Can Surgery Affect Nutritional Status
Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohn’s disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Ulcerative Colitis Diet Plan
Ulcerative colitis is a chronic, inflammatory bowel disease that affects the colon and rectum. If a person has ulcerative colitis, sores develop inside the colon. These are called ulcers.
It is not known what exactly causes ulcerative colitis, but researchers believe that it may be caused by a problem with the immune system. There are several things that may trigger a flare and worsen the condition. Foods are one of them. Certain foods may not be suitable for some people.
Read about causes of ulcerative colitis.
Researchers are learning about the role of diet and gut bacteria in causing the disease ulcerative colitis. The Academy of Nutrition and Dietetics and the Crohn’s and Colitis Foundation of America accept that fiber is helpful for your colon. Fiber should only be reduced if you experience acute problems such as flare-ups.
When you experience flare-ups, a low-fiber diet may be considered to help you recover quickly. But if your doctor has not recommended a low-fiber diet to manage the disease symptoms, you should follow a high-fiber diet only.
Foods To Eat With Ulcerative Colitis
My long-term nutrition goal for my clients with ulcerative colitis is always to move towards an anti-inflammatory diet where they eat as many whole plant foods as possible. It is thought that a more Mediterranean or anti-inflammatory diet pattern contributes to an healthier community of gut bacteria, a stronger gut barrier and a better immune balance between tolerance and inflammation. In one clinical trial, a plant-based diet improved relapse rates in ulcerative colitis. Other lab research suggests that a Mediterranean-style diet decreases risk of colitis. However, because of the nature of inflammation and irritation, it can often take very slow and sustained change over time to increase intake of plant-based foods comfortably.
- Fruits and Vegetables
Fruits and vegetables have been associated with a decreased risk of ulcerative colitis. They are high in anti-inflammatory phytochemicals and fibre, which is critical for production of short chain fatty acids by our gut bacteria that help to ease inflammation and support gut barrier function.
- Omega 3 rich seeds
We all need omega 3 rich foods in our daily diet ulcerative colitis is no exception. Data suggests that increased intake of omega 3 rich foods decreases risk of ulcerative colitis but clinical trials on fish oils have not offered conclusive benefits to disease outcomes.
- Calcium- and magnesium-rich foods
- High Fibre Foods, as tolerated
- Turmeric
- Psyllium
Recommended Reading: Can You Get An Ulcer In Your Intestines
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Olive Oil Coconut Oil Omega

Fat is an important component of a balanced diet. A good quality olive oil is best for sautéing over low heat and making cold dressings or sauces.
Coconut oil is worth trying, especially if you have a difficult time digesting fat. As a medium-chain triglyceride, its more easily and more completely digested without the help of bile salts than other plant oils. For that reason, it can be a good oil for people with malnutrition and malaborption problems.
Coconut is solid at room temperature, so it is versatile and can be used like butter for both sautéing over high heat and for baking.
Omega-3 fats are important because we cannot make them in our body. They are found in nuts, avocadoes, freshly ground flaxseed, and fish. Wild salmon and sardines are preferable to other fish as a source of omega-3s because of their low heavy metal content.
Artificial trans fats should be avoided altogether because it increases the risk of developing heart disease. Trans fat is used to make crackers, cookies, and other processed food because it extends the shelf life.
Recommended Reading: Ulcerative Colitis Symptoms Back Pain
Can Food Cause Crohn’s Or Colitis
We dont know what causes Crohns and Colitis but we do know that a combination of the following factors are likely to play a part:
- Genetics
- A problem with the immune system, where the body attacks its own cells
- Changes in the bacteria in the gut.
These, together with environmental factors, like food and stress, may trigger the conditions.There isnt any clear evidence that specific foods cause Crohns or Colitis. Some researchers think a diet low in fruit and vegetables may increase the risk of Crohns and a low intake of vegetables may increase the risk of Colitis for some people. Theres also some evidence that eating a lot of meat or table sugar, called sucrose, may increase the risk of Crohns and Colitis. But there isnt enough evidence yet to say for certain whether food affects the risk.
Ulcerative Colitis Diet: Advice From A Dietitian
If you have ulcerative colitis, knowing what to eat can be tricky. Its important to customize your food choices based on your current tolerance and health goals. This post will help you understand the current scientific thinking on ulcerative colitis and diet and how to move forward with the approach that is right for you.
We have been working with clients with Crohns disease and ulcerative colitis in our practice for over seven years its an area I am passionate about because of the massive toll these diseases take on peoples quality of life. I also believe that nutrition can play a much larger role in the management of the diseases than is often discussed in the doctors office.
As a dietitian, I believe that the goal of nutrition is more than just ensuring you get all the vitamin D you need. I believe and have seen firsthand in my practice that creating a strong individualized approach to nutrition can help people find healing and learn how to thrive, no matter their diagnosis. Which is why it is frustrating that much of the scientific literature on ulcerative colitis is focused on either associating the risk of disease with certain foods, or acute strategies for securing remission in a flare.
Read Also: What Are Ulcers Caused From
Dietary Advice For Ulcerative Colitis
Please note, this page is printable by selecting the normal print options on your computer.
What is Ulcerative Colitis?
Ulcerative Colitis is a form of Inflammatory Bowel Disease . IBD is a term used to cover a number of inflammatory conditions of the gastrointestinal tract. UC causes inflammation in the large bowel and can affect the rectum, part of, or the entire colon. If you have UC this diet sheet may help you.
Can diet help?
Diet is not a cause of UC however diet can help to relieve symptoms such as diarrhoea during a flare up and maintain good health including healthy bones. You may find as time goes by you begin to notice that certain foods aggravate your symptoms of UC and so they are best avoided. However, do not remove whole food groups as this could mean you lose some vital nutrients. The main food groups are demonstrated below in the Eatwell Guide.
What foods are beneficial for UC during a flare up?
Soluble FibreDietary fibre can be categorised into two forms, soluble and insoluble. Soluble fibre is partially digested in the large intestine to form a glue like substance, which helps to produce soft/formed stools, without causing inflammation. Examples of foods rich in soluble fibre are:
- Oats e.g. Porridge oats/Ready Brek ®, oatcakes
- The body of fruits and vegetables e.g. peeled apples and pears, tinned fruit, peeled root vegetables such as carrots, parsnips, turnip
What foods may worsen UC during a flare up?
Dairy foods
Spicy foods and fatty foods
More Information About Ulcerative Colitis
According to George Washington University, colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon.
The following diseases fall into the colitis/IBD category they all can be treated with a combination of medication and improvements to your eating habits:
Recommended Reading: Removing Colon Due To Ulcerative Colitis
What To Eat On An Ulcerative Colitis Diet During Remission:
What you should eat on an Ulcerative Colitis diet plan is very individual but lets get acquainted with what it takes to be on an Ulcerative Colitis diet plan when your disease is not active:
What You Can Eat on an Ulcerative Colitis Diet.
-
Eat a variety of vegetables and fruits.
-
Select the refined grains. These have been milled to remove the bran and germ, may increase symptoms.
-
Include protein-rich foods.
-
Get enough calcium.
-
Drink plenty of fluids.
Your Ulcerative Colitis diet plan can even be more liberal when your symptoms subside but remember to:
-
Go Slowly. Gradually add more foods back into your diet. Shift to whole grains and those colorful veggies and fruits. Start with small amounts of these foods. If your symptoms act up, add that item to your potential list of trigger foods. You can try eating that food at a later time.
-
Eat 5 or 6 small meals per day. Go easy on your GI tract. Large meals can flare your symptoms and make you feel bloated.
-
Stay well hydrated. Sip on water throughout the day. As you add back in fiber, getting enough to drink is important. Fiber without adequate fluid intake can lead to constipation.
-
Avoid your trigger foods. Focus on the foods you can eat and enjoy. Create a list of substitutions for your trigger foods.
Foods That May Help Avoid Flares
Some healthful foods may have anti-inflammatory effects that can help control the underlying inflammation of Crohns disease and ulcerative colitis. Many of these foods are unprocessed. They also tend to have lots of color. Some of the substances that give fruits and vegetables their color have anti-inflammatory and other healthful effects.
Eating this way helps support anti-inflammatory pathways in our bodies, which may be very helpful when managing an inflammatory disease like IBD. In addition, if you are not flaring, eating healthful foods will also help you avoid any deficiencies in vitamins, minerals, and other nutrients.
Don’t Miss: What Is Best Medicine For Ulcer
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
Watch out for items that can be troublemakers if you have UC, including:
- Alcohol
Ulcerative Colitis Foods To Avoid
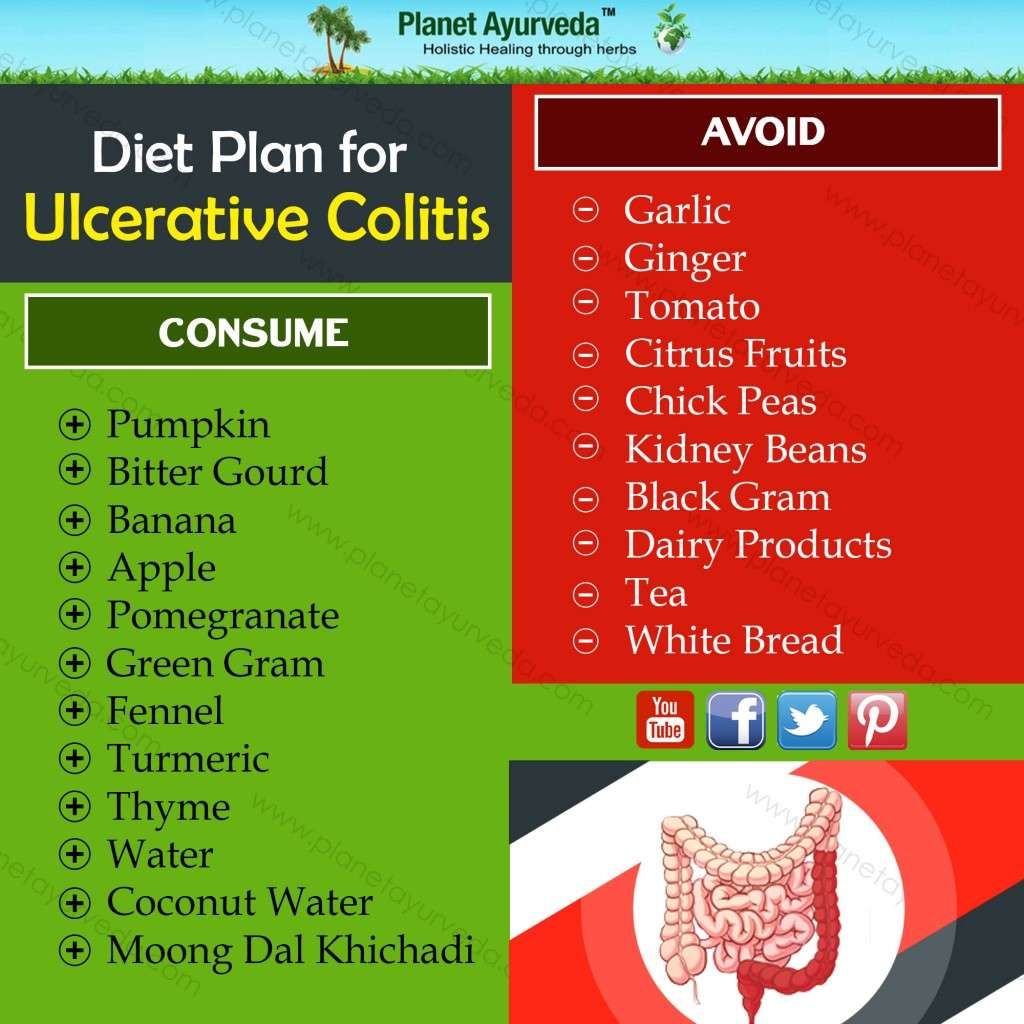
Now that we have looked at foods good for ulcerative colitis, well outline foods to avoid with ulcerative colitis. If you have received a diagnosis recently, you will likely find the list below helpful:
When you suffer from ulcerative colitis, you can feel desperate for relief, and it can be easy to get caught up in fad diets that claim to cure ulcerative colitis. Diet does not cure this inflammatory bowel condition but dietary changes can reduce symptoms. To find the best diet for your individual situation, it is best to talk to your gastroenterologist and a nutritionist who is familiar with UC. Again, there may not be a diet cure, but what you eat can make a big difference in your comfort level as you live with this chronic disease.
Also read:
Mohan Garikiparithi got his degree in medicine from Osmania University . He practiced clinical medicine for over a decade before he shifted his focus to the field of health communications. During his active practice he served as the head of the Dept. of Microbiology in a diagnostic centre in India. On a three-year communications program in Germany, Mohan developed a keen interest in German Medicine , and other alternative systems of medicine. He now advocates treating different medical conditions without the use of traditional drugs. An ardent squash player, Mohan believes in the importance of fitness and wellness.
Don’t Miss: Best Diet For Gerd And Ulcers
Lay Off Sweets And Sugar
One of the ways scientists suspect that sweets and sugars are not good for those with UC is that they studied what those from Japan ate 20 years ago: a diet high in rice and low in sweets and sugars. Since that time, sweets and sugars have been on the rise in Japan as well as UC. While this may paint only part of the picture, other studies have shown that high consumption of soft drinks has been associated with UC.
What To Eat With Ulcerative Colitis
Although there is no universal standard dietary plan for people with UC, there are some things we know about IBD and the microbiome that can help guide food recommendations. In our practice we focus on two areas when it comes to dietary recommendations:
- Choosing things to reduce inflammation & risk of flare
- Choosing things that will improve quality of life & reduce symptoms
Before we delve into the guidance- if you arent familiar with the 4 types of remission be sure to check out our previous article. As you navigate nutrition for UC, its important to note that what triggers symptoms- doesnt always trigger inflammation. Also, the opposite is also true- an inflammatory diet pattern doesnt always lead to immediate symptoms.
Typically, the best type of diet for UC is a plant-based diet thats rich in omega 3-fatty acids. Discussed below are some foods that are helpful for people with ulcerative colitis:
Read Also: Is Ginger Tea Good For Ulcerative Colitis
Fructose & High Fructose Corn Syrup
Ascientific study that examined the effect of fructose among people with ulcerative colitis concluded that high amounts of fructose causes can be inflammatory in UC. Fructose can be found in several foods, including corn syrup, honey, fruit juice, and molasses. Fructose also depletes the layer of mucus lining the colonic wall, exposing it to bacteria that eat up the colonic lining. That results in inflammation.
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
Also Check: Can Ulcers In The Colon Be Cancerous