Lifestyle Changes To Treat Ulcerative Colitis
You can make dietary and lifestyle changes to help alleviate symptoms and lengthen time between flare-ups.
While there is no evidence that says certain foods cause ulcerative colitis, there are certain foods that can aggravate your symptoms. Limiting dairy products and avoiding problem foods may help improve your symptoms. Problems foods can vary for each person, but you should also avoid gassy foods such as beans, cabbage and broccoli, raw fruits and fruits, popcorn, caffeine and carbonated beverages. Experiment with fiber. For some, adding more high-fiber foods can help with bowel issues however, if you have an inflammatory bowel disease fiber may worsen your symptoms. Try eating five or six meals instead of two or three large ones and drink plenty of fluids, preferably water.
Avoiding stress is also a good way to alleviate your symptoms. Stress can aggravate your symptoms, so learning to better manage stress can help. Exercise, biofeedback, regular relaxation and breathing exercises are all ways you can manage stress.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Articles On Ulcerative Colitis Overview
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
Read Also: What Not To Eat When You Have Ulcers
Potential Harmful Consequences Of Nausea And Vomiting
Dehydration and/or imbalance of the bodys chemicals and minerals circulating in the blood are the most important acute harmful effects of nausea and vomiting. The doctor will measure vital signs , perform a physical examination to look for signs of dehydration, check levels of chemicals in the blood, test the kidney and liver with blood tests, and sometimes order testing of the heart. Treatment with intravenous fluids, sometimes with added chemicals , and medications to reduce nausea and vomiting may be used. When nausea and vomiting last for a long time, there may be weight loss or malnutrition. Feeding into the intestines or sometimes directly into a large vein may be needed.
Violent retching or vomiting can cause painful bruises or tears in the abdominal wall muscles, with pain and soreness to touch. Sometimes tears develop in the lining where the swallowing tube joins the stomach, called Mallory-Weiss tears. These tears may bleed, and the vomit may contain blood, or stools may turn black and sticky. Very rarely, the entire wall of the esophagus can tear, with escape of stomach contents into the chest or abdomen, called Boerhaaves syndrome. This is a serious condition and can lead to abscess formation or fluid collection, typically around the bottom of the left lung.
Diagnosing Causes Of Nausea And Vomiting

After talking to you and examining you, your doctor will often know why you have nausea and vomiting. Your doctor will try to understand what was going on before you started having nausea and vomiting.:
Also Check: Best Over The Counter Medicine For Stomach Ulcers
Symptoms Beyond The Intestine
When ulcerative colitis is raging, it can take its toll on more than just the GI tract.
The inflammation from ulcerative colitis can make patients feel very fatigued lead to blood loss, causing anemia and cause weight loss due to difficulty absorbing nutrients, says Dr. Ather.
Symptoms beyond the intestine affect mental health and quality of sleep, too. A study published in 2018 in the International Journal of Behavioral Medicine found higher rates of mental health and sleep disorders in people with ulcerative colitis.
It is important for us to screen for these issues and refer our patients to get the help they need, Dr. Ather says.
How Do Doctors Diagnose Ulcerative Colitis
To assist with diagnosing the cause of your symptoms, your doctor may take a full personal and family medical history and carry out a physical examination, according to the NIDDK. They may then order tests to confirm the diagnosis and assess the severity of the condition.
Tests that your doctor may order to assist with diagnosing ulcerative colitis include:
- Blood tests: checking for anemia, infection, and other digestive conditions
- Stool sample: checking for signs of inflammation and to rule out other possible conditions
- Endoscopy of the large intestine: looking inside your intestines using an endoscope
- Endoscopy of the large intestines can include a colonoscopy and a flexible sigmoidoscopy.
Your doctor can provide more information about the diagnostic tests they order. Make sure to ask them any questions you have before your tests.
Learn more about how doctors diagnose UC. You can also find out about what to expect after a UC diagnosis.
Also Check: Paleo Diet For Ulcerative Colitis
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
You May Like: What Causes Stomach Ulcers In Horses
Increased Appetite And Ibd
An increase in appetite and disordered eating can also occur in people with IBD. Binge eating, comfort eating, and impulse eating are all associated with IBD due to anxiety, depression, drug side effects, and factors associated with inflammation and the gut-brain axis. Flares also seem to affect appetite in some people.
Also Check: What Should You Eat If You Have Ulcerative Colitis
Read Also: Patient Education On Pressure Ulcer Prevention
What To Eat For Acid Reflux
Whether its a chronic condition or a newfound symptom of stressful days, heartburn happens! Avoiding spicy, acidic and fried foods as well as cutting back on alcohol and chocolate can help douse the flames and there are some foods you should gravitate towards to help reduce the discomfort. Heres what you can eat to help keep heartburn symptoms from being too upsetting.
How It Affects Daily Life
The diagnosis of UC usually comes before an individual reaches 35 years old. However, theres another time in life when UC is most frequently diagnosed at around 60 years old. An estimated 12 percent of those with UC are diagnosed in the decades before and after this age.
Regardless of when the disease is diagnosed, UC can take a significant physical and emotional toll on those living with this chronic condition.
The urgent need to use a bathroom multiple times a day can interfere with your social activities and your ability to work. Diarrhea can be unpredictable, highly inconvenient, and potentially embarrassing. In addition to physical symptoms, people living with UC may experience:
- elevated stress
Your doctor may be able to pinpoint some potential triggers. You may also find it helpful to keep a daily journal to track what you eat, your physical activities, and stressful events. In time, you may be able to identify a pattern that leads to diarrhea.
Read Also: Aloe Juice For Ulcerative Colitis
Recommended Reading: Can Ulcerative Colitis Cause Blood In Urine
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, persons with ulcerative proctitis generally do not have nutrient deficiencies however, other factors may influence an individuals nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, then modifications to the diet will be necessary to compensate for this.
Better overall nutrition provides the body with the means to heal itself. It is important to follow Canadas FoodGuide, but some foods may irritate the rectum and increase symptoms, even though they do not affect the disease course. The customized recommendations of a registered dietitian can address your sensitive digestive tract.
Medications For Ulcerative Colitis
Your doctor may prescribe medication to alleviate symptoms and reduce the risk of relapse when you are in remission, according to the NIDDK.
Medications for UC include:
- aminosalicylates to reduce inflammation in mild to moderate UC
- corticosteroidsto treat moderate to severe UC, particularly if you do not respond to aminosalicylates
- immunosuppressantsfor moderate to severe UC
- biologics to reduce inflammation in cases of moderate to severe UC
Find out more about treatment options for UC. You can also learn about finding the right treatment for UC.
Read Also: Foods Not To Eat If You Have Ulcerative Colitis
Changes To Your Bowel Movements Are A Potential Sign Of Colitis
Changes to your bowel movements that last for over two weeks should always be checked out, as theyre a clear sign that something isnt right with your digestive system. For colitis, the most common change is diarrhea, which might contain blood at times.
Not being able to pass a movement, or wind, is a symptom of ulcerative colitis, too. If youre not sure, keep a diary for two weeks and see if you can spot any patterns, like symptoms after certain food.
If youre not sure of the cause, and any changes to your bowel movements are persistent, make sure you come and see us to get checked out.
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Recommended Reading: What Is Ulcerative Colitis Pain Like
You May Like: What Not To Eat With Bleeding Ulcers
People Describe How They Were Diagnosed With Ulcerative Colitis
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohnâs disease .
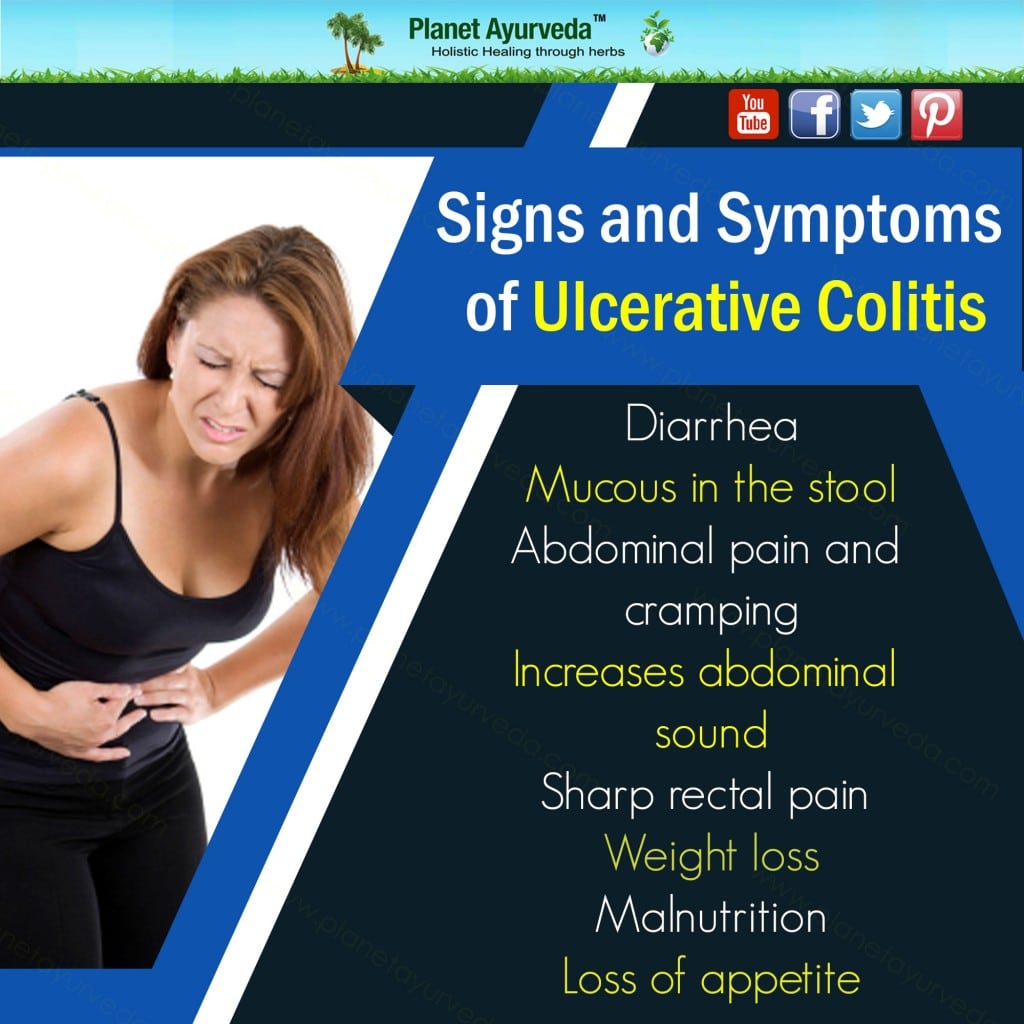
UC is a chronic conditionthat can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while thereâs no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesnât cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
When To Call A Professional
New or changing symptoms often mean that additional treatment is needed. People who have ulcerative colitis should be in frequent contact with their physicians.
Common symptoms that require a doctors immediate attention are:
- Fever, which could indicate infection or a ruptured intestine
- Heavy bleeding from the rectum
A serious, but uncommon, complication is called toxic megacolon. This results when the colon inflammation is so severe that it stops the colons motion. Megacolon causes the abdomen to swell. This can cause vomiting or severe abdominal pain and bloating. Megacolon requires emergency treatment, often surgery.
Also Check: How To Calm Ulcer Attack
Recommended Reading: Foods That Cause Ulcerative Colitis
Ibd Patients Perception Of Coffee On Their Bowel Disease
All participants were asked to give their general opinion whether regular coffee intake exerts a positive, negative or no influence at all on their bowel symptoms. In total 38 % of IBD patients assumed that coffee does have an overall effect on their symptoms, significantly more in CD than UC . Strikingly and highly significant, more than twice as many CD patients felt that coffee negatively influences their course of disease by worsening intestinal symptoms, as compared to only 20.2 % of UC patients . Among CD roughly an equal amount of patients as those stating an adverse influence of coffee did not attribute any effect on coffee on the course of their condition at all. This fraction of patients not identifying any disease modifying effect of coffee intake on the course of their IBD is significantly higher in UC .
IBD patients perception about the effect of regular coffee consumption on their intestinal symptoms. Significantly more patients with CD think that coffee has an overall impact on their bowel disease, compared to UC patients as depicted by brackets combining patients attributing a positive and a negative effect. Among UC patients, the majority do not think that coffee has any influence at all on their symptoms. Uniformly among all IBD subtypes, if an impact of coffee on disease symptoms is attributed by patients, only a small minority of patients experience a positive influence
What Happens When Dietary Intake Of Sulphur Is Reduced
There has been one pilot study undertaken to see if a reduction in sulphur amino acids of animal and plant origin would benefit patients with ulcerative colitis. There were two groups consisting of only 4 individuals. One group had recently had an exacerbation and the other group had not had a recent attack.
Those patients who began the project with a recent exacerbation reported no acute attack after 56 combined months of observation. Expected relapse on a 5-ASA medication for such a group would be 22.6%. All showed marked histological improvement. Three members of the chronic group also showed histological improvement with at reduced number of bowel movements from 6 to 1.5 per day, with a more formed stool. The fourth member of the chronic group was able to stop steroids and had no further acute episodes compared to 4 attacks of the same period prior to beginning the diet.
Read Also: What Is Peptic Ulcer Pain Like
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to poo frequently
You may also experience extreme tiredness , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is.
For some people, the condition has a significant impact on their everyday lives.