The Tricky Thing About Iron Supplements
Most of the time, doctors prefer you get iron through your diet, but people with UC often have a hard time eating high-iron foods like green leafy vegetables, which can worsen diarrhea. Complicating matters, taking an iron supplement can also be iffy for people with UC, Dr. Yen says, because it may irritate the bowels . The sort-of good news: In cases where iron deficiencies are bad, we can give intravenous irona little easier on the bowels, says Dr. Yen.
Supplements Being Studied For Ulcerative Colitis
Researchers are checking a number of supplements to see if they can help people with UC. In at least one study, omega-3 fatty acids found in fish oil reduced symptoms and prevented UC from returning. Other studies, however, have not had the same results.
Probiotics are “good” bacteria or other microorganisms that can be healthful. Several studies show they reduce ulcerative colitis symptoms. The thinking is that probiotics, like lactobacillus or live-culture yogurt, help to restore balance to the good bacteria that live inside the intestines.
A few studies have seen benefits from aloe vera when you take it in the form of a gel that you swallow, but more research is needed to confirm this.
Talk to your doctor about other supplements that are being studied to see if they can help you manage ulcerative colitis.
Show Sources
How The Gut Microbiome Works
If all systems are operating normally, your large intestine serves as a home to a diverse mix of bacteria that produce and modify molecules that have beneficial physiological functions. This “good” gut bacteria protects the intestine from harmful bacteria that could invade it. It does this by releasing a specialized, anti-inflammatory and immune-beneficial substance called butyrate, a fatty acid. This, in turn, protects the innermost lining of the intestine , which is key to a healthy gut.
The intestinal barrier is made up of a tightly knit network of cells that maintain the guts integrity. A healthy gut relies on the interactions between the gut microbiome and this barrier. If something upsets the balance between the good and bad bacteria in the microbiome or if theres a dysfunction in the intestinal barrier, harmful bacteria can invade the barrier itself, resulting in the intestines immune cells being activated and, ultimately, chronic intestinal inflammation, like you find in people with UC. The interaction between the host, intestinal microbiota, and anti-inflammatory metabolites these bacteria produce, may be a key factor in ulcerative colitis, says Paul-Peter Tak, M.D., Ph.D., a professor of medicine at Amsterdam University Medical Centre in the Netherlands.
Recommended Reading: How Long Does An Ulcerative Colitis Flare Up Last
Why You Might Want An Iron Supplement
Iron is the building block for blood cells, but if you suffer from UC, inflammation and blood loss through ulcers in your GI system make it difficult for your body to absorb enough of the mineral. When your body is sick, it doesnt make blood cells very efficiently, says Dr. Yen. Not only are you losing blood through your ulcers, but your body is probably not making it very fast, either. Thats a problem because if you dont have enough healthy red blood cells to carry oxygen throughout your body, you will develop anemia, causing you to feel super-tired all the time.
Get Help For Ulcerative Colitis With A Specialized Nutrition Plan

Not sure which foods you should be eating? Fed up of having a restricted diet? Our professional dietitians can help you to create an individualized nutrition plan that reduces your symptoms and makes food more enjoyable.
Weve helped hundreds of people just like you with ulcerative colitis. Join us on the road to recovery and apply for a custom nutrition plan today.
Resources
Vitamin D
Omega 3s
Folate
Don’t Miss: New Medicine For Ulcerative Colitis
Common Supplements Recommended For Ibd Patients
Your healthcare provider may recommend that you take vitamin or mineral supplements, especially if you are experiencing nutritional deficiencies. We can help you learn about supplements that are commonly recommended for IBD patients.
This information can help you learn which vitamins and minerals are important to maintain your nutrition, along with the various foods you may want to try as part of your IBD-friendly diet.
Your body is unique. What works for one patient, will not work for everyone. Check with your healthcare providers before starting any supplements, as you will need proper dosing.
How Can Supplements And Vitamins Help
Many practitioners recommend vitamins and supplements for ulcerative colitis to help the body get the nutrition that it needs. Those with UC often dont eat enough food through a loss of appetite or simply in trying to avoid a flare-up of symptoms. This increases the risk of malnourishment and stops your body from getting the calories, vitamins, and minerals it needs to heal.
Some prescribed medicines for ulcerative colitis can also have an effect on how the body absorbs minerals including calcium, vitamin D, zinc and B vitamins.
Read Also: Drinking Alcohol With Ulcerative Colitis
How To Use Sulfasalazine Suppositories
Sulfasalazine suppositories are used to treat inflammatory bowel disease.
You will generally use the suppositories twice a day, in the morning and at bedtime. Use them after you do a poo.
Youre Avoiding Certain Healthy Foods
It can be hard to eat a healthy diet or anything at all if youre experiencing abdominal pain, cramps, or nausea. But if youre not eating the right foods, you could be at risk of nutrient deficiencies, malnutrition, and unwanted weight loss. The National Institute of Diabetes and Digestive and Kidney Diseases says that because people with ulcerative colitis can lose their appetite, it is important to focus on eating a healthy, balanced diet.
While theres no one meal plan that works for everyone, many people find they can tolerate low-fiber fruits , lean proteins, cooked veggies, sourdough bread, and grains such as oatmeal. A doctor or dietitian who specializes in IBD can help you develop a personalized meal plan.
Recommended Reading: Best Cure For Leg Ulcers
Dietary Sources Of Folic Acid
Green leafy vegetables, nuts, beans, and vitamin B9-supplemented products are rich sources of folic acid Table 1 shows the folate content of the selected products . It should be noted that the bioavailability of folate in food is approximately half of that of synthetic folic acid found in supplements , although it is worth bearing in mind that taking supplements with meals reduces bioavailability . Nevertheless, it is difficult to determine the bioavailability of folic acid in different groups of products. In fact, the supplementation of folic acid for five weeks significantly increases the serum folate levels in pregnant women . An enhancement of serum folate levels upon folic acid supplementation in adults has also been observed .
Supplements For Ulcerative Colitis: What Should You Take
by Health Writer
If youre living with ulcerative colitis , you know all about the pain chronic inflammation and ulcers cause in your digestive tract. You also probably know the fatigue that comes from the inflammatory bowel disease interfering with your bodys ability to absorb nutrients. Thats why many people with UC take supplements, says Eugene Yen, M.D., a gastroenterologist and co-chair of the Patient Education Committee for the Crohns & Colitis Foundation. But are supplements necessary? And what types should you consider taking? Heres what the experts have to say.
Don’t Miss: Ulcerative Colitis Mouth Sores Pictures
Food Supplements For Ulcerative Colitis
A well-balanced diet is your first step to guard against malnutrition. You need to eat a variety of things from different food groups and make sure you get enough protein and calories. Work with a dietitian who can help you plan meals that meet your nutrition needs.
Even with a well-designed meal plan, you may still need some of these supplements:
Vitamin D. You need it to keep your bones strong. It also plays a role in how your immune system — your body’s defense against germs — works.
If you have ulcerative colitis, especially if you need steroids, you may be at risk for having low levels of vitamin D.
A good source of vitamin D is dairy foods, but a lot of people with UC cut back on dairy to help them curb symptoms of diarrhea.
Experts have different views on vitamin D supplements, so ask your doctor if it’s a good idea for you to take them.
Calcium. It’s a mineral your body uses to build bones, help your muscles contract, and send messages through your nervous system.
If your system doesn’t have enough calcium, your body removes it from the bones, which causes them to become brittle and leads to a bone-weakening disease called osteoporosis.
If you avoid calcium-rich dairy products or need certain kinds of medicines, you could be at risk for low levels of calcium. If your doctor recommends a calcium supplement, you’ll probably need 1,000 to 1,200 milligrams a day.
Complementary And Alternative Therapies
Diet
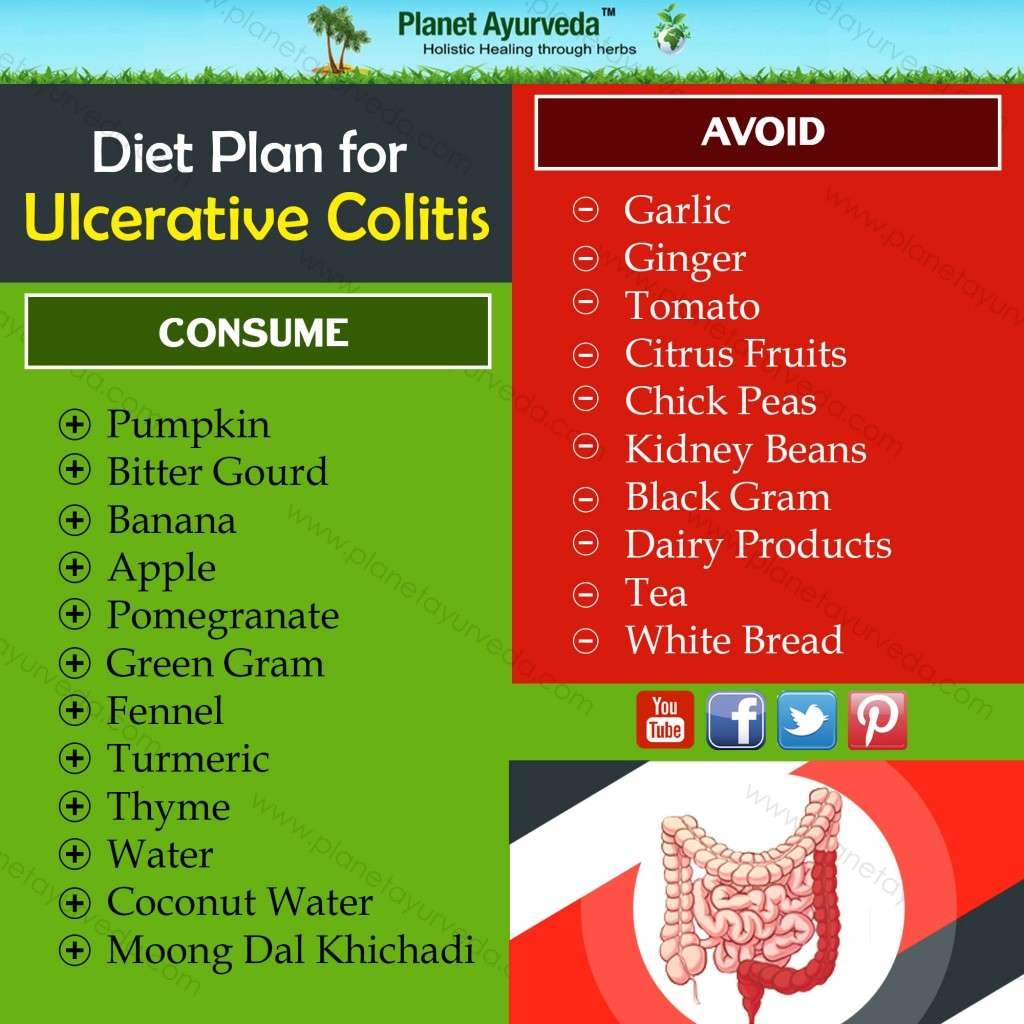
Although diet cannot cure ulcerative colitis, some studies suggest that people who eat foods high in saturated fat and sugar, and who eat less amounts of fruits and vegetables, may be at greater risk of developing the disease. Certain foods may also reduce symptoms.
- Limit intake of dairy products, which may help reduce diarrhea.
- Eat fruits and vegetables and pay attention to fiber. Although fiber is crucial to a healthy diet, some people with inflammatory bowel disease find that fiber makes symptoms worse. If fiber bothers you, steam or bake your vegetables instead of eating them raw, and avoid high-fiber foods such as broccoli, cauliflower, and raw apples. Eat antioxidant foods, including fruits and vegetables .
- A bland, low-fiber diet may be best during acute flares.
- Eat 5 to 6 small meals a day.
- Certain foods may aggravate symptoms of ulcerative colitis .
- Avoid refined foods, such as white breads and pastas.
- Avoid caffeine, alcohol, and tobacco.
People with significant malnourishment, severe symptoms, or those awaiting surgery may require parenteral nutrition.
Nutrition and Supplements
Read Also: Can You Drink Coffee With Ulcerative Colitis
Enumeration Of Colorectal Neoplasms And Colitis Score
At necropsy, the colorectum was removed and flushed with Krebs buffer solution to remove fecal debris. The entire length of the colorectum was opened longitudinally, laid flat on Whatman filter paper, and fixed in 10% neutral buffered formalin. All macroscopic tumors were identified and harvested under a dissecting microscope, processed in a standard manner for H& E staining, and histologically classified as low-grade dysplasia, high-grade dysplasia/carcinoma in situ, or invasive adenocarcinoma according to the previously described criteria by a gastrointestinal pathologist blinded to the study group. In addition, the severity of colitis was graded by the same pathologist in a blinded fashion based on histological examination of the distal colon as follows: grade 0, normal histological findings grade 1, mild thickening of the colon with often focal involvement of the mucosa grade 2, moderate thickening of the colon with diffuse involvement of the mucosa or grade 3, marked thickening of the colon with occasional crypt abscesses and the presence of focal lymphoid aggregates .
Special Precautions & Warnings
Pregnancy and breast-feedingLIKELY SAFE
Procedures to widen narrowed arteries : Using folic acid, vitamin B6, and vitamin B12 intravenously or by mouth might worsen narrowed arteries. Folic acid should not be used by people recovering from this procedure.
Cancer: Early research suggests that taking 800 mcg to 1 mg of folic acid daily might increase the risk of cancer. Until more is known, people with a history of cancer should avoid high doses of folic acid.
Heart disease: Early research suggests that taking folic acid plus vitamin B6 might increase the risk for heart attack in people with a history of heart disease.
Malaria: Early research suggests that taking folic acid plus iron might increase the risk of death or need for treatment in hospital in areas of the world where malaria is common.
Anemia caused by vitamin B12 deficiency: Taking folic acid might mask anemia caused by vitamin B12 deficiency and delay appropriate treatment.
Seizure disorder: Taking folic acid supplements might make seizures worse in people with seizure disorders, particularly in high doses.
Recommended Reading: How Do You Cure A Stomach Ulcer
Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
Youre Skipping Your Uc Medications
The most important thing to do if you have UC? Take your medications as prescribed, and work closely with your doctor to stay well, says Richard Bloomfeld, MD, a gastroenterologist and professor at Wake Forest Baptist Medical Center in Winston-Salem, North Carolina.
A variety of medications can treat UC, depending on the severity of your condition and your overall health. While it may be tempting to skip doses once you start feeling better a report published in the journal Intestinal Research reported that medication adherence is a significant problem for people who have inflammatory bowel disease doing so can cause your symptoms to reappear.
Skipping medications is the biggest reason people experience flares, says Laura Yun, MD, a gastroenterologist and assistant professor of medicine at Feinberg School of Medicine at Northwestern University in Chicago. Whether your doctor has you taking an anti-inflammatory drug, an immunosuppressant, or a combination of medications, none of them will work if you dont take them as your doctor prescribes.
You May Like: Preventing Pressure Ulcers In Nursing Homes
Cautions With Other Medicines
There are some medicines that can affect the way sulfasalazine works.
Tell your doctor or pharmacist if you’re taking:
- digoxin, a medicine for heart problems
- medicines for high blood sugar or diabetes, such as metformin or glibenclamide
- methenamine, a specific antibiotic sometimes used for treating urinary tract infections
- folic acid, often taken in first 12 weeks of pregnancy, as it may be less well absorbed so you may need to take a higher dose than usual
- azathioprine or mercaptopurine, taken for rheumatoid arthritis or to prevent organ rejection after a transplant
- methotrexate which is usually used to treat rheumatoid arthritis
Diet Doesnt Always Cover Your Needs
Fantasy: You eat a well-balanced diet that gives you all the vitamins and minerals you need every day. Reality: During a UC flare, there is often nothing balanced about whats going inor coming outof your body. If youre having a lot of diarrhea, the food and nutrients you consume may not have a chance to be fully absorbed, says Javelli. Plus, many people avoid certain nutrient-dense foods such as fruit, vegetables, and whole grains because these can worsen symptoms, leaving you a day late and dollar short when it comes to nutrition.
Don’t Miss: Do Stomach Ulcers Cause Gas
You Need Your Meds Adjusted
Antibiotics for an infection outside of your gut could aggravate UC symptoms. Let your doctor know if you experience diarrhea after starting antibiotics, since a switch in the type of drug might be needed. Aspirin, ibuprofen, and naproxen can also trigger a UC flare.
Your doctor may also suggest taking an antidiarrheal medication. Probiotics beneficial live microorganisms that live in your gut may also help reduce diarrhea, according to the NIDDK, although its not clear how many of them you have to take or which strains may be most helpful. If you do decide to take a probiotic, always talk to your doctor first.
What Is Ulcerative Colitis
Ulcerative colitis is a long-term form of Inflammatory bowel disease that causes inflammation to the colon or large intestines. This results in small ulcers which cause bleeding along the lining of the colon.
While the exact cause of UC is unknown, its usually the result of an immune system dysfunction. Normally the immune system defends the body against infection. But for those with ulcerative colitis, their immune system mistakenly attacks healthy tissue, food and good bacteria that lines the colon, resulting in inflammation and sores.
The main symptoms are bloody diarrhea, stomach pain and frequently going to the toilet. But there are also many other signs including fatigue, weight loss, lack of appetite, and dehydration.
While there isnt a cure for ulcerative colitis, making changes to your diet with the help of an expert licensed dietitian thats specialized in IBD can reduce symptoms and help to reduce inflammation.
You May Like: Genetic Testing For Ulcerative Colitis