Is Manuka Honey Good For Ulcerative Colitis
You might have of people using Manuka honey as a natural home remedy for alleviating symptoms of ulcerative colitis.
The good news is, there is some reliable research behind this and lots of anecdotal evidence of people having success.
In this article well break down the causes of ulcerative colitis and the reasons why Manuka honey might be a useful remedy.
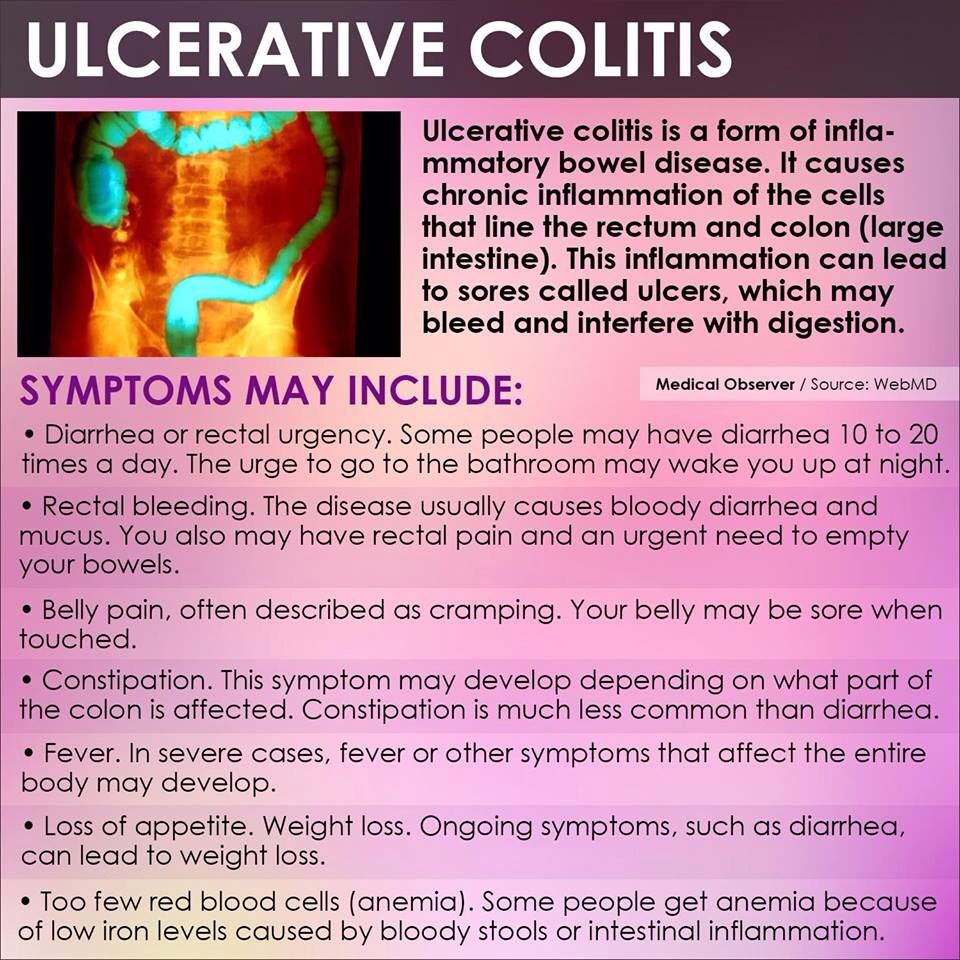
What Is Ulcerative Colitis
Though the root cause is unknown, Ulcerative Colitis is a common disease that affects the digestive tract by causing inflammation and sores in the lining of the large intestine and rectum.
As you can imagine, Ulcerative Colitis is an excruciating condition for many, and the hallmark of this disease is abdominal discomfort, which sometimes becomes a life-threatening condition.
According to the Mayo Clinic, depending on the extent of the inflammation and its location, the symptoms of Ulcerative Colitis can change.
Symptoms are often developed over time rather than coming on all at once.
Some warning signs and symptoms of ulcerative colitis include:
- Diarrhea, often with blood or pus
- Rectal bleeding passing a small amount of blood with stool
- Abdominal pain and cramping
- Inability to defecate despite urgency
- In children, failure to grow
While the range of individuals that Ulcerative Colitis affects is extensive, the disease itself only presents in a few forms.
There are four types of Ulcerative Colitis:
Often the symptoms of these variations are the same, so that the diagnosis will depend on a physicians expertise and medical examination.
Therapeutic Focus And Assessment
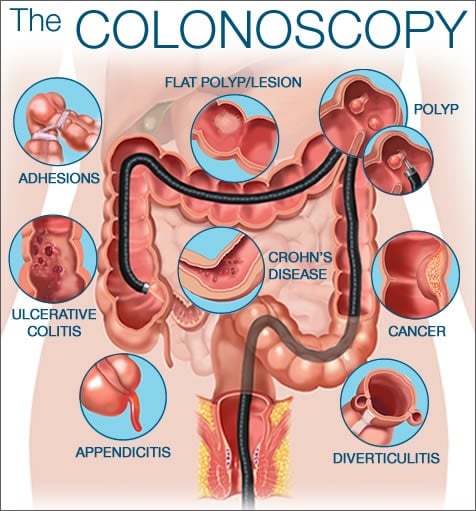
We initiated therapy with corticosteroids and 5-amino-salicylate derivatives , as well supportive treatment . The initial disease progression, within the first 2 weeks, was burdened by the presence of up to 11 bloody stools per day, prompting the patient to undergo multiple blood transfusions . After ~14 days of corticosteroid therapy, the patient’s condition started to progressively improve. We repeated colonoscopy after ~6 weeks , and we observed an improvement of the initial colonic lesions.
Figure 2. Aspect of the colon after 6 weeks.
You May Like: Fmt Treatment For Ulcerative Colitis Uk
What Are Nonsurgical Inflammatory Bowel Disease Treatments
IBD treatments vary depending on the particular type and symptoms. Medications can help control inflammation so you dont have symptoms . Medications to treat IBD include:
- Aminosalicylates minimize irritation to the intestines.
- Antibiotics treat infections and abscesses.
- Biologics interrupt signals from the immune system that cause inflammation.
- Corticosteroids, such as prednisone, keep the immune system in check and manage flares.
- Immunomodulators calm an overactive immune system.
You may also benefit from these over-the-counter IBD treatments:
- Antidiarrheal medication.
- Vitamins and supplements like probiotics.
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Read Also: Wound Vac For Pressure Ulcers
Don’t Miss: How To Treat Ulcer Pain
How Does Ulcerative Colitis Diet Work
When UC symptoms worsen, eating a temporary low-residue or low-fiber diet can occasionally assist. These eating plans aim to lessen how often and how many stools you pass.
You won’t need to go to the bathroom as frequently when there is less of this food debris in your intestines.
Eating foods that can easily flow through your intestines without creating too much irritation is a good choice if you’re attempting to decrease or prevent symptoms.
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohns disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Read Also: How Do You Get Ulcerative Colitis
Don’t Miss: What Causes Diarrhea In Ulcerative Colitis
Doctor’s Notes On Diverticulitis Vs Ulcerative Colitis
Diverticulosis and ulcerative colitis are conditions that both affect the digestive tract. Diverticulosis occurs when the inner layer of the digestive tract bulges through weak spots in the outer layer, forming small pouches in the wall of the digestive tract. When these diverticula become inflamed or infected, diverticulitis may develop.
Ulcerative colitis is a type of inflammatory bowel disease that is an acute or chronic inflammation of the innermost membrane that lines the colon and may result in the formation of sores .
Symptoms and signs of diverticulosis/diverticulitis and ulcerative colitis that are similar include
Symptoms of ulcerative colitis also include
- the urge to have a bowel movement,
- lack of appetite, and
What is the treatment for diverticulitis and ulcerative colitis?
The treatment for diverticulitis typically involves antibiotics and a liquid diet while the intestine heals. In severe cases, intravenous antibiotics may be required. Surgery is generally reserved for those with complicated or recurrent diverticulitis.
The treatment of ulcerative colitis may involve a combination of the following:
- Anti-inflammatory medications
- Biologic therapies that target proteins involved in the immune response
- Antidiarrheal medications or medications that reduce spasms in the intestine
- Surgery to remove part or all of the colon
What Are The Treatments Complications And Risk Of Cancer For Diverticular Disease Vs Ulcerative Colitis
Diverticular Disease Treatment
A high-fiber diet is the mainstay of diverticulosis and diverticulitis prevention.
- Start a high-fiber diet because it will decrease the risk of complications and the accompanying symptoms however, will not make the diverticula a person has gone away. Foods high in fiber include:
- Whole-grain cereals and bread
- Beans, peas, and lentils.
In the past patients with diverticulosis/diverticulitis were told that foods to avoid included seeds, corn, and nuts because it was thought fragments of these foods would get stuck in the diverticula and cause inflammation. However, current research has not found this to be the case, and the fiber content of such foods may benefit individuals with diverticulosis/diverticulitis. Discuss your diet or potential diet changes with your doctor.
Treatment for diverticulitis depends on the severity of the condition.
Treatment consists of IV or oral antibiotics, bowel rest, and possibly surgery.
If diverticulitis attacks are frequent or severe, the doctor may suggest surgery to remove a part of the patient’s colon.
- As with any surgery, there are risks the patient should discuss with his or her doctor.
- Sometimes the operation requires at least two separate surgeries on different occasions.
Complications
Recommended Reading: How To Self Treat An Ulcer
A Note About Sex And Gender
Sex and gender exist on spectrums. This article will use the terms male, female, or both to refer to sex assigned at birth. .
Small pouches called diverticula can form in the colon lining and push out through weak spots in the outer wall of the colon. If a person has diverticula in their colon, they have what health experts refer to as diverticulosis.
Diverticulitis is a condition where the diverticula become inflamed. Around 1025% of individuals with diverticulosis may have diverticulitis.
People may also use the term diverticular disease for diverticulitis or diverticular bleeding or if diverticula cause chronic symptoms.
Diet Management In Ulcerative Colitis
Its important to pay attention to what you eat if you have ulcerative colitis . Foods do not drive the condition, although they can induce flare-ups.
How can you avoid those triggers while still getting the nutrition you require? A nutrition plan can be beneficial in this situation. Here we discuss diet in Ulcerative Colitis, including what foods to eat and what foods to avoid.
You May Like: Venous Stasis Ulcer Treatment Dressings
What Questions Should I Ask My Healthcare Provider
You may want to ask your healthcare provider:
- What type of IBD do I have?
- Whats the best treatment for me?
- What foods or drinks should I avoid?
- What lifestyle changes should I make?
- Am I at risk for other problems?
- Should I look out for signs of complications?
A note from Cleveland Clinic
Most people with inflammatory bowel disease enjoy active lives. Still, symptoms of Crohns disease and ulcerative colitis can be life-disrupting. Some people go into remission after taking medications. Some people need surgery to deal with severe symptom flare-ups. Your healthcare provider can suggest dietary and lifestyle changes to manage IBD.
Last reviewed by a Cleveland Clinic medical professional on 05/03/2021.
References
Key Difference Colitis Vs Diverticulitis
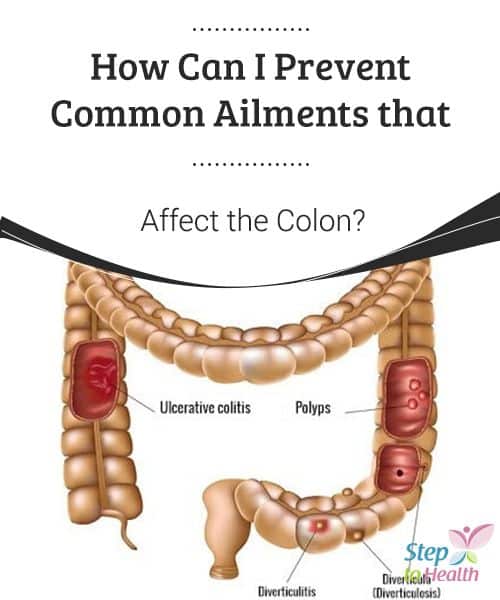
Colitis and diverticulitis are two inflammatory diseases of the colon that are difficult to be diagnosed solely based on the clinical features. The inflammation of the colon is known as colitis. Diverticulitis is the inflammation of the diverticula in the colon. As seen from the definitions, colitis is a condition that occurs in the colon whereas diverticulitis is a condition that takes place in the diverticula. This is the main difference between colitis and diverticulitis.
Read Also: Ulcerative Colitis Long Term Prognosis
Key Difference Diverticulitis Vs Ulcerative Colitis
In the medical jargon, the suffix itis is almost always used to describe something to do with inflammation. According to that preamble, you can understand that diverticulitis is the inflammation of the diverticula that arise from the colon. Ulcerative colitis, on the other hand, is the inflammation of the colon with the formation of associated ulcers. In ulcerative colitis, the overlying mucosa of the colon is inflamed, but in diverticulitis, it is the diverticulum arising from the colon that gets inflamed. This is the key difference between diverticulitis and ulcerative colitis.
Also Check: How Long Does An Ulcerative Colitis Flare Up Last
How Is Treatment The Same And Different
In both conditions, treatments usually involve medications or, sometimes, surgery. In severe cases, your doctor may recommend a combination of the two to bring your symptoms under control. Certain over-the-counter medications may ease some of your pain-related symptoms. These include:
- Anti-diarrheal medications
- Antispasmodics to ease cramps and bloating
- Iron supplements, especially if youâre bleeding
UC treatments may include:
Anti-inflammatory drugs. This is usually the first line of treatment. This can include drugs like 5-aminosalicylates and corticosteroids. Some newer drugs like sulfasalazine and 5-ASAs , which are called âsteroid-sparing,â can be safely taken long-term. Your doctor may not want you to take steroids long-term because of their side effects.
Immunosuppressant drugs. This helps to reduce inflammation in your colon and cut down the immune response that might attack your digestive cells.
Biologics. This targets the proteins made by your immune system.
Surgery. About 30% of people who have UC need surgery. Itâs sometimes the only cure, especially if medications donât ease your symptoms or they become too difficult to manage. Your doctor may consider a surgery called proctocolectomy.
In this procedure, your entire colon and rectum are removed. Most surgeries also involve a procedure in which your doctor will attach a pouch at the end of the small intestine or outside your body to pass poop directly into it.
Diverticulitis treatments may include:
You May Like: How To Heal Mouth Ulcers Quick
Oral Signs Of Crohn Disease
The oral mucosa is commonly affected in Crohn disease with up to one third of patients reported to have oral changes, and even higher in children. In some studies, the oral changes preceded the diagnosis of Crohn disease in 60%. There may be a male predominance.
1. Specific oral mucosal changes: orofacial Crohn disease
In children with Crohn disease, orofacial Crohn disease can be an important presentation preceding the bowel diagnosis.
2. Nonspecific changes in the mouth and surrounding facial skin associated with Crohn disease:
How Is Diverticulitis Diagnosed
If you are experiencing any of the symptoms of diverticulitis, your doctor will likely take the following actions:
- Gather information about your full medical history, including preexisting conditions and risk factors
- Examine your abdomen to check for tenderness
- Perform a rectal exam to check for rectal bleeding
- Perform a blood test to check your white blood cells and determine if you have an infection
- Order a diagnostic test to get a picture of your colon and determine if diverticula are present and whether they are inflamed or infected
The most common test used to diagnose diverticulitis is a CT scan. A CT scan uses both X-rays and computer technology to create three-dimensional images of your colon.
Don’t Miss: Immune Modifiers For Ulcerative Colitis
Main Differences Between Colitis And Diverticulitis
Difference Between Ulcerative Colitis And Diverticulitis Causes
As mentioned, the immune system is suspected to play a role in ulcerative colitis, along with genetics and environmental factors. Certain genes seem to be involved in the development of ulcerative colitis, and having more than four family members with this condition increases your risk of developing it, too. Environmental factors include place of residence, especially because there are higher rates of ulcerative colitis in urban areas, North America, and Western Europe. Air pollution, medications, and certain diets have also been found to be associated with a higher risk of ulcerative colitis.
Weak spots along the bottom of the large intestine can prompt the formation of diverticula. When pressure is added, bulges form. These bulges, or pouches, may protrude through the colon wall. When they burst or get infected, this marks the diagnosis of diverticulitis. It is worth noting that diverticula themselves do not necessarily create symptoms.
Read Also: Different Stages Of Pressure Ulcers
Difference Between Colitis And Diverticulitis
The difference between colitis and diverticulitis can be hard to distinguish as both cause similar abdominal pain. Colitis and diverticulitis are inflammatory diseases that can affect the colon and rectum in our large intestine. Though both the diseases show some similar symptoms, colitis causes inflammation of the colon whereas diverticulitis causes inflammation of the diverticula.
Read Also: Can I Eat Oatmeal With Ulcerative Colitis
What Causes Diverticular Disease Vs Ulcerative Colitis
Causes of Diverticular Disease
Diverticulosis is thought to be caused by increased pressure on the intestinal wall from inside the intestine.
- As the body ages, the outer layer of the intestinal wall thickens. This causes the open space inside the intestine to narrow. Stool moves more slowly through the colon, increasing the pressure.
- Hard stools, such as those produced by a diet low in fiber or slower stool transit time through the colon can further increase the pressure.
- Frequent, repeated straining during bowel movements also increases the pressure and contributes to the formation of diverticula.
Diverticulosis in developed countries is blamed largely on a diet low in fiber.
- Fiber is found in fruits and vegetables, whole grains, and legumes .
- There are two types of fiber soluble and insoluble.
- Soluble fiber forms a soft gel-like substance in the digestive tract.
- Insoluble fiber passes through the digestive tract nearly unchanged.
Causes of Ulcerative Colitis
The cause of ulcerative colitis is uncertain. Researchers believe that the bodys immune system reacts to a virus or bacteria, causing ongoing inflammation in the intestinal wall. Although UC is considered to be a problem with the immune system, some researchers believe that the immune reaction may be the result, not the cause, of ulcerative colitis.
Don’t Miss: What Are The First Signs Of A Stomach Ulcer
What Are Surgical Treatments For Crohns Disease
As many as 7 in 10 people with Crohns disease eventually need surgery when medications no longer provide symptom relief. During a bowel resection, a surgeon:
- Removes the diseased bowel segment.
- Connects the two ends of the healthy bowel together .
After surgery, the remaining part of the bowel adapts and functions as it did before. Approximately 6 in 10 people who undergo surgery for Crohns disease will have a recurrence within 10 years. Another bowel resection may be a good option for you.
When To See A Doctor
Schedule a doctors visit, Mayo Clinic suggests, if you have these symptoms of colitis:
- Diarrhea that continues even after you treat it with over-the-counter drugs
- Diarrhea that wakes you up
- A fever that lasts for more than a day or two without explanation
Schedule a doctors visit if you have these symptoms of diverticulitis: Continuous abdominal tenderness or pain without an obvious reason, especially if you also have a fever and constipation or diarrhea.
Keep in mind that any unusual signs should prompt a visit to your doctor. Dont try to diagnose these conditions on your own, warns Dr. Stollman.
Dont Miss: How To Check A Horse For Ulcers
Don’t Miss: Best Dressing For Stage 2 Pressure Ulcer On Buttocks