Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
Fatigue From Ulcerative Colitis Can Be Brutal
Exhaustion from ulcerative colitis can be so severe its hard to get through day-to-day life. For Sam, fatigue was one of the first signs that something was wrong. I’m usually a pretty energetic person, she says. I like running every day, things like that. And I just couldn’t do it anymore.
After developing ulcerative colitis, you might have to be more careful than youre used to about how you use your energy. Some days I’m just hit with a truck of fatigue, Skomski says. So I always give myself an out. If I have plans with friends or we’re going out of town, Ill tell the other people, I might not feel good and we might have to reschedule.
Sam has had to have similarly frank conversations about the fact that her energy can take a major dip sometimes. I’ve had to teach everyone around me that it doesn’t mean I’m mad at them, it doesn’t mean I’m not happy, she says. It’s just that I have a very concrete amount of energy that day.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Read Also: What Causes Ulcers On Your Lip
From Stabbing Sensations To Major Cramps Uc Pain Can Be Debilitating Heres What To Expectand How To Get Relief
by Health Writer
If youve recently been diagnosed with , you know: It can be hard to separate out symptoms of this gastrointestinal disease from the other aches and pains in your body. Is that stomachache due to a meal that didnt agree with you, or is caused by inflammation in your colon? Are those cramps related to your inflammatory bowel disease or your monthly cycle? Lets take a closer look at symptoms that make UC abdominal pain different from a run-of-the-mill stomachache, plus how to relieve the pain so you can get back to the things you love.
Bottom Line On Uc Pain Relief
You may be battling UC pain today but that by no means predicts your future. Complete remission should be a shared goal between you and your doctor. It may take patience to find the best treatment but living your life without UC pain is an achievable goal.
Pain Prevalence:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Over the Counter Medications: Mayo Clinic. Ulcerative Colitis.
How Imodium Works: Imodium. How IMODIUM Products Work.
How Tylenol Works: Tylenol. What Is Acetaminophen?
NSAIDs: Therapeutic Advances in Gastroenterology. Pain Management in Patients With Inflammatory Bowel Disease: Insights for the Clinician.
Prescription Medications:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Recommended Reading: Meals For People With Ulcers
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
What Are Common Signs Of Ulcerative Colitis
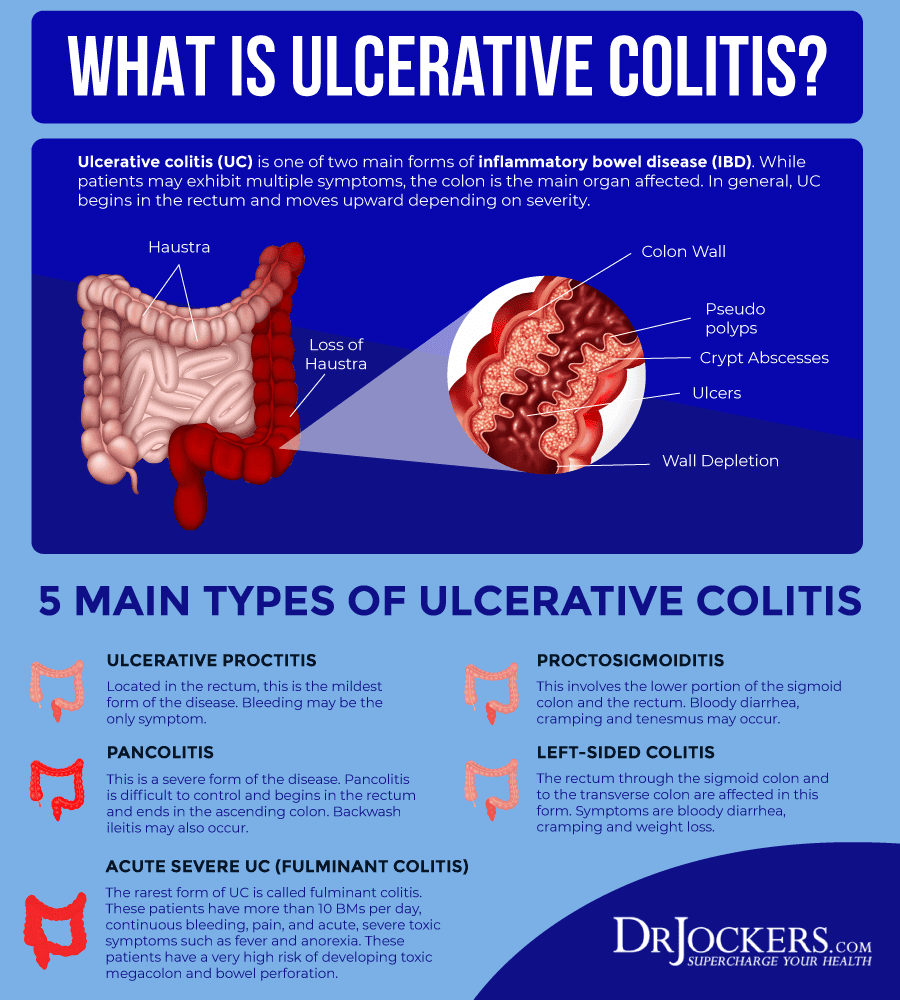
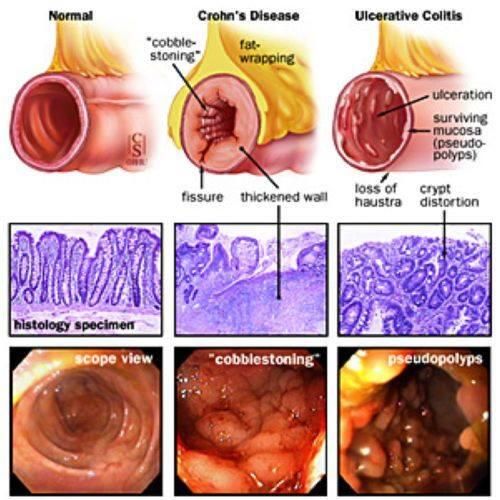
Ulcerative Colitis is a type of inflammatory bowel disease that affects your digestive tract. It causes inflammation and ulcers in the colon and rectum.
As one of the most common GI conditions, Ulcerative Colitis can cause some pretty serious health complications, so its important to contact a medical professional if you feel that you may have it. These are some of the common signs of Ulcerative Colitis that can help you identify the disease:
Bloody diarrhea. This is the most common sign of Ulcerative Colitis and can sometimes be accompanied by pus.
Abdominal pain and cramping. Cramps can occur due to the ulcers and inflammation caused by Ulcerative Colitis throughout the digestive track.
Rectal pain or bleeding. A noticeable pain may occur in the rectum. In Ulcerative Proctitis , this could be the sole symptom.
Urgent and frequent defecation. You might have difficulty holding in your stool and find yourself using the bathroom more frequently. Feelings of needing to go may wake you up at night or seemingly come out of nowhere. Frequent defecation can cause weight loss.
Inability to defecate. Oppositely, if you arent able to use the bathroom when you feel like you need to, you could have Ulcerative Colitis.
Other extraintestinal symptoms that may be related to Ulcerative Colitis are:
Sores or rashes. Physical sores or rashes may appear on the skin as a result of inflammation caused by Ulcerative Colitis.
Recommended Reading: Over The Counter For Ulcerative Colitis
People Describe How They Were Diagnosed With Ulcerative Colitis
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohns disease .
UC is a chronic condition that can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while theres no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesnt cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Responses have been edited for length and clarity.
Related:
Extraintestinal Manifestations And Complications
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes. Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Uveitis and iritis are more commonly associated with ulcerative colitis, whereas episcleritis is more commonly associated with Crohns disease.
Recommended Reading: How Does Ulcer Pain Feel
Questions To Ask Your Doctor
- How will my inflammatory bowel disease be treated?
- Will I need surgery? Are there other options?
- What lifestyle changes can I make to help inflammatory bowel disease?
- What are some medicines used to treat inflammatory bowel disease and what are the possible side effects?
- Are my children at risk of inflammatory bowel disease?
Symptoms That May Indicate You Are Suffering From Colitis
posted: Mar. 01, 2019.
Colitis literally means inflammation of the colon, and it happens when the lining of your digestive tract has become damaged, causing it to become inflamed and sore. There are a few reasons this damage might occur, including infection, food poisoning, restricted blood flow to the colon, and as a side-effect of cancer treatment.
Colitis can also be because of inflammatory bowel disease, such as Crohn’s disease or the most common form, ulcerative colitis. Inflammatory bowel disease affects over 1.6 million Americans , but you might not know you have anything more than the occasional stomach ache or digestive issue.
There are four particular symptoms that indicate you may suffer from colitis. If you recognize any of these signs, book a consultation to come and see the Hawaii Gastroenterology Specialists.
Don’t Miss: Can Ulcers Cause Bloody Stool
Abdominal Pain And Bloating Can Be More Than Just A Stomach Ache
Its not unusual to experience the occasional stomach ache when food disagrees with you, or stress might trigger Irritable Bowel Syndrome. Its when you appear bloated more often than not, and are experiencing persistent abdominal pain and cramps, you need to consider colitis.
This is particularly the case when your pain and bloating coincides with significant weight loss, vomiting, and even painful joints.
Many Disease Activity Indices Exist For Ulcerative Colitis But None Have Been Developed With Formal Patient Input
There is no consensus gold standard for the evaluation of disease activity in ulcerative colitis. This is illustrated in numerous recent clinical trials, in which investigators measured several different indices of disease activity, as no one index is considered sufficient. There are many indices for the measurement of ulcerative colitis disease activity, including Truelove and Witts classification of mild, moderate, and severe disease the St Marks Index, which empirically added endoscopy in 1978 simplified versions of the St Marks Index, including the Ulcerative Colitis Disease Activity Index and the Mayo Score and noninvasive versions, including the Seo Index and the Simple Clinical Colitis Activity Index .
The diversity of indices suggests that none of these has proven satisfactory, and none was developed with patient input. In addition, it has never been established that any of these indices actually measures all of the important symptoms of ulcerative colitis.
Ulcerative colitis lacks a validated measurement instrument such as the Crohns Disease Activity Index in Crohns disease . Furthermore, the indices that do exist for ulcerative colitis were not constructed in a patient-centered manner to attempt to capture the symptoms experienced by patients. Therefore, our study group aimed to investigate through focus groups that what symptoms does patients with ulcerative colitis experience during their disease process.
You May Like: How To Heal Mouth Ulcers Quick
What Does A Uc Cramp Feel Like
People who have UC describe a pronounced sensation of squeezing and releasing in their abdomen, Dr. Ha says, that feels more like pressure than a stabbing pain.
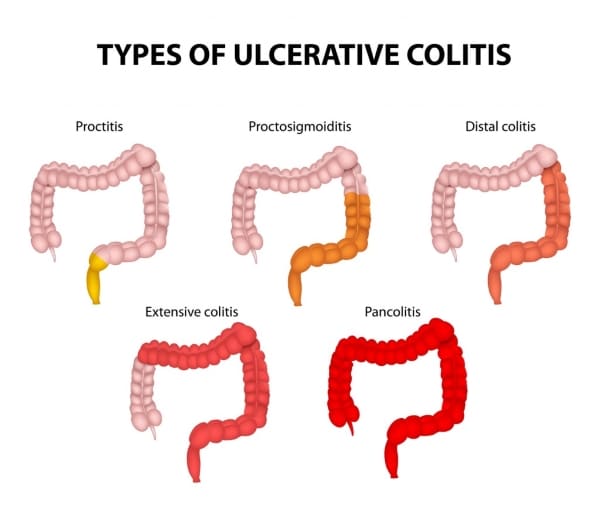
Doctors diagnose UC based on where symptoms are occurring. Many people with the condition experience whats known as left-sided colitis, where the pain and inflammation occur on their left side, from the rectum up to the descending colon.
Cramps can also be accompanied by bloating and gas, which cause a feeling of pressure and knotting in your abdomen.
Medications For Ulcerative Colitis
Medications can calm the inflammation inside your colon. The first one youâll usually try is from a group called aminosalicylates. If that doesn’t help, your doctor might prescribe a steroid like prednisone. A third option is an immune modifier, which lowers inflammation by changing the activity of your immune system. It can take up to 3 months before you feel the benefits.
Recommended Reading: Is Black Tea Good For Ulcerative Colitis
Complications Outside The Bowel
Colitis doesnt just affect the bowel. As many as 1 in 5 people with Colitis develop problems in other parts of the body. Most affected are joints, eyes or skin. These are known as extraintestinal manifestations . They usually happen during a flare-up, but can occur without or before any bowel symptoms. These complications can often happen to people who dont have Colitis too. For many of the complications, there are things you can do to reduce your risk.
Joints
You may have pain and/or swelling in your joints. Around 1 in 6 people with Colitis experiences joint problems. For some, this will get worse during a flare, but will usually improve with treatment for Colitis. Others may have joint problems even when bowel symptoms feel better. Find out more in Joints.
Bones
People with Colitis are more at risk of developing thinner and weaker bones or osteoporosis. This can be due to ongoing inflammation, smoking, taking steroids or low levels of physical activity. Calcium is needed for bone formation, and this may be low if your diet doesnt contain enough dairy. Weight-bearing exercise, calcium and vitamin D supplements, not smoking and avoiding long-term steroid use can help. Some people may also take bisphosphonate medicines. Find out more in our information on Bones.
Skin
Colitis can affect the skin in different parts of the body.
Eyes
Anemia
Anaemia can make you feel very tired. If its more severe you may also have shortness of breath, headaches, and general weakness.
Liver
Ulcerative Colitis Pain Location
Each person perceives pain differently and thus describes their pain in different ways. We list common pain descriptors below:
- A Charley Horse in your gut
UC pain location can also differ from person to person, depending on which part of their colon is most affected. The most common UC pain locations are listed below:
- Lower-abdominal pain
- This pain is typically associated with inflammation or ulcers in the colon.
- Often described as aching, cramping, spasmic pain.
You May Like: High Calorie Diet For Ulcerative Colitis
Feeling Chills And Ibd
| | |
Not every symptom of Crohns disease and ulcerative colitis is gastrointestinal that is, related to the digestive system. Some common symptoms are extraintestinal, meaning they affect other parts of the body. In addition to abdominal pain, cramping, bloating, diarrhea, and weight loss, people with inflammatory bowel disease can experience chills.
Fever and chills can have a variety of causes in people with Crohns or UC. They could be due to a drug allergy, or they may be a sign your IBD is becoming more severe. People on treatments that affect the immune system, like biologics, need to be aware of the reasons fevers can occur while taking these medications.
Its important to contact your doctor if youre experiencing fever and chills, especially if the symptoms intensify over time.
Can Inflammatory Bowel Disease Be Prevented Or Avoided
IBD cannot be prevented, but there are lifestyle changes you can make to minimize symptoms. The best thing you can do is to take good care of yourself. Its important to eat a healthy diet. Depending on your symptoms, your doctor may ask you to reduce the amount of fiber or dairy products in your diet. It also may be necessary to limit or avoid caffeine, alcohol, and carbonated beverages. In addition to eating well, you need to get enough rest and exercise regularly. Its also important that you learn to manage the stress in your life. When you become overly upset by things that happen at home or at work, your intestinal problems can get worse.
Read Also: Ulcer On White Of Eye
Upper Middle Abdominal Pain
A type of IBD called gastroduodenal CD often causes pain in the middle and upper sections of the abdomen. These Crohn’s disease pain locations correlate with problems in the:
This disease type is rare, accounting for only about 4% of all diagnoses. It’s even more rare for it to only impact the duodenum. This happens in just 0.07% of all CD cases.
Other symptoms of gastroduodenal CD may include:
- Fullness, or an inability to eat very much at once
| Jejunoileitis |
Triggers Of Ulcerative Colitis Pain
While UC pain can be managed through diet, there are also many behaviors that can contribute to UC pain.
- Irregular eating habits
- Waiting too long to eat after waking up, skipping meals and eating too quickly are all irregular eating habits that can produce inflammation in your gut. People with UC tend to experience less pain when they eat smaller, more frequent meals because this allows their body to more effectively digest and pass food. It is also beneficial to eat slowly in a relaxed environment.
Also Check: Signs And Symptoms Of Ulcerative Colitis Flare Up