unable to eat certain foods
- Feeling self-conscious about their body
- Having mental health issues, including depression
- Having trouble getting things done at work
- Having problems with sexual function
Despite these issues, 84 percent of the people in this study said they had a better overall quality of life after surgery.
Your gastroenterologist may put you on a different diet if you have an ostomy. For example, you will probably have to make sure to drink extra fluids. It may also help to eat foods that contain pectin, such as peanut butter, bananas, and applesauce, in order to reduce diarrhea. Many people with an ostomy also prefer to avoid foods that cause gas. Your doctor can help you learn more about what types of foods will be best for you.
You May Like: Do Ulcers Make You Bloated
Surgery For Ulcerative Colitis: Before During And After
Patient
Physicians have an extensive therapeutic arsenal for treating patients with ulcerative colitis. Available drugs keep the disease inactive or in remission in most cases. Despite this between 25% and 40% of patients with ulcerative colitis will need surgical treatment at some point in their illness1.
Unlike Crohns Disease2, surgery in ulcerative colitis is curative. The fact is that, by affecting the rectum and the colon, its removal implies the total healing of the patient.
In particular, surgery is indicated3 when the pharmacological treatment has not controlled the symptoms of ulcerative colitis when complications such as stenosis , perforation, severe bleeding, abscesses or fistulization occur when premalignant or carcinogenic lesions develop or when perianal disease occurs and drainage surgery is necessary, derivative colostomies to isolate fistulas from passing stool or radical protections in advanced cases.