Introduction And Scope Of The Problem
Patients with VLU have increased missed workdays, with 29% higher work-loss costs. However, a price on the burden endured by patients with VLU cannot be estimated when one takes into account the psychosocial impact with significant isolation, embarrassment, negative emotions, anxiety, depression, loss of self-worth, dependency, and sleep disturbance. The annual United States taxpayer burden for VLU is estimated at an astonishing cost of $14.9 billion .
Facts about venous leg ulcer.
The intention of this comprehensive review is to provide practitioners caring for patients with VLU with a foundation of information that will define causes of VLU and other ulcers that are less common that may be mistaken for VLU, the clinical manifestations of VLU, and delayed healing of and difficulty healing VLU that is common place in clinical practice and to provide pathophysiological molecular insights on important regulators and inflammatory mediators that are critical factors in propagating the VLU refractory state of continued inflammation, surgical treatments and innovations, and drug therapies that have evolved given our increased scientific discovery and knowledge that lead to better targeted therapies and finally with information on the means to prevent progression, occurrence, and recurrence of VLU.
What Is The Treatment For Leg Ulcers
Where possible, treatment aims to reverse the factors that have caused the ulcer. As an ulcer is often the result of both arterial and venous disease, careful assessment is needed first.
Venous leg ulcer, in the absence of arterial disease, is usually treated with exercise, elevation at rest, and compression. Compression must not be used if there is significant arterial disease, as it will aggravate an inadequate blood supply. Surgery, ultrasound-guided sclerotherapy or endovascular laser treatment of superficial and perforator leg veins may also help, particularly if the deep venous system is intact. Venous-return assisted calf compression devices may be of additional benefit.
A vascular surgeon should also assess patients with arterial leg ulcers as they may require surgery to relieve the narrowing of the arteries. Revascularisation is particularly important if the ABPI is less than 0.5.
It is also very important to treat underlying diseases such as diabetes and to stop smoking.
Symptoms Of Venous Insufficiency Ulcers
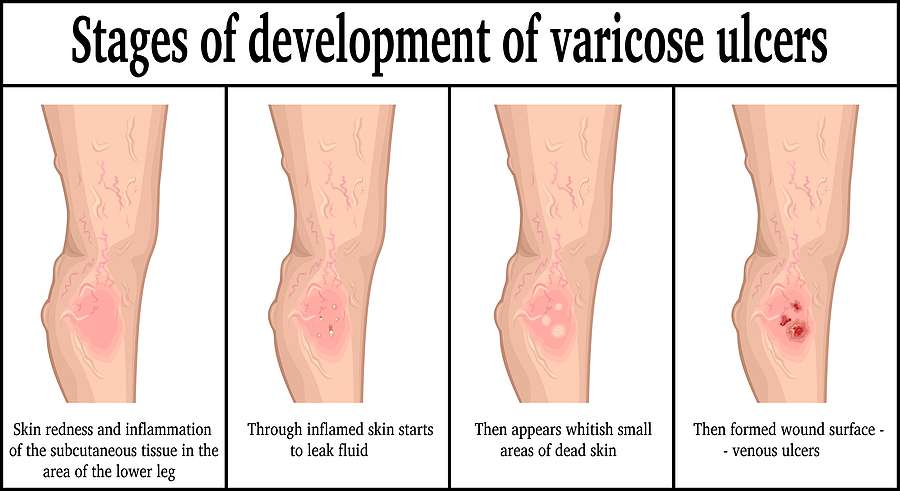
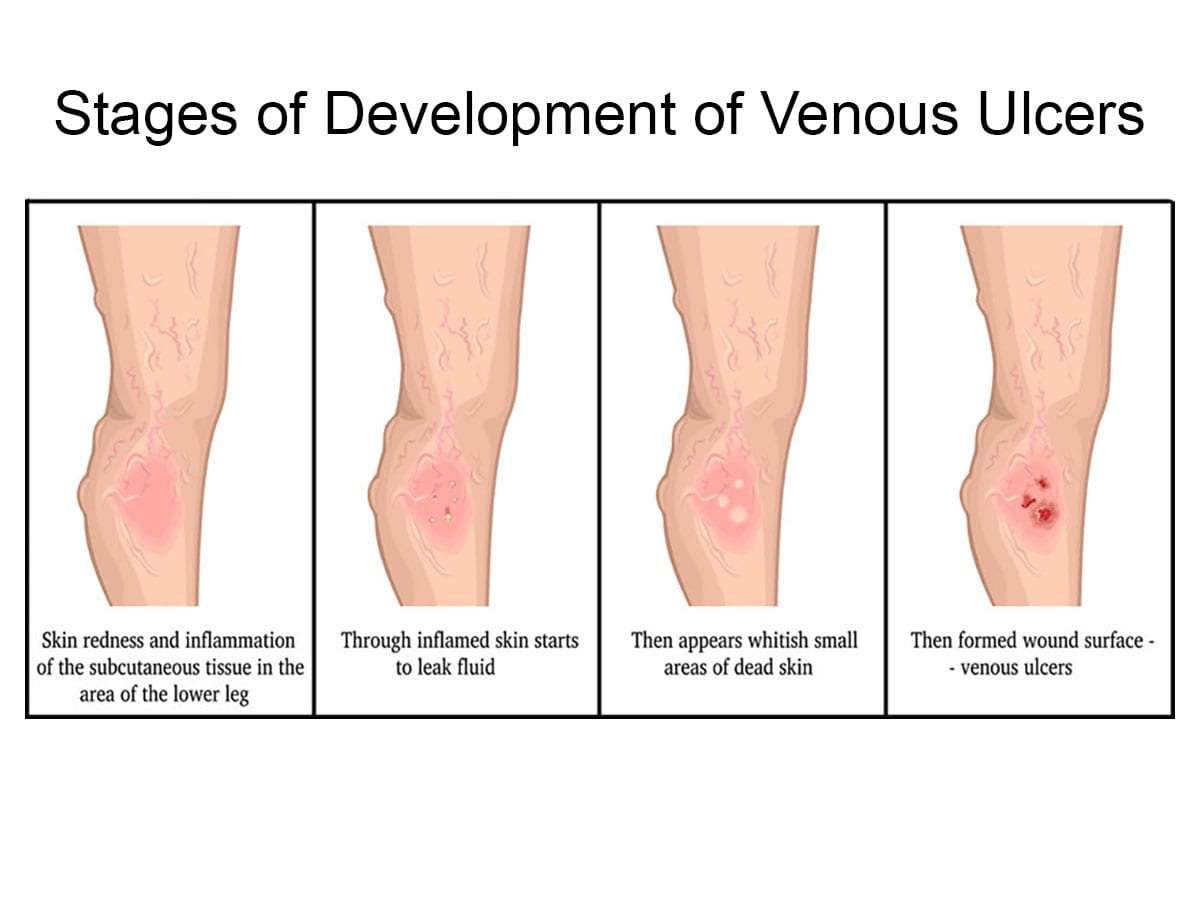
Whe a venous ulcer begins to develop, stasis dermatitis may be present causing scaling and erythema of the lower extremities. Hemosiderin staining may also occur, causing the presence of brownish or yellow patches underneath the skin. Other skin changes may include the appearance of dark red or purple as a result of blood leaching into the surrounding tissue. Venous ulcers will present with shallow but large wounds with irregular margins that typically develop on the lower leg or ankle. The base of the ulcer is typically red, can result in a significant amount of exudate depending on the level of infection, and will ooze venous blood when manipulated. Typically the wound will be relatively painless, with any pain resulting from subsequent infection or edema. Often the entire leg will become swollen, and the skin will become more firm and reddish brown in color, otherwise known as stasis dermatitis. Elevation of the limb will help to relieve discomfort and swelling.
Figure 1: Venous ulcer with obesity as cofactorFigure 2: Large superficial venous ulcer
You May Like: How To Treat Stage 4 Pressure Ulcer
What Are The Complications Of Leg Ulcers
People with nonhealing wounds are at risk for:
- Bone infections such as osteomyelitis, which may lead to limb loss .
- Cellulitis, a potentially severe bacterial infection of the skin and layers beneath the skin.
- , a potentially life-threatening bacterial infection.
- Skin cancers like squamous cell carcinoma.
What Types Of Venous Disease Cause Venous Stasis Ulcers
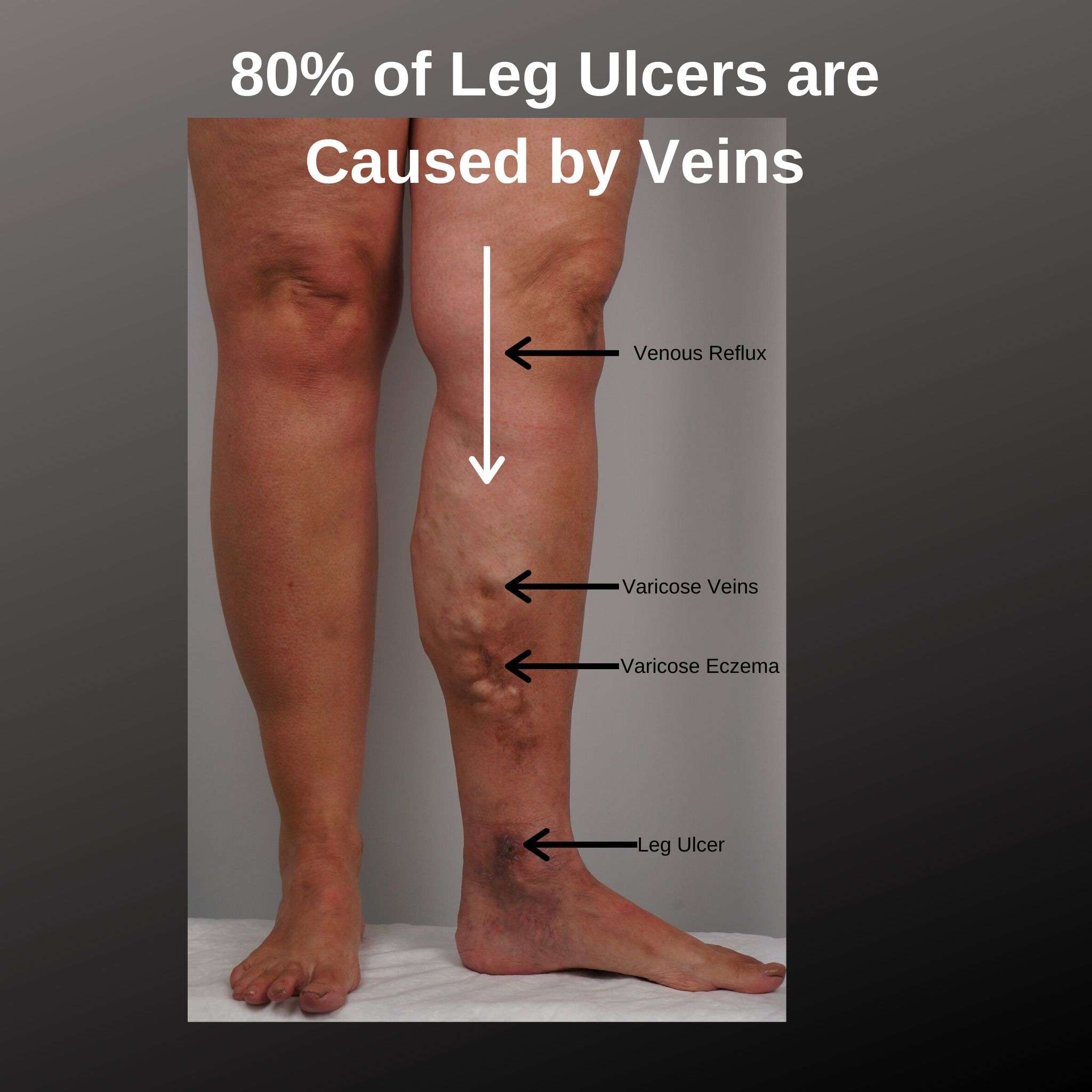
Chronic venous insufficiency is a common cause of valve dysfunction. It occurs when your valves are damaged or too weak to do their job.
Other venous ulcer causes include:
- High blood pressure , which damages blood vessel walls.
- Venous obstruction, a vein blockage thats sometimes due to blood clots.
- Venous reflux, when blood flows backward through weak or damaged valves.
Recommended Reading: Ulcer Signs Symptoms And Treatment
Do Not Hesitate Get Treatment
If you do suffer venous stasis ulcers, its critical that you get treatment immediately. Your doctor will clean the wound and may apply an antibiotic ointment to stave off an existing or potential infection. Other treatment options may include wearing of a special boot that helps to protect and more quickly heal the wound, time in a whirlpool, and ultrasound or physical therapy. While most patients respond well and heal with adequate wound care, extreme cases may require skin-grafting surgery.
It is very important to also treat the abnormal veins which caused the ulcer. If not the ulceration will usually reoccur.
If you have signs of venous statis ulcers, contact the St. Johns Vein Center at 877-640-VEIN and schedule a consultation today.
Dont Miss: Foam Dressing For Pressure Ulcer
How Should We Define Wound Infection
Virtually all open wounds are colonized with microorganisms, but this usually has no clinical consequences, because they show no evidence of infection and heal as expected . Some wounds are clearly infected they have purulent secretions or some of the cardinal manifestations of inflammation that have classically defined the host response to tissue damage caused by pathogenic and invasive microorganisms . The likelihood that a wound will become infected is related directly to the inoculum size and virulence of the colonizing organisms and inversely related to local and systemic host resistance . But some wounds occur in patients with neuropathy , ischemia , or venous insufficiency . Because these conditions limit the expression of inflammation, some define infection by secondary signs of local infection, . A Delphi approach by an international group of 54 wound care experts produced consensus on criteria they deemed common to infection in all chronic wounds: cellulitis, malodor, pain, delayed healing, deterioration or breakdown, and increased exudate . Some of these criteria have purportedly been validated by studies of various wounds in several settings, but the findings are limited by the fact that they compare the clinical criteria to inadequately validated microbiological definitions of infection . Furthermore, the additional evidence of infection likely varies for different types of chronic wounds .
Read Also: Best Foods To Eat When You Have A Stomach Ulcer
Implications For Future Practice
Improving venous ulcer care requires increasing nurse wound care knowledge across settings and ensuring nurses work at the top of their scope of practice. For example, barring exclusion from a states nursing practice act, training in debridement of venous ulcers can be taught to nurses in many settings to facilitate care outside of wound care centers. In addition, nurses and patients can use monofilament devices for mechanical debridement.
The Centers for Medicare & Medicaid Services has paved the way for using telehealth during the pandemic, making it an ongoing viable option for helping patients adhere to treatment recommendations. It can be used for patient and family education and to perform screening and monitoring visits, effectively reducing barriers to care.
For more complex patients, home health nurses should be trained in advanced wound care to help reduce gaps in care during times of crisis and for patients unable to visit a wound care center. In addition, in-person or virtual patient self-care education is vital to ensure proper venous ulcer management if in-office or home health visits arent possible.
Why Is It Important To Seek Venous Ulcer Treatment
Venous ulcers dont heal on their own. The longer you live with them, the greater the likelihood of permanent tissue damage. The damage can spread or cause infections that can become life- or limb-threatening, such as gangrene.
In severe cases, it may be necessary to surgically remove your affected limb. Timely care from an experienced wound care provider significantly lowers this risk.
Read Also: Medical Management Of Ulcerative Colitis
Why Are Diabetics At Risk
The risk of venous ulcers is much higher for diabetics. First, diabetes causes reduced circulation. Second, diabetic peripheral neuropathy can cause numbness in the feet.
If patients cannot feel when they have injured feet, they do not know they need treatment. Poor circulation makes wounds slow to heal, creating the perfect conditions for venous ulcers to develop in the feet and legs of diabetics.
What Do Stasis Ulcers Look Like
Stasis ulcers are commonly located on the lower legs, usually just above the ankles. They are shallow, open wounds with uneven borders, and they can vary in size and shape. The base of the sore will be red, sometimes with an overlay of yellow tissue. The surrounding skin may discolor , and it may also be shiny, tight, swollen, and warm to the touch. Often, the whole leg will become swollen.
Recommended Reading: Can Ulcerative Colitis Cause Back Pain
Don’t Miss: New Meds For Ulcerative Colitis
Signs And Symptoms Of Venous Ulcers
Symptoms may show up even before an ulcer forms, such as:
- Swelling, heaviness or cramping in the legs
- Hardening or thickening of the skin
- Dark red, purple or brown discoloration
Signs and symptoms of venous ulcers include:
- Sore on the inside of the leg or just above the ankle. The base of the wound is red and is sometimes covered by yellow tissue. The edges of the ulcer may be unevenly shaped.
- Skin around the wound is shiny, warm or hot, tight and discolored.
- Pain in the leg.
Venous Vs Arterial Ulcers
Before we dig into the causes, we are going to cover the difference between venous and arterial ulcers because they are two completely different things.
Arterial ulcers are due to a lack of blood flow the the skin caused by damage to the arteries. This is an extremely serious condition if left untreated could potentially result in an amputation.
And venous ulcers are a result of damage to the veins caused by a lack of blood from back up to the heart.
Thus, the causes of each ulcer type is different, and the prevention is different as well.
Read Also: How To Control Ulcerative Colitis
What Are Leg Ulcers
Leg ulcers are open wounds on your leg that take more than two weeks to heal despite treatment. These ulcers typically appear between the ankle and knee.
Leg ulcers often seep and can grow larger if left untreated. A sore on your leg that doesnt heal after three months of treatment is considered a chronic condition.
Definition And Etiology Of Venous Leg Ulcers
VLU can be defined as a full-thickness defect of the skin frequently seen in the ankle region that fails to heal spontaneously and is sustained by chronic venous disease . In more recent guidelines, a VLU is defined by best practice and uses the standard definition of an open skin lesion of the leg or foot that occurs in an area affected by venous hypertension .
Diagram representation of chronic venous disorder pathophysiology. GAG: glycosaminoglycans, MCP-1: monocyte chemoattractant protein, MIP-1: macrophage inflammatory protein, ICAM-1: intercellular adhesion molecule, VCAM-1: vascular cell adhesion molecule, NO: nitric oxide, Fe2+/Fe3+: ferrous/ferric ions, ROS: reactive oxygen species, NOS: nitrogen oxidative species, TAM: Tyro Axl MerTK receptor family tyrosine kinase, TLR: toll like receptors .
A clear understanding of inflammatory pathways allows for detailed understanding of the pathophysiology and for areas of research for treatment targets. In addition, there are significant metabolic changes that occur in the VLU cell and tissues, which affect cell function and potential for healing and also present systemically, indicating that metabolic changes are dynamic and opportunity for novel therapeutic targets .
Read Also: What Should I Eat With Ulcerative Colitis
How Should I Treat A Leg Infection
The most appropriate treatment for a leg infection depends on the particular type of infection. Some affect a persons skin cells while others may involve the bone or lymph nodes. If a person suspects he has an infected leg, he should see a doctor for a diagnosis and treatment recommendation. Some seemingly minor infections can become severe if left untreated or if theyre treated with the wrong types of medication.
One type of infection that may affect a persons leg is called cellulitis. This infection involves the cells right below the skins surface, causing inflammation in the affected area. It develops when the skin is broken, such as because of a cut, broken blister or animal bite. The broken skin allows bacteria to enter the body, which leads to the infection. There are many types of bacteria that cause cellulitis, but those in the strep family are the most common.
Oral antibiotics are usually used to treat a cellulitis leg infection and usually cure it within a week or so. A patient may return to his doctor after about a week to check whether it has gone away entirely. In a severe case, a person may need to be hospitalized and treated with intravenous antibiotics.
Dont Miss: Will Doctors Prescribe Antibiotics Over Phone
Caring For Venous Ulcers
Venous ulcers need proper care and treatment to prevent infection and to heal. It’s important to have any venous ulcers checked right away by your healthcare provider.
Treatment may require focusing on the circulatory or vein problems that are causing the ulcers. Or it may mean removing some tissue around the wound. You may be asked to:
-
Clean the wound regularly
-
Apply a dressing to the ulcer
-
Avoid products that cause skin sensitivity
-
Wear compression stockings to prevent blood from pooling in the legs and to speed healing
-
Apply an antibacterial ointment or another topical medicine to prevent or treat an infection
-
Take oral antibiotic medicines to prevent or treat an infection
-
Have allergy testing done
Wearing a compression wrap to keep blood flowing back up to your heart can also help ulcers heal more quickly. In some cases, surgery or a skin graft is needed to close up the opening in the skin.
You May Like: What Can I Take For A Stomach Ulcer
Chronic Leg Ulcers: Epidemiology Aetiopathogenesis And Management
Shubhangi Vinayak Agale
1Department of Pathology, Grant Govt Medical College, Byculla, Mumbai 400008, India
Academic Editor:
Abstract
Chronic leg ulcer is defined as a defect in the skin below the level of knee persisting for more than six weeks and shows no tendency to heal after three or more months. Chronic ulceration of the lower legs is a relatively common condition amongst adults, one that causes pain and social distress. The condition affects 1% of the adult population and 3.6% of people older than 65 years. Leg ulcers are debilitating and greatly reduce patients’ quality of life. The common causes are venous disease, arterial disease, and neuropathy. Less common causes are metabolic disorders, hematological disorders, and infective diseases. As many factors lead to chronic lower leg ulceration, an interdisciplinary approach to the systematic assessment of the patient is required, in order to ascertain the pathogenesis, definitive diagnosis, and optimal treatment. A correct diagnosis is essential to avoid inappropriate treatment that may cause deterioration of the wound, delay wound healing, or harm the patient. The researchers are inventing newer modalities of treatments for patients with chronic leg ulceration, so that they can have better quality life and reduction in personal financial burden.
1. Introduction
2. Epidemiology
3. Aetiopathogenesis
| Vascular |
4. Pathogenesis of Chronic Leg Ulcers
4.1. Venous Ulcers
4.2. Arterial Ulcers
4.3. Diabetic Foot Ulcer
Diagnosis Of Leg Ulcers
- examine the wound
- perform some tests to measure the blood flow in your lower leg, such as the ankle-brachial index. This test compares blood pressure readings taken at the ankle and at the arm using a device called a Doppler machine
- recommend an angiogram for an arterial ulcer, to find out if the artery needs surgery to clear the blockage.
Also Check: Best Treatment For Diabetic Foot Ulcer
Swelling In The Legs And Ankles
Venous leg ulcers are often accompanied by swelling of your feet and ankles , which is caused by fluid. This can be controlled by compression bandages.
Keeping your leg elevated whenever possible, ideally with your toes at the same level as your eyes, will also help ease swelling. You should put a suitcase, sofa cushion or foam wedge under the bottom of your mattress, to help keep your legs raised while you sleep.
You should also keep as active as possible and aim to continue with your normal activities. Regular exercise, such as a daily walk, will help reduce leg swelling. However, you should avoid standing or sitting still with your feet down. You should elevate your feet at least every hour.
The Old Understanding Of Venous Leg Ulcers
Until the 1980s, most doctors and nurses had a clear understanding of the difference between venous leg ulcers and varicose veins.
Unfortunately, it turned out that they were wrong!
When valves failed in the superficial veins, they swelled on the surface causing varicose veins.
They believed that the deep veins could not be treated and so the only way to treat venous leg ulcers was to wrap the leg in compression bandages and dressings.
They also believed that the superficial veins caused no inflammation. Although they could be treated by varicose vein surgery, there was no need to do so as varicose veins were only cosmetic.
They believed in only 2 systems of veins in the legs the deep and superficial systems. The deep veins were in the muscles. The superficial veins in the fat under the skin.
When valves failed in the deep veins, this resulted in inflammation at the ankles. After a time, this inflammation would accumulate until the ankles swelled, the skin turned brown and leg ulcers appeared.
It is a great pity that many doctors and nurses still believe this, as it is totally incorrect.
This error has resulted in patients with leg ulcers failing to get the right treatment and ending up in compression for years. It also resulted in patients with varicose veins being left untreated, deteriorating towards complications such as leg ulcers in the future.
Also Check: How Long Does A Ulcerative Colitis Flare Up Last