What Are The Contraindications For Fish Oil Supplementation
High doses of omega-3 fatty acids may be harmful, resulting in increased bleeding risk and might suppress the immune system.2 Some patients have reported symptoms such as abdominal pain and diarrhea as a result of fish oil supplementation. Fish oil supplementation should only be administered under the supervision of a healthcare provider. As with any medicinal treatment, alert your healthcare provider of any medications or supplements you are taking, as certain drugs could have adverse interactions.
What About An Omega
If your diet is low in omega-3 fatty acids, a supplement may be considered. There are a number of supplements on the market that contain omega-3 fatty acids.
For example, if you are aiming to consume 500 mg/day of EPA + DHA combined, you should look for a label like this:
Each Capsule Contains:
- Eicosapentaenoic Acid – 300 mg
- Docosahexanoic Acid – 200 mg
Making omega-3 fatty acids work for you:
- Eat two or more servings of fatty fish each week.
- Use flaxseed, canola, soybean, or olive oil when cooking or baking.
- Consider taking a daily omega-3 fatty acid supplement.
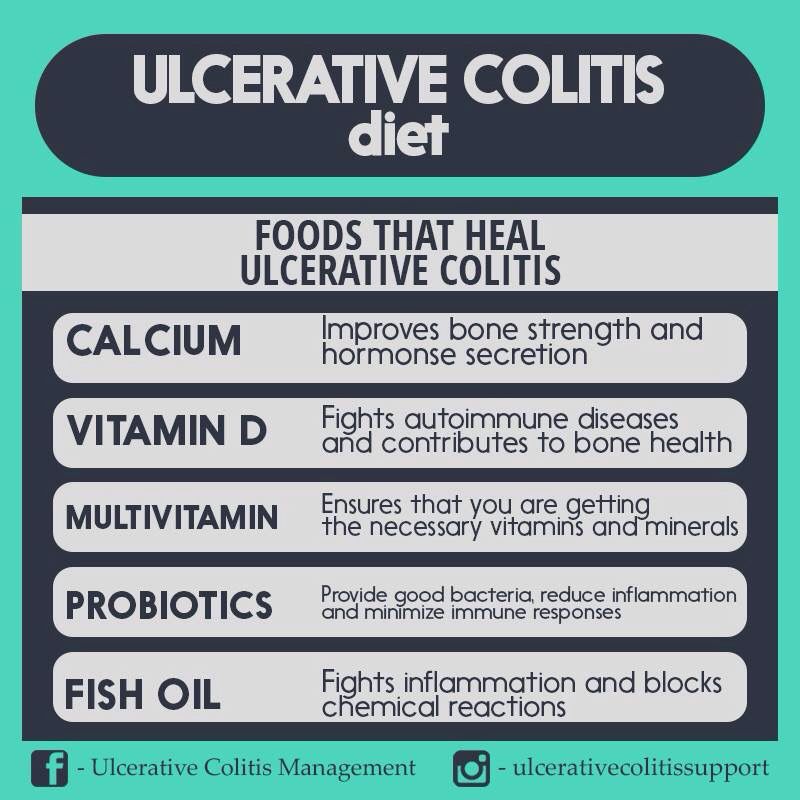
Vitamins Minerals And Supplements
If you have Crohns or ulcerative colitis, vitamin and mineral supplements may be recommended, especially if you are at risk for nutritional deficiencies. Deficiencies can be caused by certain medications, surgeries, or active inflammation from IBD, which can affect your bodys ability to absorb certain vitamins and minerals.
For many with IBD, eating a healthy diet rich in foods with vitamins and minerals may be all that you need. However, some patients may have trouble absorbing enough vitamins and minerals from food alone.
Complementary Medicine for IBD: Vitamins, Minerals, and Herbs
There are some supplements currently under investigation that may provide additional benefits for IBD patients:
Recommended Reading: What Is The Best Medicine For Ulcerative Colitis
What Is Ulcerative Colitis
Ulcerative colitis is a long-term form of Inflammatory bowel disease that causes inflammation to the colon or large intestines. This results in small ulcers which cause bleeding along the lining of the colon.
While the exact cause of UC is unknown, its usually the result of an immune system dysfunction. Normally the immune system defends the body against infection. But for those with ulcerative colitis, their immune system mistakenly attacks healthy tissue, food and good bacteria that lines the colon, resulting in inflammation and sores.
The main symptoms are bloody diarrhea, stomach pain and frequently going to the toilet. But there are also many other signs including fatigue, weight loss, lack of appetite, and dehydration.
While there isnt a cure for ulcerative colitis, making changes to your diet with the help of an expert licensed dietitian thats specialized in IBD can reduce symptoms and help to reduce inflammation.
What Is Fish Oil
Fish oil is a type of food that contains omega-3 fatty acids. Your body needs omega-3s for a lot of functions like cell growth, fighting diseases, energy production, and muscle activity. But your body canât make them naturally, so you have to get them through foods or supplements.
There are three types of omega-3s:
Fish oil is a good source of omega-3s and contains DHA and EPA. The fatty acid is known for its anti-inflammatory effects on your body, especially against specific conditions like heart disease, high blood pressure, cholesterol, and rheumatoid arthritis.
Read Also: How To Reduce Stomach Ulcer
Fish Oil In The Treatment Of Ulcerative Colitis
Abstract
Patients with active ulcerative colitis have increased levels ofleukotriene B4 in their rectal mucosa. Eicosapentaenoic acid competitivelyinhibits the cyclo-oxgenase pathway and reduces the formation of cyclo-oxygenasepathway products. EPA is a good substrate for lipoxygenase enzymesand is efficiently converted to leukotriene 85, which is less biologically active.The conversion of EPA to leukotriene B5 is as efficient as that of arachidonicacid to teukotriene B4. Two pilot studies showed benefit of EPA in the treatmentof ulcerative colitis. Two of three controlled studies suggest that EPA is moreeffective than placebo in the treatment of active chronic ulcerative colitis. Themechanism of action is probably reduction of leukotriene B4, but EPA couldincrease cell and lysosomal membrane stability, or it may exert its effect byreducing interleukin-l. More controlled studies and detailed investigation intothe mode of action of EPA are required.
Copyright
Coconut Water Can Replenish Electrolytes
After a bout of severe diarrhea, a common Crohns symptom, you may need a little more punch than just plain old water. In this instance, for an IBD like Crohns disease, its best to turn to products with added electrolytes. Coconut water a natural source of electrolytes can make a refreshing change, says Catsos. If you choose another electrolyte replacement beverage, she adds, try to avoid those sweetened with high fructose corn syrup or crystalline fructose, or those with artificial coloring. Talk to your doctor if youre concerned about dehydration.
Also Check: Signs Of A Bleeding Stomach Ulcer
Also Check: Can You Eat Cheese With Ulcerative Colitis
Cytokines And Myeloperoxidase Measurements
Ultrasensitive multiplex cytokine profiling kit was used to assess mouse IL-1, IL-6, keratinocyte-derived chemokine , IL-10, IL-12p70, IFN and TNF- in colonic protein extracts according to manufacturers instructions. Proteins from colon samples were prepared in RIPA buffer and protein measured with RC-DC Protein assay kit . MPO content of the colon protein extracts was determined with an ELISA kit following the manufacturers instructions. Cytokines or MPO levels were normalized to total tissue protein contents.
Foods That May Fight Uc
Some research shows that certain nutrients may help fight the irritation and swelling in your gut caused by UC. Scientists have studied how linoleic acid affects people with the condition. Although everyone needs this âgoodâ fat, donât overdo it, since there is some evidence it may play a role in inflammation if you get too much.
Other studies show that an omega-3 fatty acid called EPA may fight inflammation. This is another âgoodâ fat that blocks certain chemicals in your body called leukotrienes. Fish oil is a good source of EPA. In some studies, folks with UC saw some benefits when they took high doses. Many people, though, didnât like the fishy taste. There is also some evidence that adding fish oil to aminosalicylates may be helpful, but this isnât proven. DHA is another omega-3 found in fish oil that can fight inflammation and is used by some people with UC.
Some research also shows that yogurt with gut-healthy bacteria, called probiotics, eases inflammation. Scientists are still studying how they may help people with UC and similar conditions. Some people also believe that a diet low in FODMAPs â a type of highly-fermentable carbs found in meats, fruits, dairy, and lots of other foods â may help ease UC symptoms. But the evidence is unclear if it does. And without close monitoring, any diet that restricts certain foods may lead to poor nutrition and other problems.
Show Sources
Also Check: Differential Diagnosis For Ulcerative Colitis
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
Omega 3 Fatty Acids For Maintenance Of Remission In Ulcerative Colitis
Fish oil contains omega 3 fatty acids that may be beneficial in reducing inflammation, such as seen in the bowel of ulcerative colitis patients. Randomized placebo-controlled studies that evaluated the effect of daily intake of omega-3 fatty acids to maintain remission in ulcerative colitis were reviewed. Three studies were included of which none reported a reduction in the rate of disease relapse in comparison with placebo. When the studies were pooled for meta-analysis there was no benefit for omega 3 fatty acids. There were no serious side effects in any of the studies. None of the studies used enteric coated capsules which allow release of the fish oil in the small bowel. Non-enteric coated omega-3 fatty acids seem safe but ineffective for maintaining remission in ulcerative colitis. Further studies of enteric coated capsules may be justified.
No evidence was found that supports the use of omega 3 fatty acids for maintenance of remission in UC. Further studies using enteric coated capsules may be justified.
Omega-3 fatty acids have been shown to have anti-inflammatory properties. Therefore, n-3 therapy may be beneficial in chronic inflammatory disorders such as ulcerative colitis.
To systematically review the efficacy and safety of n-3 for maintaining remission in ulcerative colitis .
Also Check: Ozanimod Ulcerative Colitis Phase 3
Colonoscopy And Body Composition
The COLOVIEW mini-endoscopic system was used as previously described . Distal colon was examined along the first 34 cm. Scoring system consists in evaluation of ulceration numbers , vasculature features , mucosal granularity , erythema , pinpoints , fibrin deposition , length involved and overall vulnerability of the colon. Fat and lean body mass were measured with NMR the day before the sacrifice and expressed as% of animal body weight.
Read Also: Natural Home Remedies For Ulcers In Stomach In Tamil
What Is Uc Again And Why Does Diet Matter
If youre reading about UC and diet, you probably have some of the basics already down but just in case this is all new to you: Ulcerative colitis causes chronic inflammation in the colon and rectum, triggering frequent and urgent diarrhea, bloody stools, and abdominal pain and cramping.
Its not just a poop problem though. It can lead to nutrient deficiencies, actual malnutrition, and weight loss along with body-wide inflammation, which can spur joint pain, fatigue, and more. And these are all issues that can be influenced for better or worse by what you eat .
Whats tricky, though, is that theres no specific ulcerative colitis diet.
In fact, there isnt even a set list of trigger foods that applies to every single person with UC.
Just like everyones specific set of UC symptoms is unique, so too are their problem foods. So, what the heck are you supposed to do with that? Find yourself a guide, thats what.
The best way to figure out how to make your diet work for your UC is to seek the advice of a registered dietitian. Ask your gastroenterologist if they can refer you to an R.D. they trust.
In the meantime, get up to speed on which foods do commonly worsen symptoms in people with UC, along with what goes into a healthy diet in general. While you cant manage UC with diet alone, arming yourself with this knowledge can be a key piece of the puzzle.
Read Also: Can You Drink Alcohol If You Have Ulcerative Colitis
Recommended Reading: Snack Ideas For Ulcerative Colitis
Helper T Cell And Regulatory T Cell Characterization
Mesenteric lymph node cell suspensions were made to assess in AT mice Th1 and Th17 cells ex vivo as described previously . Th1 cells were CD4+IFN+ whereas Th17 cells were CD4+IL-17+. Additionally, anti-FoxP3 intranuclear staining was made in order to track the generation of so-called CD4+FoxP3+ regulatory T cells. All antibodies were purchased from eBiosciences.
You May Like: What Is Good For Mouth Ulcers
What To Eat On An Ulcerative Colitis Diet During A Flare:
Eating during an Ulcerative Colitis flare needs to be approached with caution. When you are in pain, feeling bloated, and just dont feel like eating, choose foods that are easy to digest.
-
Select refined grains. Refined grains are easier to digest than whole grains. So, select white bread, white rice, and white pasta. Yes, a dietitian is recommending you eat white grains! These foods are sources of B vitamins and Iron.
-
Choose low fiber vegetables and fruits. Low-fiber vegetables are well cooked or canned veggies, mashed potatoes without the skins, and string beans. Cooking veggies helps to break down the fiber. So, when you are flaring, avoid salads and other dishes with raw vegetables. Also, remove the skin from raw veggies and fruits and avoid produce that has seeds such as strawberries and raspberries. Low-fiber fruits are bananas or cantaloupes. For a nutrient-rich drink, reach for low-sodium vegetable juice.
-
Use unsaturated fats. Cook with small amounts of heart-healthy unsaturated oils. Try different oils to replace butter or stick margarine. Aim for a fat intake below 35% of your daily calorie intake. A low-fat diet may help to prevent bloating, cramping, and diarrhea.
-
Reach for calcium-rich foods. For example, low-fat dairy products , canned salmon, and soy products. Oat, soy, or rice drinks enriched with calcium are another option.
Recommended Reading: Is Soy Milk Good For Ulcerative Colitis
Also Check: What Does An Ulcer Feel Like In Your Stomach
What Foods Should I Not Eat When I Am Having An Ulcerative Colitis Flare
Certain foods can exacerbate or aggravate an UC flare and should be avoided. They are more likely to trigger cramping, bloating, and/or diarrhea and are also not recommended in people diagnosed with a stricture, which is a narrowing of the intestine caused by inflammation or scar tissue, or in those who have had recent surgery. Examples include:
- Foods high in insoluble fiber that are hard to digest, such as seeds, raw green vegetables , whole nuts, whole grains, or fruits with a skin
- Lactose, which is milk sugar found in dairy products, milk, cream, cream cheese, and soft cheeses
- Non-absorbable sugars such as sorbitol, mannitol, and other sugar alcohols that are typically found in sugar-free gum, candy, ice cream, and certain types of fruits and juices such as pear, peach, and prune juice
- Sugary foods such as candy, pastries, and juices
- High-fat foods such as butter or margarine, coconut oil, or fatty, fried, or greasy food
- Alcohol such as beer, wine, or spirits
- Caffeinated drinks such as coffee or energy drinks
Tips For Meal Prepping
Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
Read Also: Cheap Ulcer Treatment For Horses
Recommended Reading: How To Reduce Ulcer Pain
The Utility Of Pufas In The Management Of Ibd
The aetiology of IBD remains unclear but local mediators including arachidonic acid metabolites, cytokines and altered cell mediated immunity are likely to contribute to the disease. The rationale for the prescription of n-3 PUFA to promote a healthy gastrointestinal tract has been linked to their suggested anti-inflammatory properties. Different strategies have been adopted in various clinical trials to evaluate n-3 PUFA in patients with IBD. Inhibition of natural cytotoxicity, changes in interleukin 2 and arachidonic acid metabolites, e.g., LTB4 are the main chemotactic signals seen in the mucosa during a relapse. All are known to mediate the natural killer activity. A second hypothesis is based on the possible deficiency of essential fatty acids in IBD and its effect on cell membranes. A further possibility is that fish oil ameliorates oxidative stress in IBD.
In a randomised crossover trial from four units which involved 18 patients with ulcerative colitis fish oil supplements reduced LTB4 levels in a rectal dialysate. Histology improved and patients weight increased.
Conversely, a small Canadian trial of 11 patients found that addition of fish oil was of clinical benefit in UC but did not reduce mucosal LTB4. However, over a six month period serum LTB4 was insignificant while there was a simultaneous fall in NK cell cytotoxicity.
Fatty Acids In Diet Affect Ulcerative Colitis Risk
By Anne Harding, Reuters Health
3 Min Read
NEW YORK People who eat lots of red meat, cook with certain types of oil, and use some kinds of polyunsaturated fatty acid -heavy margarines may be increasing their risk of a painful inflammatory bowel disease, a study in more than 200,000 Europeans shows.
These foods are high in linoleic acid and the study have found that people who were the heaviest consumers of this omega-6 PUFA were more than twice as likely to develop ulcerative colitis as those who consumed the least.
Dr. Andrew Hart of the University of East Anglia in Norwich, UK, and his colleagues also found that eating more eicosapentaenoic acid, an omega-3 fatty acid found in fish and fish oils, was associated with a lower risk of the disease.
While people need a certain amount of linoleic acid to survive, Hart noted in an interview with Reuters Health, excess amounts are taken up into the lining of the colon, and if theyre released, they can promote inflammation. Omega-3 fatty acid, he added, does the opposite. It basically dampens down inflammation, he explained.
To investigate the role of fatty acids and ulcerative colitis, a life-long disease characterized by inflammation of the lining of the large intestine, Hart and his colleagues looked at data from the European Prospective Investigation into Cancer and Nutrition trial, which includes over half a million people from 10 European countries.
Recommended Reading: What Happens When You Have A Stomach Ulcer