Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
What Medications Should Be Avoided With Ulcerative Colitis
When colitis strikes, medications to avoid will depend on the condition responsible. For instance, patients infected with toxic strains of E. coli need to avoid both antibiotics and antidiarrheal medications, both of which can make the condition significantly worse. There are, however, medications that irritate the bowel and cause or worsen colitis. These include nonsteroidal anti-inflammatory drugs , beta-blockers, statins, stomach acid reducers, vasopressors, and immune suppressants.
What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
You May Like: Why Do You Lose Weight With Ulcerative Colitis
Diet And Ulcerative Colitis
Diet can play a role in UC flare-ups, but a universal diet to help prevent these flare-ups doesnt exist. Instead, youll need to work with your gastroenterologist and possibly a nutritionist to create a diet plan thatll work for you.
While everyone reacts differently to foods, some foods you may need to avoid or eat in smaller quantities. This includes foods that are:
You may also need to avoid alcohol.
Use a food diary to help you identify your trigger foods. You may also want to eat smaller meals throughout the day to avoid extra discomfort from inflammation.
Speak with your gastroenterologist if you feel any flare-ups returning so you can work on a diet adjustment together.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
You May Like: Ozone Therapy For Ulcerative Colitis
How Close Are We To A Cure
Ulcerative colitis is an inflammatory bowel disease that mainly affects the lining of the large intestine . This autoimmune disease has a relapsing-remitting course, which means that periods of flare-ups are followed by periods of remission.
Right now, theres no medical cure for UC. Current medical treatments aim to increase the amount of time between flare-ups and to make flare-ups less severe. This may include a variety of medications or surgeries.
Still, UC research continues to explore other methods to decrease the inflammation associated with this autoimmune disease. Learn more about the new UC treatments that have recently come out on the market, as well as emerging therapies that could be other options in the future.
Two new types of medications for UC have emerged in recent years: biosimilars and Janus kinase inhibitors.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Also Check: Signs Of An Ulcer In A Woman
What Happens If Colitis Is Left Untreated
If ulcerative colitis is left untreated, it can raise the risk of colonic dysplasia and colorectal cancer. The only way to treat ulcerative colitis is to have the colon surgically removed. Medication and nutrition, on the other hand, can alleviate symptoms, delay progression, and help a person remain in remission for a longer period of time.
Taking medication daily and following a strict diet may seem like a lot to take on, but with proper guidance, most people are able to do this without difficulty. In fact, many people who suffer from ulcerative colitis find that taking care of themselves by eating well and exercising often makes them feel better overall.
The main goal of treatment for those who have ulcerative colitis is to reduce your chances of getting colon cancer by removing any chance factors you could have for developing this disease. This means avoiding cigarettes and alcohol consumption and maintaining a healthy weight. If you have diabetes, controlling blood sugar levels properly should be your top priority too. All these things can help prevent colon cancer from forming or growing if it has already formed.
About Article Author
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
Read Also: Ozanimod Phase 2 Ulcerative Colitis
Taking Care Of Yourself
Its natural that living with ulcerative colitis can make you feel stressed at times. Stress can sometimes trigger flare-ups so you may find it helpful to try some relaxation techniques. These may include deep breathing, meditation, yoga and mindfulness.
Regular exercise can also help to give you a boost and make you feel better. It can also improve your general health and help to keep your bones and muscles strong. This is important because some medicines for ulcerative colitis may affect your bone health.
You May Like: Is Coconut Milk Good For Ulcerative Colitis
What Tea Is Good For Colitis
Teas high in antioxidants, such as green tea, may help reduce swelling and pain of the intestinal tissues. Colitis is often associated with an increase in substances, called reactive oxygen species , which easily react with oxygen and can damage tissues and worsen inflammation. Infections, ischemia , radiation, and inflammatory conditions all increase the amount of these substances. Antioxidants neutralize reactive oxygen species by reacting with them before they react with molecules in the bodys tissues, minimizing the damage they do. While reactive oxygen species do not cause colitis, they can make the condition more unpleasant.
Don’t Miss: Can Ulcerative Colitis Cause High White Blood Cell Count
How To Stay Healthy
Keep up with treatment even when youre in remission. That means you need to take your medicine even if you feel good. See your doctor at least once a year so they can see how things are going. And like everyone else, its important to stay active and follow a healthy diet.
Get regular screenings for colon cancer. Your doctor will let you know how often you should get checked. You may need a colonoscopy every 1-3 years. Thats a procedure that helps your doctor look for cancer or cells that might become dangerous. Your chances of recovery go way up when you find and treat colon cancer early.
Show Sources
Recommended Reading: Whats The Difference Between Ulcerative Colitis And Crohns Disease
Uc Treatment Options At A Glance
The most commonly used treatments for UC:
These drugs, given orally or rectally, are anti-inflammatory compounds that contain 5-aminosalicylic acid . They decrease inflammation at the wall of the intestine. Examples of 5-ASAs include sulfasalazine, balsalazide, mesalamine, and olsalazine.
Metronidazole, ciprofloxacin, and other antibiotics may be used when infections occur, or to treat complications of ulcerative colitis.
Biologics for UC are designed to suppress the immune system to reduce inflammation. Certain biologics work by targeting specific inflammatory proteins called cytokines that play a role in inflammation. Others work by preventing certain white blood cells from getting into inflamed tissues.
Prednisone, prednisolone, and budesonide are included in this type of medication. They affect the bodys ability to initiate and maintain an inflammatory processkeeping the immune system in check. While effective for short-term flare-ups, theyre not recommended for long-term use.
These modify the bodys immune system activity to stop it from causing ongoing inflammation These drugs are usually used for people who have responded only to steroids.
Also Check: Foods To Avoid With Ulcerative Proctitis
Caring For Colitis At Home
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Don’t Miss: Pressure Ulcer Wound Care Dressings
Strategies To Reduce Your Risk Of Colorectal Cancer
Having regular colonoscopies is one of the most important preventive measures people with ulcerative colitis can take to reduce the risk of colorectal cancer.
There are also other steps people with UC can take to minimize risk, including avoiding smoking, limiting alcohol intake, maintaining a healthy weight, and exercising regularly.
Other tactics that have been shown to reduce the risk of colorectal cancer include the following:
When To See A Doctor
Anyone with symptoms of ulcerative colitis should see a medical professional for an evaluation.
Individuals who already have a diagnosis of ulcerative colitis should see a doctor if symptoms become worse. This development could be the sign of a flare-up, and appropriate treatment can help control inflammation.
People may want to consider seeking emergency assistance if symptoms are sudden and severe.
Doctors can prescribe a range of medications to treat people with ulcerative colitis. Treatment aims to relieve symptoms and induce and maintain remission.
Available treatment options for ulcerative colitis can include:
Lifestyle changes may also help a person better manage their ulcerative colitis. For instance, suggests that a low-fat diet with plenty of vegetables may reduce the risk of developing ulcerative colitis.
Lifestyle modifications that may help a person manage their symptoms include:
- drinking more liquids but avoiding sodas and other fizzy drinks
- replacing large meals with smaller, more frequent ones
- using a journal to track foods that may trigger flare-ups
- limiting high-fiber and high-fat foods, during flare-ups
Also Check: Ulcerative Colitis Flare Up Diet
How Long Does Colitis Take To Heal
Most illnesses last less than 1 week, although symptoms can persist for 2 weeks or more and relapses occur in as many as 25% of patients. In up to 16% of patients, prolonged carriage of the organism can occur for 2 to 10 weeks. Recurrent and chronic infection is generally reported in immunocompromised patients.
Is Ulcerative Colitis Curable
Ulcerative colitis can differ from person to person, but its usually a lifelong condition. Symptoms come and go over time.
Youll have flare-ups of symptoms, followed by symptom-free periods called remissions. Some people go years without any symptoms. Others experience flare-ups more often.
Overall, about half of people with ulcerative colitis will have relapses, even if theyre being treated.
Youll have the best outlook if the inflammation is only in a small area of your colon. Ulcerative colitis that spreads can be more severe and harder to treat.
The one way to cure ulcerative colitis is with surgery to remove your colon and rectum. This is called proctocolectomy. Once your colon and rectum are removed, youll also be at lower risk for complications like colon cancer.
You can improve your own outlook by taking good care of your ulcerative colitis and getting regular checkups to look for complications. Once youve had ulcerative colitis for about eight years, youll also need to start having regular colonoscopies for colon cancer surveillance.
It can be helpful to talk to others who understand what youre going through. IBD Healthline is a free app that connects you with others living with ulcerative colitis through one-on-one messaging and live group chats, while also providing access to expert-approved information on managing the condition. Download the app for iPhone or Android.
Recommended Reading: Is Cabbage Juice Good For Ulcerative Colitis
It Can Affect You Mentally Too
Beyond the physical symptoms, UC might also impact your mental health.
Fighting a war with your own body can take a mental toll.
- Around 35% of people with UC or Crohns disease experience symptoms of anxiety.
Note: A UC flare on its own typically doesnt lead to a new mental health condition like depression or anxiety, says Dr. Max Pitman, gastroenterologist at Salvo Health. But UC might worsen your existing anxiety or mood-based issues through the gut-brain connection.
When Im flaring up, its like being stuck in a dark fog. I feel hopeless, anxious, and even guilty often because I feel too exhausted to stick to work deadlines and have to cancel plans.
But, I had to learn how to give myself a break. Im not lazy: Im just tired. I have a chronic illness that impacts my gut. And my gut may affect my brain, in turn: One review found that people with IBD have higher rates of anxiety when the disease is active versus in remission, suggesting an upset gut may play a part in mental distress.
If youre having trouble managing your mental health, treatments like cognitive behavioral therapy could help.
Pitman recommends a form of CBT called gut-directed cognitive behavioral therapy, which helps you learn coping methods for your thoughts and emotions when you have a GI illness. Some research even suggests that gut-based CBT might improve digestive tract symptoms.
Recommended Reading: How To Stop Ulcers From Hurting
Symptoms Of Ulcerative Colitis
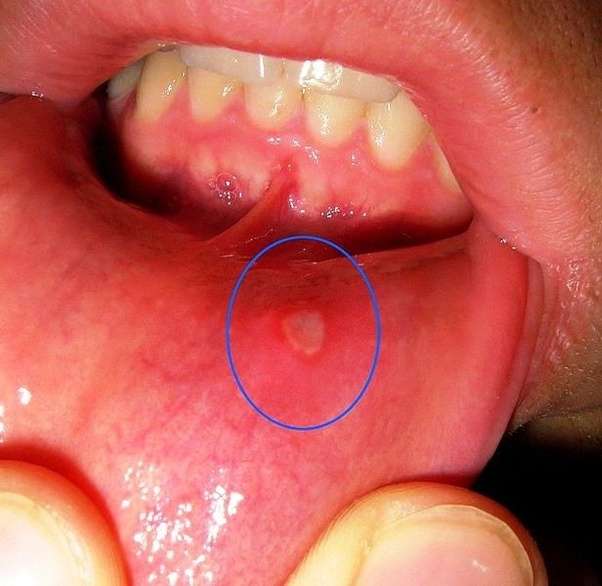
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience extreme tiredness , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is.
For some people, the condition has a significant impact on their everyday lives.
Recommended Reading: Rectal Treatment For Ulcerative Colitis
How Does Colitis Make You Feel
Most people with ulcerative colitis experience urgent bowel movements as well as crampy abdominal pain. The pain may be stronger on the left side, but it can occur anywhere in the abdomen. Together, these may result in loss of appetite and subsequent weight loss. These symptoms, along with anemia, can lead to fatigue.
Complications Outside The Bowel
Colitis doesnt just affect the bowel. As many as 1 in 5 people with Colitis develop problems in other parts of the body. Most affected are joints, eyes or skin. These are known as extraintestinal manifestations . They usually happen during a flare-up, but can occur without or before any bowel symptoms. These complications can often happen to people who dont have Colitis too. For many of the complications, there are things you can do to reduce your risk.
Joints
You may have pain and/or swelling in your joints. Around 1 in 6 people with Colitis experiences joint problems. For some, this will get worse during a flare, but will usually improve with treatment for Colitis. Others may have joint problems even when bowel symptoms feel better. Find out more in Joints.
Bones
People with Colitis are more at risk of developing thinner and weaker bones or osteoporosis. This can be due to ongoing inflammation, smoking, taking steroids or low levels of physical activity. Calcium is needed for bone formation, and this may be low if your diet doesnt contain enough dairy. Weight-bearing exercise, calcium and vitamin D supplements, not smoking and avoiding long-term steroid use can help. Some people may also take bisphosphonate medicines. Find out more in our information on Bones.
Skin
Colitis can affect the skin in different parts of the body.
Eyes
Anemia
Anaemia can make you feel very tired. If its more severe you may also have shortness of breath, headaches, and general weakness.
Liver
You May Like: Can Vyvanse Cause Stomach Ulcers