Figuring Out Which Foods Trigger Flare
As the NIDDK explains, although ulcerative colitis isnt caused by diet or nutrition, certain foods can trigger the symptoms or make them worse in some people. The tricky part is figuring out which ones.
Common ulcerative colitis triggers include dairy, high-fiber foods like fruit, vegetables, and whole grains, spicy foods, alcohol, and caffeine, according to the Mayo Clinic. That said, its really individual. Sam has always loved food and says that when it comes to what she can eat now, I have not figured that aspect out. And its not for lack of trying. I feel like I’ve done everything! she tells SELF, explaining that she tries to avoid various food groups like dairy that can trigger symptoms. It doesn’t mean I don’t ever eat them, but I try to avoid them, she says. I’m definitely still experimenting.
Stacey Bader Curry, 48, was diagnosed with ulcerative colitis in March 2020 and is concerned about giving up foods she loves, as well as alcohol and coffee. I’m trying to focus on what I can eat and not what I can’t eat, she says.
To figure out whether certain foods might be triggering your symptoms, the NIDDK recommends keeping a food diary where you record everything you eat and any flare-ups to help you work out what your dietary triggers could be.
Things No One Tells You About Life With Ulcerative Colitis
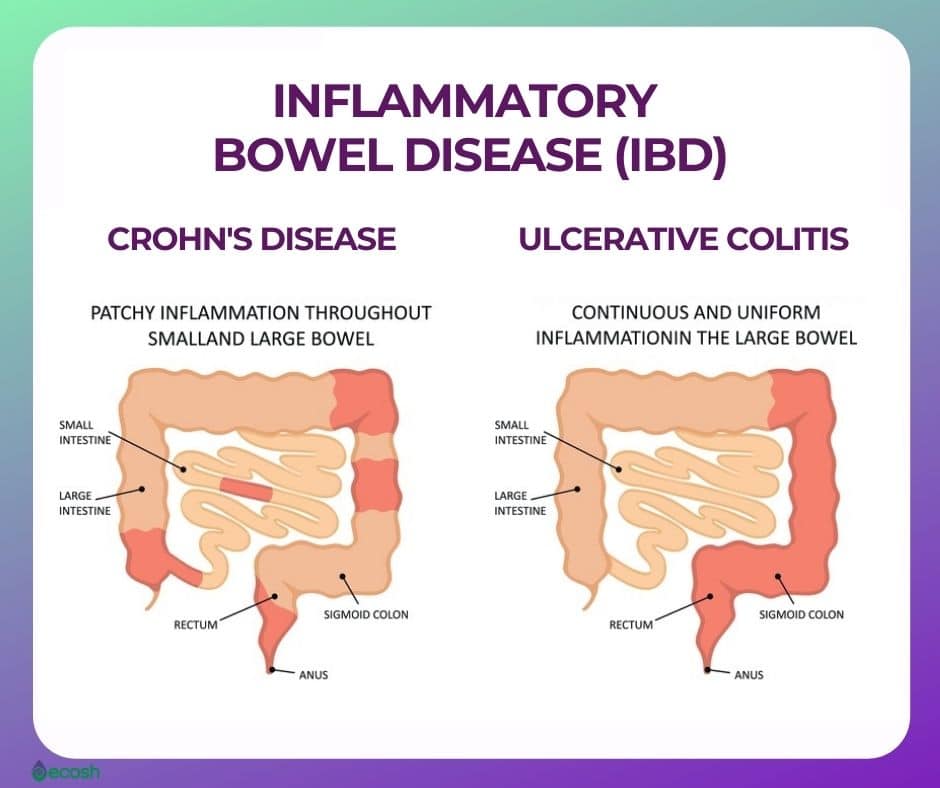
People who have never experienced ulcerative colitis may think it means getting the occasional bad stomachache or having a fussy gastrointestinal system. But as anyone with ulcerative colitis knows, the effects of this inflammatory bowel diseasein which sections of the large intestine develop inflammation and ulcerscan be severe and disrupt many aspects of your life. After a diagnosis of ulcerative colitis, it can be incredibly hard to navigate the reality of your new normal. Knowing the following seven facts about life with ulcerative colitis might help make the whole experience a little bit easier.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Read Also: Ulcerative Colitis Caused By Bacteria
Not Everyone Will Understand The Intensity Of Your Disease
Although ulcerative colitis can affect many aspects of your physical health, its often considered an invisible illness. Depending on the severity of symptoms on a given day, people with the condition can often still move around without any obvious signs that theyre in pain or discomfort. It puts a lot of pressure on your shoulders when you are chronically ill and it’s not visible, because you have to explain yourself time and time again, Skomski says. And since people between the ages of 15 and 30 are one of the more at-risk age groups for developing ulcerative colitis, people with the condition are sometimes perceived as too young to be sick.
People may also have a hard time wrapping their head around the pretty major lifestyle adjustments you might have to make with ulcerative colitis. My lifestyle’s not like a typical 20-something, Sam says. I think a lot of my friends see this as the intense period of their life: staying up all night, going to concerts that go until the middle of the night, going to bars, things like that. And I just can’t.
The Best Foods To Eat If You Have Ulcerative Colitis Or Crohns Disease
If you have ulcerative colitis, it is possible that a variety of foods, such as spinach, bananas, chickpeas, smooth nut butters, melons, and low-fiber breads and cereals, will improve your gut health. Many of these foods, in addition to helping you with your ulcerative colitis symptoms, have been found to be relatively simple to digest on your own. When you have Crohns disease, you may want to avoid whole grain or whole wheat cereals with high fiber content. Nonetheless, there are cereals with low amounts of fiber that are ideal for meeting your nutritional requirements.
Also Check: Infected Leg Ulcers In The Elderly
You May Like: Signs I Have A Stomach Ulcer
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Follow Up With Your Doctor
You may only need at-home or short-term care for some kinds of colitis. But UC is a condition youâll have for the rest of your life. And it affects everyone in a different way. Youâll need to work with your doctor to find a treatment plan that works for you.
No matter whatâs causing your symptoms, get medical care right away if you have:
- Watery diarrhea for more than a few days
- Heavy, ongoing diarrhea
Also Check: How To Treat Skin Ulcer On Leg
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
How Is Ulcerative Colitis Diagnosed
Colitis shares many symptoms with other common conditions, such as Crohns disease, irritable bowel syndrome, gastroenteritis and coeliac disease. Your doctor will examine you and take a detailed history of your symptoms to help rule these out.
There is no single test that can be used to diagnose UC, so a combination of tests is usually required:
- Blood tests help to rule out other medical conditions, and certain markers in the blood can indicate that inflammation is present.
- A stool sample may find other possible causes of diarrhoea and inflammation, such as an infection.
- A colonoscopy may be performed, where a thin, flexible tube that contains a tiny camera looks inside the bowel for ulcers, inflammation and bleeding.
- A biopsy may be taken from inside the bowel so a pathologist can examine it under a microscope to look for signs of disease.
Other types of imaging are sometimes used to help in the diagnosis and to help rule out other diseases.
Read Also: How To Remove Mouth Ulcer
The Intensity Of Your Symptoms Might Vary Over Time
The most common ulcerative colitis symptoms are diarrhea containing blood or pus and abdominal pain, the National Institute of Diabetes and Digestive and Kidney Diseases says. Theres a lot of cramping, Cristal Steuer, 38, who was diagnosed with ulcerative colitis while she was in college, tells SELF. You might also experience things like fatigue, fevers, nausea, unintended weight loss, joint pain, and rashes. Whichever symptoms you do have, they may wax and wane, the NIDDK explains. You may have periods when youre in remission interspersed with periods when your symptoms are worse. But some people experience constant symptoms from ulcerative colitis.
Just because you can’t see it doesn’t mean that it’s not hard every single day, Tatiana Skomski, 26, who was diagnosed at 21 after years of unexplained fatigue and pain when an especially bad flare-up nearly caused her to bleed to death, tells SELF.
I’ve had to increase my tolerance for what is a background level of pain, Sam, 22, who was diagnosed with ulcerative colitis in the summer of 2019, tells SELF. I’ll have sharper moments where I can’t functionbut for the most part, it’s more like a constant level of chronic pain.
If pain or other ulcerative colitis symptoms are really interfering with your life, make sure your health care provider knows so that you might be able to tweak your treatment plan if necessary.
Diet And Ulcerative Colitis Flare
If you are dealing with a flare-up, you may not have an appetite or know what you can safely eat. Here are some general guidelines.
Avoid potential trigger foods:
- Alcohol and caffeine.
- High-fat foods.
- Insoluble fiber, which is contained in foods like fruits with skins, raw green vegetables , whole nuts, and whole grains.
- Lactose, a sugar that can be found in dairy products.
- Non-absorbable sugars: Sorbitol, mannitol, and other sugar alcohols that can be found in low- or no-sugar products.
Try eating easily-digested foods:
- Low-fiber fruits, like bananas, cantaloupe, honeydew melon, and cooked fruits.
- Lean protein like fish, lean cuts of pork, white meat poultry, soy, and eggs.
- Refined grains found in sourdough or white bread, potato or gluten-free bread, white pasta, white rice, and oatmeal.
- Peeled, low fiber vegetables, like potatoes, cucumbers , and squash.
If you are having a flare-up, be sure to talk to your healthcare team. They can help you come up with both a diet and a treatment plan.
Don’t Miss: Infusion Therapy For Ulcerative Colitis
How Are Ulcerative Colitis And Colitis Different
A key difference is what triggers colitis. For instance, IBD is usually an autoimmune issue. Thatâs when your immune system attacks healthy tissue in your body. Other kinds of colitis can be the result of outside factors, such as germs or medical treatments.
People with UC or other kinds of IBD may also have inflammatory symptoms alongside bowel problems, including:
But those arenât the only distinctions. Hereâs a breakdown by colitis type:
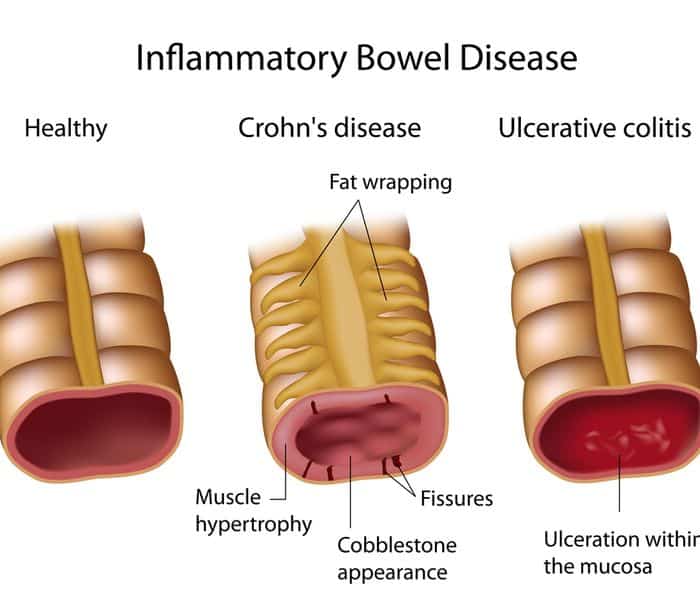
Ulcerative colitis . This type of IBD causes sores and constant inflammation in the inner lining of your large intestine. UC often starts in the rectum and extends through the left side of your colon. But some people have colitis throughout most or all of their colon. Thatâs called extensive colitis or pancolitis.
Crohnâs colitis. This is a feature of Crohnâs disease, another type of IBD. Crohnâs can impact any part of your gastrointestinal tract â thatâs your mouth to your . Unlike UC, you may have healthy tissue in between spots of inflammation. Crohnâs disease can also affect many layers of your GI tract.
Microscopic colitis. This is another type of IBD. Itâs not related to ulcerative colitis or Crohnâs disease, but itâs associated with other autoimmune diseases. Like the name suggests, your doctor has to use a microscope to see any evidence of this kind of colitis.
There are two main forms:
Some experts think collagenous and lymphocytic colitis may be different phases of the same condition.
Tips For Healthy Ulcerative Colitis Poop
There are several different approaches to UC treatment. Medications, diet, and other lifestyle changes can all help improve bowel symptoms in UC.
The foremost treatment for ulcerative colitis inflammation and related stool changes is medication. These include:
- Aminosalicylates such as Asacol or Azulfidine , to reduce inflammation
- Corticosteroids such as prednisone and Entocort EC , to reduce inflammation
- Immunomodulators such as Imuran or cyclosporine, to reduce your immune system response
- Biologic therapies such as Remicade or Simponi , to neutralize proteins made by the immune system and reduce inflammation
Your diet also plays a role in your bowel habits. After all, what goes in, must go through and come out. The following diet modifications may help reduce bowel symptoms:
- Avoid your individual trigger foods.
- Limit dairy products.
- Drink plenty of water throughout the day.
- Eat small meals.
Stress is another factor that can contribute to changes in the stool. The brain-gut connection may play a role in inflammation of the GI tract. Managing your stress levels might be able to decrease diarrhea and other changes in your stool.
In addition, participating in regular physical activity is healthy for the GI tract. Exercise helps with the movement of stools, which can be especially helpful for constipation.
Don’t Miss: Ulcer Points On A Horse
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK
Also Check: Liquid Diet For Ulcerative Colitis
Black Cumin Prevents Lung Inflammation
Black Cumin has been shown to reduce oxidative stress and inflammation. In one study, Nigella sativas antioxidant properties decreased oxidative stress induced by lipopolysaccharide in the rats. This study found the Black Cumin was thus an effective antioxidant and anti-inflammatory agent in lung inflammation. It prevented tissue damage and heightened inflammation that oxidative stress usually causes.
Dont Miss: Ulcerative Colitis Flare Up Symptoms
How A Colonoscopy Works
In a colonoscopy, a doctor uses a long, flexible tube with a camera at the end to see inside your colon. The test helps them detect polyps in your colon lining. The doctor can remove these growths to prevent them from turning into cancer.
Your doctor might also remove tissue samples during your colonoscopy and have them tested for cancer. This procedure is called a biopsy.
Donât Miss: Best Vegetables For Ulcerative Colitis
You May Like: Foods To Eat To Help Ulcers
Skin Joint Or Eye Problems
When you have UC, the lining of your large intestine gets inflamed and sets off your symptoms. For some people, this inflammation also shows up in other body parts during a flare. Experts arent sure why.
You could have symptoms like:
Let your doctor know whenever you get new UC symptoms. That way, they can change your treatment plan if needed.
Key Points About Ulcerative Colitis
Also Check: Natural Cures For Gastritis And Ulcers
You May Like: How Do I Know If I Have A Stomach Ulcer
Getting Referred To A Gastroenterology Team
If your blood and stool tests show inflammation, you should be referred by your GP to a defined specialist gastroenterology doctor in an IBD service. They have expert knowledge of gut conditions like Crohns and Colitis, and can do specialist tests like endoscopies . In some areas, you may be able to have some choice over which hospital you go to if you have been referred through the NHS e-Referral Service.
It may take some time to get an appointment with your gastroenterology team. The IBD Standards state that you should have a specialist assessment within four weeks of being referred, but it may sometimes take longer. Your GP should let you know how long you can expect to wait contact your GP surgery if you havent heard from the hospital within that timeframe so that they can chase up for you. You can also talk to your GP about how best to manage your symptoms while you wait for an appointment, and what to do if you start to feel worse.
You May Like: Medications To Treat Ulcerative Colitis
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Recommended Reading: Best Remedy For Stomach Ulcer