Colon Cancer And Ulcerative Colitis
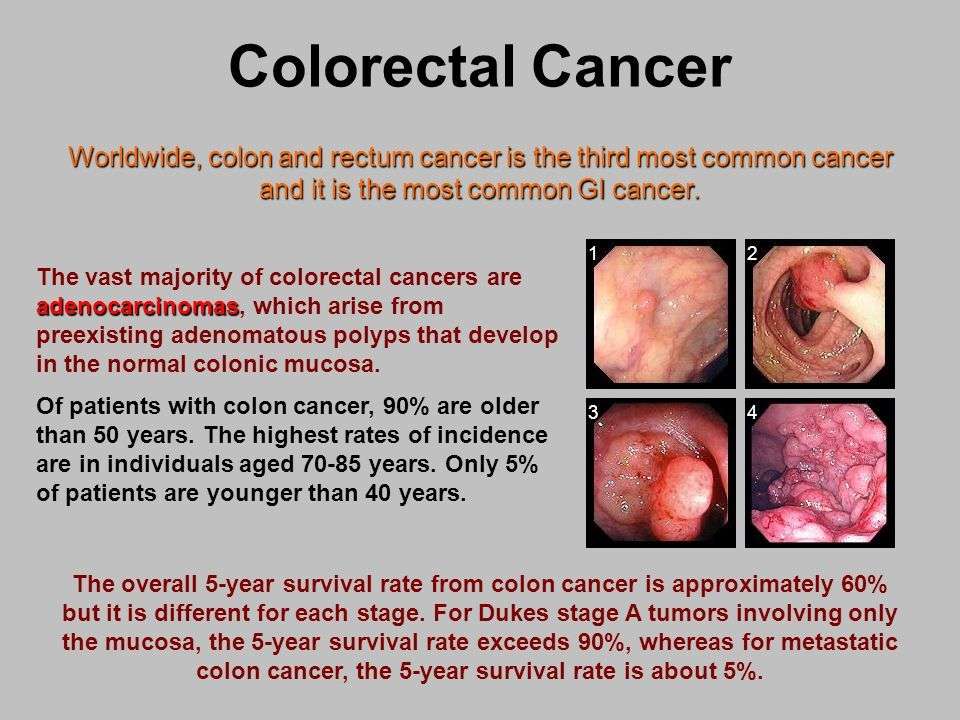
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you don’t get treatment for UC. That’s because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if you’ve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesn’t go away.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member who’s had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think it’s because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
How Ulcerative Colitis Is Treated
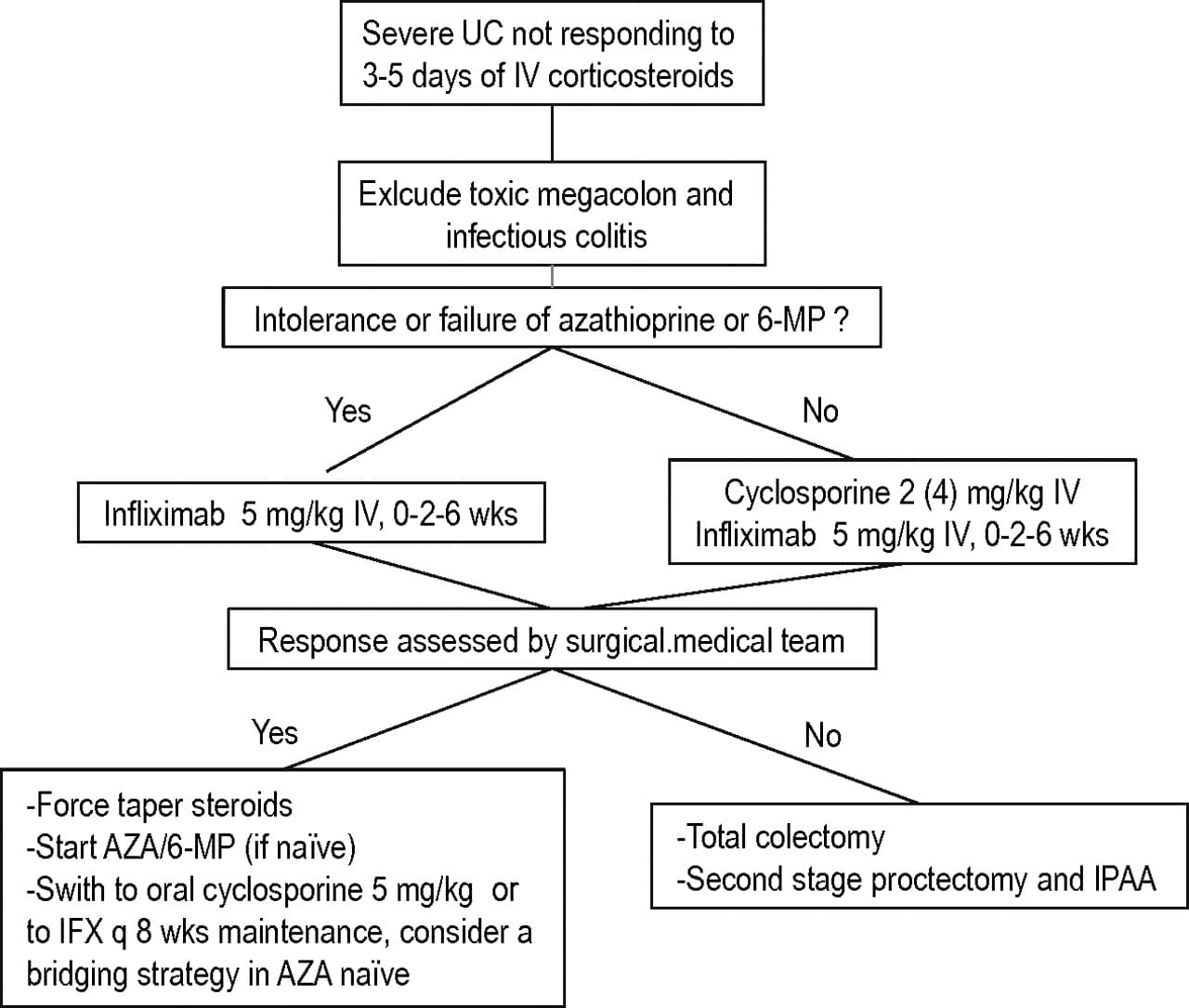
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
Response Rate And Patient Backgrounds
Ninety UC patients with moderate to severe activity received CAP therapy . Of the 90 patients, 44 patients achieved remission, 14 patients had effect, and 32 patients had no effect. According to this result, we decided input and outcomes . We divided the entire data in to training data set for generating predictive expressions and validation data set as detailed in method, generated the predictive expressions to predict the requirement of operation after CAP therapy from 13 input factors.
Read Also: What Can You Put On Mouth Ulcers
Diagnosis Of Ulcerative Colitis
X-rays of the abdomen taken after barium is given by enema do not require any special preparation . These x-rays usually can show a blockage or paralysis… read more ) may indicate the severity and extent of the disease but are not done when the disease is active, such as during a flare-up, because of the risk of causing a perforation. Other x-rays of the abdomen may also be taken.
Identification Of Factors Associated With Long
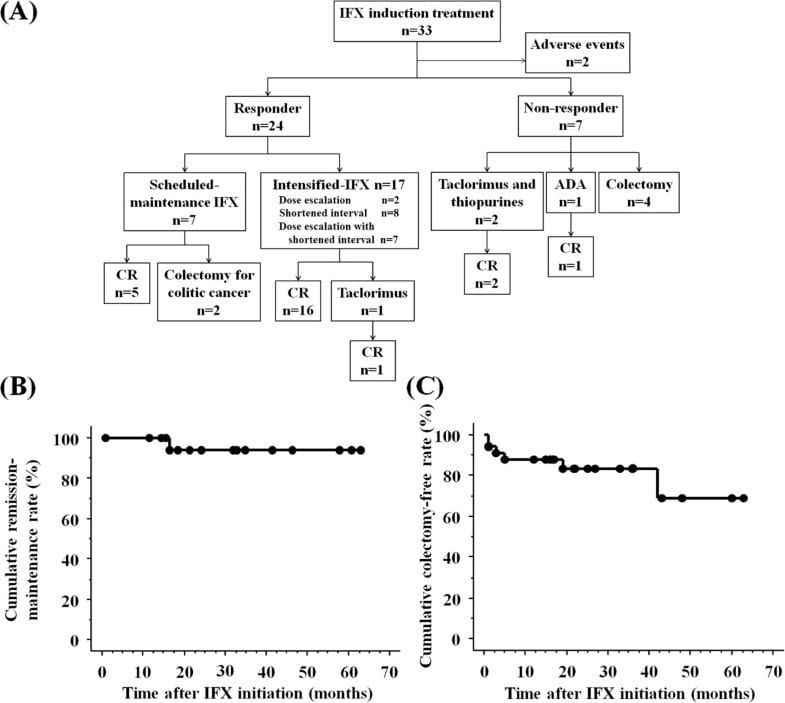
The association between clinical factors and long-term prognosis was analyzed using a log-rank test. The investigated clinical factors were sex age at diagnosis disease location family history of IBD smoking history use of topical 5-ASA response to steroid, thiopurine, and leukocytapheresis therapy use of new therapeutic agents, including tacrolimus, infliximab, adalimumab, golimumab, tofacitinib, and vedolizumab and drug-free remission. The cutoff for age at diagnosis was 30 years, which was the median age of the study participants. A multivariate analysis was performed using Coxs proportional hazard model to identify independent risk factors for colectomy.
Don’t Miss: What Do You Do For A Bleeding Ulcer
Relative Weights Of Input Factors Analysis
The detail of relative weights of input factors analysis were described elsewhere . In brief, we analysed relative weights of input factors using a leave-one-input-factor-out in turn with a missing values substitution procedure, which enables predictions to be made in the absence of values for each causal factor, and then assessed effects upon ANN response error. Root mean square error is an estimate of the typical difference between the predicted and actual values of outcomes. The smaller RMSE is the better prediction accuracy of the models. The network original error was accumulated as RMSEoriginal and the network was again used with LOFO data and the error RMSELOFO was estimated. Then, the relative weights of input factors was calculated as RMSELOFO/RMSEoriginal.
Ulcerative Colitis Life Expectancy
Thanks to improved medical treatment, people with ulcerative colitis are no more likely to die early than people who do not have ulcerative colitis. Appropriate diagnosis and treatment help many people with ulcerative colitis live long lives.
Talk to your doctor about your individual condition and how you can best combine treatment and lifestyle changes to manage your ulcerative colitis for many years to come.
Read Also: Latest Research On Ulcerative Colitis
Many Factors Shape How People With Inflammatory Bowel Diseases Fare
Crohns disease and ulcerative colitis are two forms of inflammatory bowel disease . These conditions are considered immune-mediated, which means that they involve the immune system. There is a genetic component to IBD as wellhundreds of genes have been found which may be connected to IBD. These conditions last throughout your lifetime, although symptoms will come and go. There is no cure for any form of IBD, but it is often well-managed through medications, surgery, and complementary therapies. This raises questions for many people who are diagnosed with IBD as to how the disease may affect them during their lives.
Input Factors And Outcome
We used the clinical data to determine input factors X1X13, which were used to predict the outcomes of individual patients using ANN analysis . X1 and X2 represented the patients age and gender, respectively. X3 represented the type of CAP and X4X6 represented the disease extent, duration and clinical type, respectively. X7 and X8 represented the CAI before and after CAP respectively. X9 and X10 represented medication . X11X13 represented the history of admission, PSL, operation, respectively. The outcome was requirement of operation after CAP therapy.
Don’t Miss: Do Ulcers Give You Diarrhea
Clinical Characteristics At Diagnosis
Among the 2802 patients in the study cohort, 1507 were men and 1295 were women, yielding a male-to-female ratio of 1.2:1. The median age at diagnosis of UC was 36 years . The demographic and clinical characteristics of the patients are shown in . The proportion of men , the median age at diagnosis , the proportion of ever smokers at diagnosis , and the proportion of proctitis at diagnosis increased significantly from cohort 1 to cohort 3, whereas a family history of IBD decreased significantly from cohort 1 to cohort 3. In the inception cohort, there were no differences between the three temporal cohorts in terms of disease extent at diagnosis or disease activity at diagnosis .
Demographic and clinical characteristics of 2802 Korean patients with ulcerative colitis according to the year of diagnosis.
| . |
|---|
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Also Check: Symptoms Of Crohn’s Vs Ulcerative Colitis
Recurring Or Severe Symptoms Of Ulcerative Colitis
Doctors examine people when their typical symptoms return, but they do not always do tests. If symptoms have been more frequent or longer-lasting than usual, doctors may do sigmoidoscopy or colonoscopy and a blood count. Doctors may do other tests to look for infection or parasites.
When symptoms are severe, people are hospitalized. Doctors take x-rays to look for a dilated or perforated intestine.
Ulcerative Colitis: Prognosis And Life Expectancy
Ulcerative colitis is a chronic inflammatory bowel disease that can be mild, moderate or severe. Its impossible to predict how the disease will affect an individual because lifestyle, access to medical care, and overall health status all affect the progression of this common condition. With appropriate treatment, most people with ulcerative colitis will experience symptom-free periods of remission and periodic symptom flares.
There is no cure for ulcerative colitis, but many people with ulcerative colitis live satisfying lives.
You May Like: What Causes Ulcers In The Colon
Past History Of Admission And Operation Non
We next attempted to identify factors that critically correlate to the outcome in ANN by using the relative weights of input factors analysis . This analysis involves determining how the result changes when the test factor is excluded. An Xtest value greater than 1 indicates that it improves the expression, and a value less than 1 indicates that it does not improve the expression. We analysed all expressions and determined the corresponding means and standard deviations. As shown in Fig 1, X13 and X11 were defined as significant predictive factors in every trial.
Data are expressed as the mean±SD for member networks.
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Also Check: Ulcer On White Of Eye
Is Ulcerative Colitis Curable
Ulcerative colitis can differ from person to person, but its usually a lifelong condition. Symptoms come and go over time.
Youll have flare-ups of symptoms, followed by symptom-free periods called remissions. Some people go years without any symptoms. Others experience flare-ups more often.
Overall, about half of people with ulcerative colitis will have relapses, even if theyre being treated.
Youll have the best outlook if the inflammation is only in a small area of your colon. Ulcerative colitis that spreads can be more severe and harder to treat.
The one way to cure ulcerative colitis is with surgery to remove your colon and rectum. This is called proctocolectomy. Once your colon and rectum are removed, youll also be at lower risk for complications like colon cancer.
You can improve your own outlook by taking good care of your ulcerative colitis and getting regular checkups to look for complications. Once youve had ulcerative colitis for about eight years, youll also need to start having regular colonoscopies for colon cancer surveillance.
It can be helpful to talk to others who understand what youre going through. IBD Healthline is a free app that connects you with others living with ulcerative colitis through one-on-one messaging and live group chats, while also providing access to expert-approved information on managing the condition. Download the app for iPhone or Android.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Also Check: Honey Dressings For Leg Ulcers
Outcome Of Patients With Disease Progression
In terms of steroid utilization, 47 patients with disease extension had used steroid, compared to 120 patients without disease extension . The cumulative rate of steroid use in extenders was 28.2, 39.0, 43.6, 48.9 and 59.7% in the first 5-year post-diagnosis. In the non-extenders, the corresponding rates of steroid use were 22.9, 28.3, 32.4, 36.8 and 40.8%, respectively . During the follow-up, 27 of the 91 extenders were steroid -dependent compared with 36 of 120 patients without disease extension. The incidence of steroid -dependence were 6.5, 35.1, 43.3, 46.3 and 52.3% in the group of patients with disease extension during the first 5-year post-diagnosis, compared to that of 12.6, 21.0, 29.3, 31.2 and 36.2% in patients without disease extension .
Table 3 The outcomes between patients with and without disease extension during follow-upFig. 4
Cumulative rate of a) steroid utilization, and b) immunosuppressive agents use in patients with and without disease progression. Time to event was calculated from the date of index endoscopy evaluation to the date of steroids or IMM use or censoring . KaplanMeier estimates were used to draw the cumulative incidence curves, compared by log-rank tests.
Two of the 91 extenders underwent colonic resection, compared to 5 in 427 non-extenders. There was no significant difference in the cumulative rate of colectomy between the two groups .
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
Also Check: Over The Counter Medication For Ulcerative Colitis
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Recommended Reading: Is Papaya Good For Ulcerative Colitis
Effects Of The First Course Of Cap
One hundred fourteen patients with UC received CAP therapy. Ninety patients followed for more than 3 years after the first CAP course with full clinical data were enrolled for further analysis . Following the first course of CAP, 58 patients showed clinical improvement and 44 of these 58 patients achieved clinical remission . The duration of the disease correlated significantly with the therapeutic effects of CAP CAP therapy was most effective in patients with a longer disease duration . Other factors such as age, sex, disease extent, clinical type, CAI at the start of the study, and use of PSL and IM before the study had little effect on the response to therapy .
Association Between Genotype And Long
We identified the SNP rs117506082 in 87 patients. The characteristics of these patients are shown in Table 6. There were significant differences in disease location and time from diagnosis to colectomy between the groups with the GG + GA and AA genotype . The GG + GA group tended to have less extensive disease and a longer time to surgery.
Table 6.
Clinical characteristics of the study population based on the rs117506082 genotype
The rate of use of therapeutic agents was significantly higher, and surgery-free survival was significantly lower in the AA group . The results of the multivariate analysis using Coxs proportional hazard model showed that the AA genotype was a significant independent risk factor for the need for therapeutic agents .
Table 7.
Summary of association between the rs117506082 genotype and long-term outcomes
Fig. 5.
Rate of use of new therapeutic agents and surgery-free survival according to rs117506082 genotype. a The rate of use of new therapeutic agents was significantly higher in the AA genotype group . b Surgery-free survival was significantly lower in the AA genotype group .
Also Check: Medicines Used To Treat Ulcerative Colitis
When To See A Doctor
Anyone with symptoms of ulcerative colitis should see a medical professional for an evaluation.
Individuals who already have a diagnosis of ulcerative colitis should see a doctor if symptoms become worse. This development could be the sign of a flare-up, and appropriate treatment can help control inflammation.
People may want to consider seeking emergency assistance if symptoms are sudden and severe.
Doctors can prescribe a range of medications to treat people with ulcerative colitis. Treatment aims to relieve symptoms and induce and maintain remission.
Available treatment options for ulcerative colitis can include:
Lifestyle changes may also help a person better manage their ulcerative colitis. For instance, suggests that a low-fat diet with plenty of vegetables may reduce the risk of developing ulcerative colitis.
Lifestyle modifications that may help a person manage their symptoms include:
- drinking more liquids but avoiding sodas and other fizzy drinks
- replacing large meals with smaller, more frequent ones
- using a journal to track foods that may trigger flare-ups
- limiting high-fiber and high-fat foods, during flare-ups