When To Worry About Blood In Stool
But if you donât know the cause of the bleeding, or it keeps coming back, itâs a good idea to call your healthcare provider. Infections, inflammatory conditions, and polyps need to be treated by a doctor.
Always call your healthcare provider if:
- The bleeding doesnât stop
- You see large amounts of blood
- You have other symptoms like pain or pressure in your rectum
- You feel dizzy, lightheaded, weak, or confused
Nobody expects to see bright red blood with a bowel movement â it can be quite a shock, especially if you canât think of an obvious cause.
If you do see blood, chances are very good that it was caused by something minor and easily treated. But knowing is best. Call your healthcare provider so you can be sure of your diagnosis and treatment. When rectal bleeding is a sign of something more serious, starting treatment sooner is always better than later.
Donât continue experiencing blood in stool schedule an appointment today!
What Are The Possible Complications
An untreated ulcer that swells or scars can block your digestive tract. It can also perforate your stomach or small intestine, infecting your abdominal cavity. That causes a condition known as peritonitis.
A bleeding ulcer can lead to anemia, bloody vomit, or bloody stools. A bleeding ulcer usually results in a hospital stay. Severe internal bleeding is life-threatening. Perforation or serious bleeding may require surgical intervention.
You May Like: What To Take For An Ulcer Over The Counter
Abnormalities Of The Gut
In young children various abnormalities of the gut or the gut wall may cause rectal bleeding. Examples include:
- Volvulus – a twisting of the gut.
- Intussusception – one part of the gut is sucked into another, creating a blockage.
- Meckel’s diverticulum – an extra bulge or pouch in the small intestine, present from birth .
- Hirschsprung’s disease – a condition where a part of the lower bowel does not function as it should. The muscles of the bowel wall are unable to squeeze along the faeces as they should do.
- Abnormal blood vessel development.
Read Also: Ulcerative Colitis Right Side Pain
What Are Causes To Bleeding Ulcers In The Stomach
Causes Use of NSAIDs. High doses of common NSAIDs such as ibuprofen and aspirin may cause peptic or bleeding ulcers. H. pylori infection. Zollinger-Ellison syndrome Zollinger-Ellison syndrome is an uncommon condition that causes tumors in the stomach, duodenum, or pancreas. Ulcers with other causes.
Ulcerative Colitis And Other Forms Of Colitis
Ulcerative colitis is a disease where inflammation develops in the colon and rectum. A common symptom when the disease flares up is diarrhoea mixed with blood. The blood comes from ulcers that develop on the lining of the inflamed gut. There are other rare causes of inflammation of the colon or inflammation of the rectum that can cause rectal bleeding. See the separate leaflet called Ulcerative Colitis for details.
Don’t Miss: What Do Diabetic Ulcers On The Feet Look Like
Colon Cancer And Polyps
Tumors of the colon and rectum are growths arising from the wall of the large intestine. Benign tumors of the large intestine usually are called polyps because of their shape. Malignant tumors of the large intestine are cancers, and most are believed to have developed from polyps. Bleeding from colon polyps and cancers tends to be mild , intermittent, and usually does not cause low blood pressure or shock.
Cancers and polyps of the colon and rectum can cause bright red rectal bleeding, maroon colored stools, and sometimes melena. The colon cancers and polyps located near the rectum and the sigmoid colon are more likely to cause mild intermittent bright red rectal bleeding, while colon cancers located in the right colon are more likely to cause occult bleeding that over time can lead to moderate or severe iron deficiency anemia.
Dont Miss: How Do You Lose Fat Around Your Stomach
If Your Ulcer Was Caused By Helicobacter Pylori
Most stomach ulcers are caused by infection with H. pylori. Therefore, a main part of the treatment is to clear this infection. If this infection is not cleared, the ulcer is likely to return once you stop taking acid-suppressing medication. For more information, see the separate leaflet called Helicobacter Pylori.
You May Like: How To Calm Ulcerative Colitis Flare Up
What Tests Are There For A Stomach Ulcer
If your doctor thinks you may have a stomach ulcer, the initial tests will include some blood tests. These tests will help to check whether you have become anaemic because of any bleeding from the ulcer. The blood test will also check to see that your liver and pancreas are working properly.
The main tests that are then used to diagnose a stomach ulcer are as follows:
- A test to detect the H. pylori germ is usually done if you have a stomach ulcer. The H. pylori bacterium can be detected in a sample of stool , or in a breath test, or from a blood test, or from a biopsy sample taken during a gastroscopy. See the separate leaflet called Helicobacter Pylori for more details.
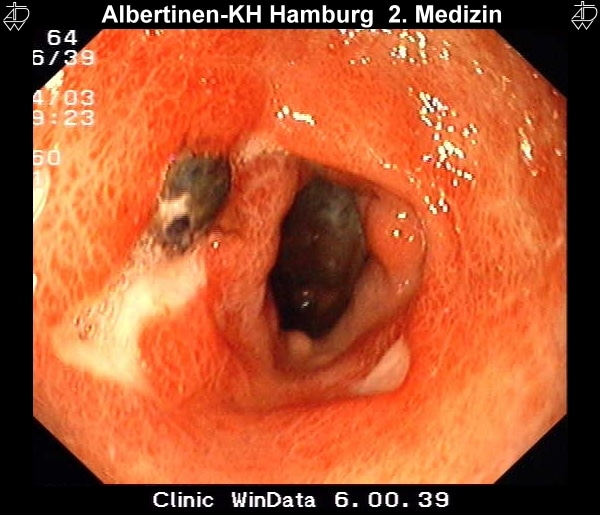
- Gastroscopy is the test that can confirm a stomach ulcer. Gastroscopy is usually done as an outpatient day case. You may be given a sedative to help you to relax. In this test, a doctor looks inside your stomach by passing a thin, flexible telescope down your gullet . The doctor will then be able to see any inflammation or ulcers in your stomach.
- Small samples are usually taken of the tissue in and around the ulcer during gastroscopy. These are sent to the laboratory to be looked at under the microscope. This is important because some ulcers are caused by stomach cancer. However, most stomach ulcers are not caused by cancer.
Also Check: Does Ulcer Pain Come And Go
How Do You Treat Melena
Diagnosis or treatment begins by identifying the sources of bleeding in order to determine and treat the underlying cause. An assessment of the individuals medical history is performed to identify related causes, such as chronic NSAID use. A lavage can be used to determine the severity of blood loss and to prepare the GI tract for endoscopy, which is a minimally invasive procedure used to look inside the . An upper endoscopy will often be performed to determine the exact source of bleeding.
Medication therapy with , such as or , can help reduce acid production, which encourages the healing of and thus reduces the risk of recurrent bleeding. Proton pump inhibitors, along with antibiotics, can also be used to treat infection, which is another potential cause of .
If necessary, the bleeding can be controlled through a combination of endoscopic therapies. The most commonly performed endoscopic therapy is injection therapy, in which medication is injected directly into the source of bleeding to encourage rel=nofollow> blood clotting). It is often combined with other endoscopic therapies, such as thermal techniques that apply heat probes to cauterize the bleeding, or mechanical techniques that apply pressure, using devices like clips or rubber band ligation.
You May Like: Hindgut Ulcers In Horses Treatment
Burning Pain In Your Abdomen
This may seem like a no-brainer but the most common sign that people experience when they have a stomach ulcer is a persistent burning pain in their abdomen. This sensation occurs when juices in the stomach used for digestion come into contact with the open sore. For the most part, the pain is felt from the breastbone to navel and is often worse at night than during the day. On the other hand, if you are someone who frequently skips meals, you may find that you experience this pain much throughout the daytime.
Dont Miss: How Long Does A Ulcerative Colitis Flare Up Last
Black Or Dark Red Blood In Stool
The longer blood is in the digestive tract, the darker it appears. Black, tarry stools are a sign of bleeding in the upper part of the digestive tract, such as the esophagus, stomach, and first part of the small intestine. Dark red blood in stool is a sign that bleeding may be in the small intestine or the beginning of the colon.
Causes of black or dark red blood in the stool may include:
- Inflammatory bowel disease
Of course, not all changes in stool color are due to underlying disease. Certain foods and supplements can also change the color of stool. For example, iron supplements and Pepto-Bismol are known to cause black stools. Black or dark red blood in the stool may also result from eating dark-colored foods like blueberries, black licorice, and dark chocolate.
Read Also: Nutritionist Specializing In Ulcerative Colitis
Read Also: Ulcerative Colitis And Back Pain
Gi Bleeding In The Elderly
In the elderly , hemorrhoids and colorectal cancer are the most common causes of minor bleeding. Peptic ulcer, diverticular disease, and angiodysplasia are the most common causes of major bleeding. Approximately 35% to 45% of all cases of acute upper GI hemorrhage occur in elderly persons. These patients increasingly account for the 10% of deaths that result from a bleeding episode each year.4
Elderly patients tolerate massive GI bleeding poorly. Diagnosis must be made quickly, and treatment must be started sooner than in younger patients, who can better tolerate repeated episodes of bleeding.9
Can Stomach Olsers Cause A Lot Of Blood In Your Stool
Ask U.S. doctors your own question and get educational, text answers â its anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â its anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
You May Like: Classic Features Of Ulcerative Colitis
Read Also: Over The Counter Ulcer Medication
When To Contact A Medical Professional
Contact your health care provider right away if:
- You notice blood or changes in the color of your stool
- You vomit blood
- You feel dizzy or lightheaded
In children, a small amount of blood in the stool is most often not serious. The most common cause is constipation. You should still tell your child’s provider if you notice this problem.
How To Prevent Gastrointestinal Bleeding
The prognosis for a person with GI bleeding depends upon the cause and location of the bleeding, how bad the bleed is when the person sees the doctor, and any underlying medical conditions that may affect the patients recovery.
-
Alcohol & Upper GI Bleeding
For those that consume alcohol, do so in moderation. Patients with high alcohol consumption are widely at risk for gastrointestinal bleeding within the upper digestive tract, which can result in death. Alcohol also accelerates the development of gastritis, which is an inflammation of the stomach lining. Over time, the inflammation can lead to erosion of the stomach lining, which plays a vital role in regulating stomach acid.
-
NSAIDs Increase The Risk Of Lower GI Bleeding
Non-steroidal anti-inflammatory drugs, or NSAIDS, are drugs that intend to reduce pain and fever, prevent blood clots, and reduce inflammation. They can also cause gastrointestinal bleeding, so it would be best to take these medications as rarely as possible. Examples of NSAIDs include ibuprofen, Advil, Motrin, aspirin, Celebrex, and Naproxin.
-
Can Smoking Cause Gastrointestinal Bleeding?
The risk of developing gastrointestinal bleeding increases significantly in individuals that smoke. Smoking not only causes peptic ulcers and other severe medical conditions, but it also can slow down the healing process for peptic ulcers. Furthermore, smoking interferes with ulcer medication, making the treatment less effective.
Also Check: Can Stress Give You An Ulcer
Inflammation In Other Areas
Some people with IBD have painful inflammation in other areas of the body, including:
- joints of the fingers, hands, feet, ankles and knees
- joints of the spine, including vertebrae and sacroiliac joints
Two specific skin problems that can occur as a result of IBD are:
- pyoderma gangrenosum small, sunken ulcers on the skin
- erythema nodosum painful, small, reddened nodules on the skin .
Dont Miss: Ulcer On White Of Eye
Treatment Of Gi Bleeding
-
Sometimes drugs
-
In some, endoscopic or angiographic hemostasis
Hematemesis, hematochezia, or melena should be considered an emergency. Admission to an intensive care unit or other monitored setting, with consultation by both a gastroenterologist and a surgeon, is recommended for all patients with severe GI bleeding. General treatment is directed at maintenance of the airway and restoration of circulating volume. Hemostasis and other treatment depend on the cause of the bleeding.
Read Also: Best Vitamins For Mouth Ulcers
What Is A Gastrointestinal Bleed
A GI bleed isnt a condition or disease, but the symptom of one. You can have an acute bleed one that occurs quickly and suddenly, or a chronic bleed. A chronic GI bleed may come and go and usually isnt severe. It still should be investigated though, because your doctor needs to know why its occurring and if left for too long, a chronic bleed can cause other complications like anemia.
What Will A Doctor Do About The Blood In My Stool
Rectal bleeding is commonly evaluated and treated by gastroenterologists. The first priority upon receiving a patient with rectal bleeding is always to correct any low blood volume or anemia, with fluids or a blood transfusion. They will then determine the site and cause of the bleeding, stop the bleeding, and prevent bleeding in the future if possible.
The doctor may order repeated blood tests to monitor changes, and will often initiate a colonoscopy or an endoscopy, depending on where they suspect the bleeding is happening .
You May Like: How To Get Tested For Stomach Cancer
Recommended Reading: What Will Help Stomach Ulcer Pain
What Foods Can You Eat On A Ulcerative Colitis Diet
If you have ulcerative colitis you may need to modify your diet to help manage the symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient.
Depending on symptoms different types of diets may be recommended, such as:
- a high-calorie diet
What Is The Prognosis For People With Gastritis
Most cases of gastritis improve quickly with treatment. For most people, medications relieve gastritis. Your healthcare provider will recommend the most appropriate treatment based on whats causing gastritis. Antacids reduce stomach acid, while antibiotics clear up bacterial infections. You can also make changes like reducing your alcohol consumption and managing pain without NSAIDs.
Also Check: How To Cure Ulcer Naturally
Also Check: What Do I Take For An Ulcer
How Do H Pylori Cause A Peptic Ulcer And Peptic Ulcer Disease
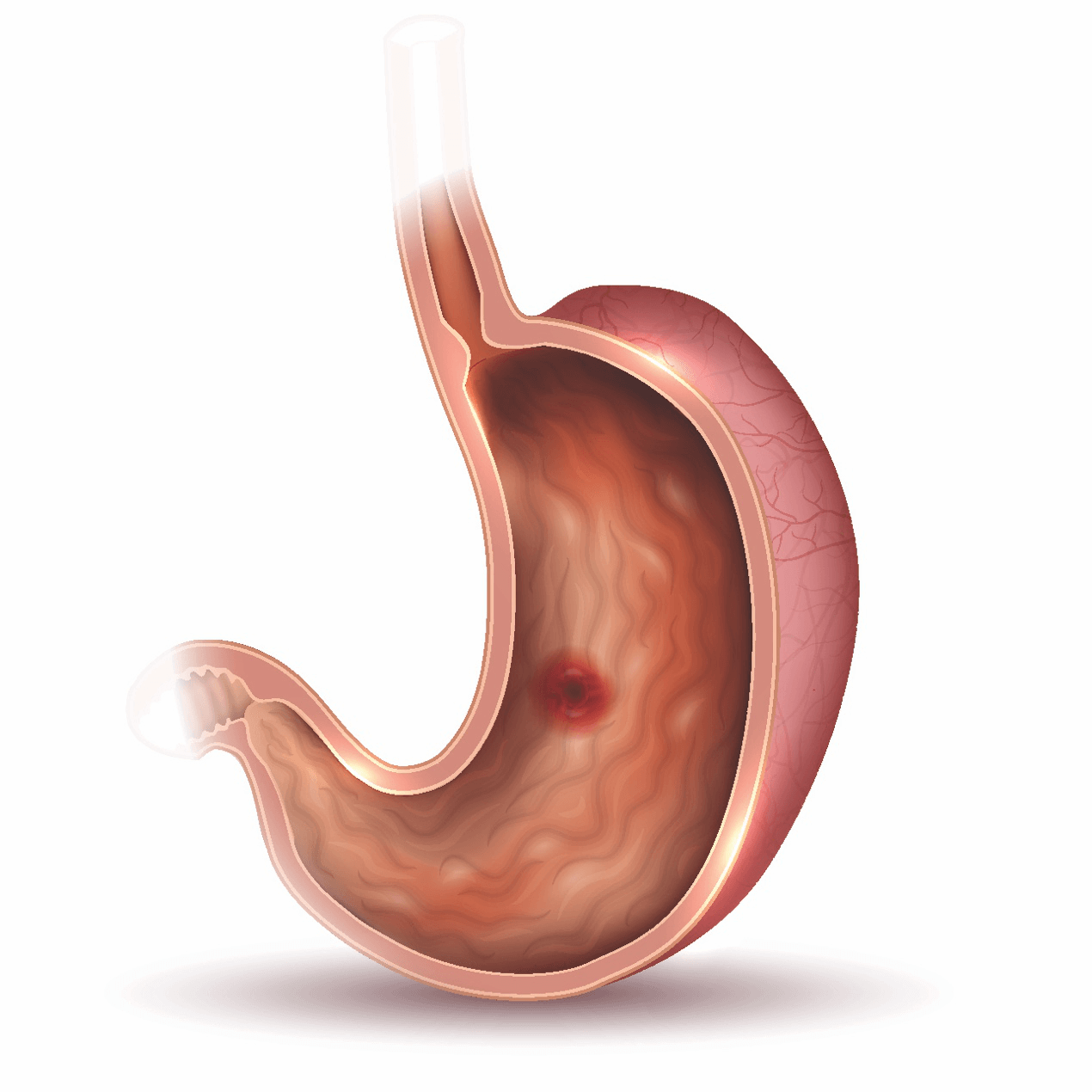
H. pylori are spiral-shaped bacteria that can cause peptic ulcer disease by damaging the mucous coating that protects the lining of the stomach and duodenum. Once H. pylori have damaged the mucous coating, powerful stomach acid can get through to the sensitive lining. Together, the stomach acid and H. pylori irritate the lining of the stomach or duodenum and cause a peptic ulcer.
How Do I Know If My Ulcer Is Bleeding
If a peptic ulcer begins bleeding, a person may notice: stools that are dark and sticky. stools that are dark red in color. vomit that looks like coffee grounds or has blood in it.Symptoms
Recommended Reading: Is Constipation A Symptom Of Ulcerative Colitis
Recommended Reading: Celiac Disease And Ulcerative Colitis
Healthi Wasnt Ashamed: Woman Shows Off Colostomy Bags In Stunning Photo
At the time they gave me my diagnosis I was told that this would not affect my quality of life, which could not be further from the truth in my severe case, Vihlen, 31, said. I continued to work for several months after being diagnosed but had to leave my physically demanding job due to the uncontrollable symptoms. Every day is different and I dont know how much energy I will have until I wake up in the morning, so making social plans is very difficult and more often than not I have to cancel at the last minute.
Dont Miss: Ulcerative Colitis Unspecified Without Complications
What Is The Purpose Of A Fecal Occult Blood Test
If you have certain symptoms, such as abdominal pain, fatigue, pain around your rectum or rectal bleeding, your healthcare provider may recommend a fecal occult blood test. The most common reason for an FOBT is to screen for colorectal cancer.
On its own, a fecal occult blood test cant diagnose colorectal cancer or any digestive issue. Depending on the results of your FOBT, you may need more testing to confirm a diagnosis.
You May Like: Diet Plan For Someone With Ulcerative Colitis
How Common Are Stomach Ulcers
Its not known exactly how common stomach ulcers are. They have become much less common since the 1980s because of much more effective treatments. So people with stomach ulcers now usually get better much more quickly.
The term peptic ulcer is used to describe ulcers that are caused by too much acid in the stomach. This includes stomach ulcers and also ulcers in the first part of the gut known as the duodenum. Stomach ulcers are less common than duodenal ulcers.
Dont Miss: What Causes Mouth Ulcers On Gums
Nutritional Supplements For Crohns
Food is ultimately the best source of nutrients, but Crohns usually causes deficiencies. Supplements can complement a balanced diet to help resolve these nutritional deficiencies. A few common ones associated with Crohns disease are:
- Fat-soluble vitamins A, D, E, and K.
Your nutritionist or health care professional may recommend supplementing these. They may also suggest the following:
These supplements also help support overall health as they support gut health and lower inflammation.
Don’t Miss: Early Symptoms Of Ulcerative Colitis
How Do You Treat Ulcers
There are a few things that you can do to relieve the symptoms of stomach ulcers. Avoiding spicy and fatty foods, managing stress, using over-the-counter antacids, and stopping the use of NSAIDs may provide relief. Your doctor may treat your peptic ulcer by prescribing antibiotics, or medications to block or reduce acid production.
Its important to know when you should seek care for stomach pain. Persistent abdominal pain that does not go away can indicate an underlying health problem.
Talk to your doctor if you experience frequent abdominal pain, or abdominal pain that does not go away, if you feel faint or have trouble breathing with abdominal pain, or if you have blood in your vomit or stool.
Your primary care doctor can help determine the best action to take, which may include a referral to a gastroenterologist: a physician that specializes in diagnosing and treating digestive diseases.
You May Like: How Do They Test For Ulcerative Colitis