Case Of The Month: Refractory Ulcers After Roux En Y Gastric Bypass
Refractory RYGB ulcers are troublesome for both the patient and the bariatric surgeon. Dr. Adrian Marius Nedelcu presents a case representing this complication and how it was managed. An expert commentary by Dr. Dino Spaniolas and his colleague Dr. Andrew Brown on the management of ulcers after gastric bypass is attached.
Case
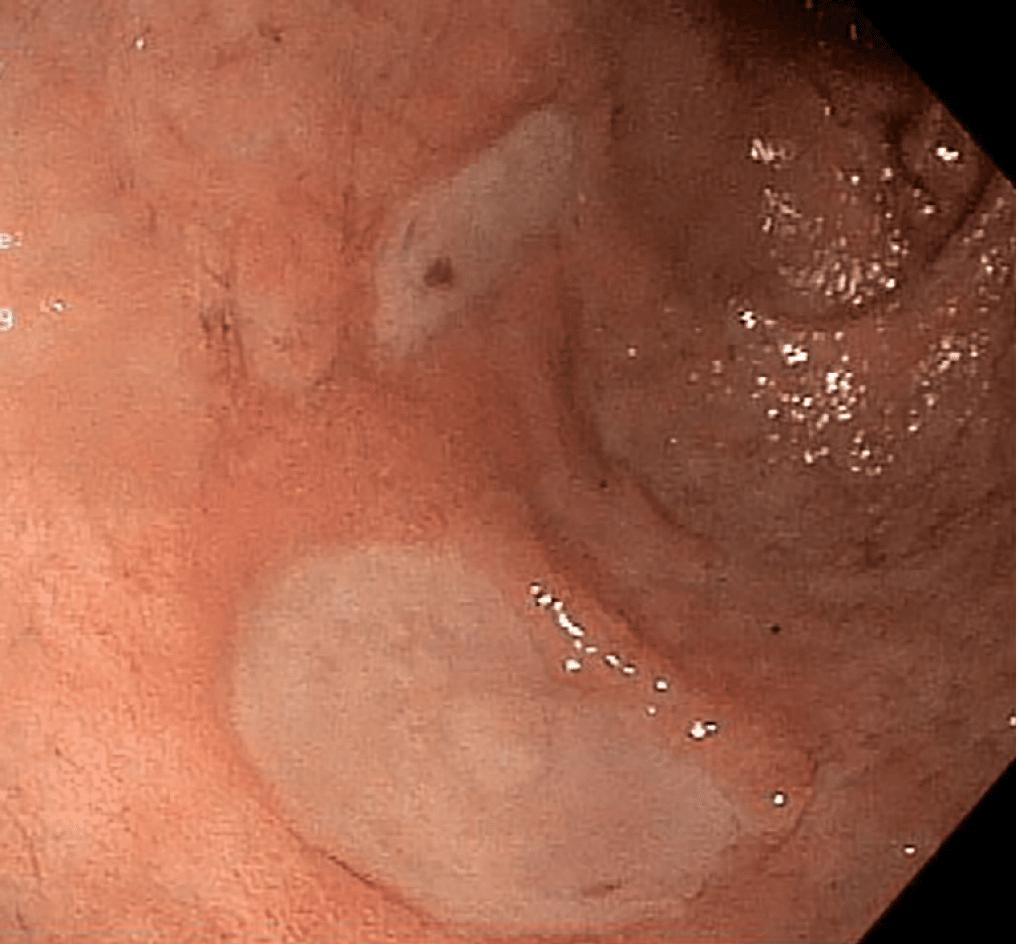
After an initial asymptomatic period, at 6 months follow up visit she is starting again to describe excruciating epigastric pain. The endoscopy showed us an important ulcer which was treated initial by medical treatment . During this period the patient had 2 negatives nicotine urine tests and no use of AINS was identified. An abdominal CT and MRI were negative for any type of tumor and the gastrin level was normal. The endoscopic control showed an important perianastomotic ulcer .
Different surgical options were discussed. The total gastrectomy with eso-jejunal anastomosis is representing the radical option. The patient was not very enthusiastic about this option. The reversal to the normal anatomy was not a real option as the symptoms of reflux following sleeve were really invalidated. To perform isolated truncal vagatomy is representing an option with insufficient results in the literature.
In conclusion we decided with patient to perform a pouch revision with almost complete gastrectomy with complete manual anastomosis. The hospital stay was 2 days with uneventful postoperative recovery. The postoperative control at one month was normal.
Medical
Symptoms And Side Effects Of Ulcers
The most common symptoms of stomach ulcers post-gastric bypass surgery are:
- Upper abdominal pain
- Bloating and gas
- Loss of appetite
Bleeding ulcers can lead to anemia in patients. Other problems you could encounter include Gastrogastric Fistula, a condition where the acid content and blood leak from your pouch to the intestines prompting severe stomach pain, nausea, and vomiting. About 25% of people with Marginal Ulcer complications are asymptomatic.
Dont Ignore the Symptoms
Ulcers can quickly become a severe after-effects and a life threatening situation. Ignoring these symptoms can put you at risk for bleeding, stomach perforation, or worse. Ulcers should be diagnosed and treated by your medical physician.
Buffering Effect Of Nutrients
After RYGB, there is no counteracting effect on the acid in the antrum and duodenum as the ingested food bypasses the excluded segments. However, the exclusion of the duodenum also leads to a reduced and desynchronized pancreatic secretion as the strongest stimulus of bicarbonate secretion is the duodenal presentation of nutrients. Furthermore, bile refluxing into the gastric remnant also contributes to mucosal injury .
Read Also: Does Ulcerative Colitis Cause Fever
Prevent Ulcers After Gastric Sleeve Surgery
A surgeon will typically use staples when resizing the stomach, and these can disturb delicate areas of the stomach lining, which can result in general irritation, a disruption of acid production, or even infection.
While the stomach lining is capable of and does repair itself, it can be challenging to treat ulcers because the acid in the stomach is continually contacting the stomach wall and irritating these sensitive spots.
There are some things that we ingest that can make ulcers worse. The following are some examples you should note of what to cut out of your daily life:
- Tobacco use: Whether it is the smoking or chewing variety, tobacco can make ulcers worse or even make them more likely to develop in the first place because they can cause acid production to increase.
- Alcohol and caffeine: Both of these types of beverages are acidic and will irritate the stomach.
- Medications: Over the counter pain medications like Aspirin can irritate the stomach and increase the possibility of ulcers.
- Food intolerances: While you will likely be restricting your food and sticking to mostly mild, whole foods post-surgery, you should be aware that your stomach may be more sensitive to certain types of foods than it used to be. As you keep a food journal, be sure to take note if you are eating anything that causes irritation or heartburn.
Find out if you qualify for the Gastric Sleeve in Mexico by clicking through to our online application form or contact us today to find out more.
Signs And Symptoms Of Ulcers After Gastric Bypass
Ulcerations after Roux-en-Y Gastric Bypass is one of the possible complications causing the patient pain and the bariatric surgeon headaches. The more prevalent case is the marginal ulcer, mucosal erosion at the gastrojejunal anastomosis. This condition can be treated with medications however, surgical intervention is needed in severe cases.
Smoking, caffeinated drinks, alcohol, and certain medications like NSAIDs are major risk factors for gastric bypass ulcers.
This post explains the types, causation, as well as medical and surgical management of ulcers in detail.
You May Like: Foods For Acid Reflux And Ulcers
Factors Contributing To Ulcers After Gastric Bypass Operations
According to one study performed on 441 morbidly obese patients who underwent either laparotomic resectional gastric bypass or laparoscopic gastric bypass, 12.3 % of those who went through laparoscopic gastric bypass showed signs of marginal ulcer in its early stage compared to 4.15% that underwent laparotomic resectional gastric bypass . Thus, this study concluded that those patients in whom the excluded gastric segment was left in the stomach were more susceptible to early marginal ulcers after the gastric bypass operations.
Other factors present in gastric bypass patients that make them susceptible to having ulcers after their gastric bypass operations are having large gastric bypass pouches, having vertically oriented pouches, and having staple-line dehiscence or disruption.
The presence of vertically oriented pouches is interconnected with staple-line disruption, as a study shows that patients with vertical pouches had the highest incidence of staple-line disruption, which therefore led to ulceration.
Also Check: Does Ulcer Pain Come And Go
Ulcers After Wls: Causes Symptoms And Treatments
Think of an ulcer as a sore in the lining of your stomach. They can cause pain, bleeding or make a hole in the stomach called a perforation. They can develop within a few months or even years out from surgery.
It is important for bariatric patients to know what are the causes and symptoms of gastric ulcers, when to contact their surgeon and how to prevent them from happening.
Donât Miss: Can Ulcerative Colitis Cause Blood In Urine
Read Also: What To Avoid Eating With Ulcerative Colitis
Causes Of Ulcers After Wls
Some causes of ulcers after WLS are preventable and others are beyond our control. The most common causes are smoking and NSAIDs. NSAIDs also known as non-steroidal anti-inflammatories Ibuprofen, Naproxen, Motrin or Aleve. Drinking alcohol and taking steroids such as Prednisone can also be the culprit.
Smoking can affect the lining of the stomach by reducing the amount of oxygen that gets to the tissues causing damage. It can also impair wound healing.
NSAIDs can damage the lining of the stomach leading to gastritis or an ulcer. Steroids may also affect the lining of the stomach and can delay healing. If you require NSAIDs or oral steroids for certain conditions, please check with your surgeon first.
Alcohol is something to be cautious of after surgery. Not only can you absorb alcohol much quicker, but it also irritates your pouch. Imagine pouring rubbing alcohol on an open wound this is the sort of effect that drinking alcohol has on your stomach.
Lastly, caffeine has not been shown to be a direct cause of ulcers however it can act as an irritant. If you already have gastritis or inflammation inside your stomach, caffeine can make it worse.
Gastrogastric Fistula and Helicobacter Pylori
Factors out of our control leading to an ulcer include a large gastric pouch, gastrogastric fistula, Helicobacter pylori, and sutures used to close the pouch. It is thought that a large pouch produces too much acid which can lead to an ulcer.
Symptoms of Ulcers
Stomal Ulcer After Gastric Bypass1
Stomal ulcer is a serious complication of gastrogastric fistula following Roux-en-Y gastric bypass for obesity.
Study Design:
A 18 year continuous followup of 499 patients with gastric bypass in continuity and isolated gastric bypass documented the incidence of fistula formation, development of stomal ulcer, stimulation of acid production within the gastric pouch, and response to treatment.
Results:
In 123 GB patients, staple line disruption occurred in 36 and stomal ulcer occurred in 20 . Gastrogastric fistula with stomal ulcer was significantly lower in 376 patients who underwent IGB, . Significantly larger amounts of acid, a lower pH, and a greater time with a pH less than 2 were found in the gastric pouches of patients who developed stomal ulcer after Roux-en-Y gastric bypass. All patients had a perforated staple line. Successful closure of the staple line significantly decreased acid production and pH in the gastric pouch when tested before and after remedial operation with healing of stomal ulcers.
- Previous article in issue
Read Also: Gel Cushion For Pressure Ulcers
Incidence Of Gastritis And Predictors Of Pud
Studies evaluating the gastric remnant after RYGB are rare. Among 53 patients with RYGB, remnant gastritis was found in 87% of patients with a normal mucosa in the pouch, indicating a harmful effect of unbuffered acid on the gastric remnant . Elsewhere, in more than half of patients taking PPI, endoscopy of the gastric remnant revealed peptic changes .
Considering symptoms as surrogates for gastritis and PUD, upper abdominal pain by far is the most frequent symptom leading to readmissions after RYGB . Of the reported patients, over two-thirds reported epigastric and/or upper abdominal pain.
Other Reasons To Quit Smoking Before Bariatric Surgery
In general, smokers after bariatric surgery have a 30% increased risk of complications. Similarly, long-term smoking can decrease ability to lose weight and increase the risk of future complications, such as ulcers at the site of surgery.
You risk surgery postponement or cancellation if you smoke within four weeks prior to your procedure. Some surgeons will not risk performing the surgery due to the complications and difficult healing process brought upon by smoking.
Though it may be difficult to quit smoking before bariatric surgery, overall life expectancy increases by about 10 to 15 years for patients who go through weight loss surgery. Meanwhile smokers, on average, see a in life expectancy of about ten years when compared to nonsmokers. Therefore, we encourage all of our bariatric patients to quit smoking as they make a commitment to leading a healthier life.
Read Also: Can You Drink Alcohol If You Have Ulcerative Colitis
Tobacco And Weight Loss
Tobacco use is actually more prevalent among obese people than it is across the general population, with up to 38 percent of obese individuals being regular users of tobacco products. When you are making the choice to undergo weight loss surgery, it is time to put the tobacco products away for good. Aside from the standard health issues that smoking causes, from increasing risk of heart and lung disease to damaging the skin and posing an increased risk of cancer, smoking is a surgical risk factor.
Bariatric surgery has a rather low risk factor, with under a one percent mortality risk. Among smokers, however, that risk doubles. This means that you are twice as likely to experience serious surgical complications leading to death if you are a smoker. Smokers are 1.5 times more likely to experience non-fatal surgical risks, too. This is just part of the reason why so many weight loss surgeons mandate that smoking cessation happens at least one year prior to surgery.
Smoking increases your risk of experiencing the following surgical complications:
- Surgical wound infection
Smokers have almost a 30 percent complication rate after weight loss surgery, which is astoundingly higher than the surgical complication rate for non-smokers.
Whats the Secret to Maintaining a Healthy Weight?
Risk Factors For Ulcers
Some of the most common risk factors for developing ulcers after bariatric surgery include the following:
- Type of Bariatric Surgery Procedure Ulcers after weight loss surgery tend to be more likely in patients who have undergone gastric bypass surgery or a sleeve gastrectomy.
- Smoking and Use of Tobacco Products Smoking and tobacco, in general, can lead to issues with recovery and healing time, resulting in a greater chance of an ulcer developing. Additionally, tobacco use can increase the risk of Heliobacter pylori infections.
- Use of Certain Medications Aspirin, ibuprofen, and anti-inflammatory drugs can all cause stomach irritation and disturb the normal repair processes of the body, which makes postoperative ulcers more likely.
- Alcohol Consumption Alcoholic beverages can irritate the lining of the stomach, making a person more prone to developing an ulcer.
- Drinking Caffeinated Beverages Caffeine can increase the amount of stomach acid and its potency, which can irritate and worsen an existing stomach ulcer. This is just one of many reasons why caffeine intake should be limited after bariatric surgery.
A healthy diet and proper health practices can go a long way toward preventing an ulcer from forming.
You May Like: How To Cure Ulcer Naturally
Gastrin Levels And Acid Production In The Excluded Stomach
After RYGB, there is continued, although diminished, basal, and stimulated acid excretion in the excluded stomach. Gastrin levels are decreased after RYGB, yet the gastric mucosa maintains its ability to respond to vagal and hormonal stimuli , thus preserving an acidic environment . The amount of acid production is influenced by the proportion of the parietal cell mass, partitioned by surgery to the pouch and the distal stomach, a factor certainly influencing the development of MU . In theory, high transection increases acid production in the excluded stomach and contributes to acid-related mucosal injury in the antrum and duodenum . Furthermore, post-RYGB, cellular hypertrophy of the gastric mucosa occurs in the presence of a reduction in G cells, again lowering gastrin production . Additionally, in proton-pump inhibitor treated mice with normal anatomy, the resulting hypochlorhydria causes bacterial overgrowth resulting in gastric inflammation .
Confessions Of A Twirly Girl
This blog blossomed in 2010 to chronicle my adventures in pole dance after weight loss surgery. Although I am pole dancing less these days, I still hike and do yoga. I sometimes still have to remind myself that the size of my body doesnât dictate my worth. I believe living a life full of gratitude and joy helps lead to a true mind, body and spirit connection. You have the power to manifest your best life!
Read Also: Removing Colon Due To Ulcerative Colitis
Also Check: What To Eat With An Ulcerative Colitis Flare Up
Ulcers After Gastric Bypass Surgery
Gastric bypass surgery is one of the most common bariatric procedures available for patients who are dealing with morbid obesity, hypertension, and type 2 diabetes. This surgery has proven to be useful for losing weight and for correcting or reducing other comorbid issues, such as hyperlipidemia, GERD, and lower back pain. The postoperative recovery process takes several months and if the procedure goes over smoothly, the patient should expect positive results, as long as they also follow their doctors recommendations on how to take care of their body.
These recommendations can include a determined resting period, prescribed medication, a specific diet, and removing certain habits from your daily life that could hinder your recovery. However, its important to keep in mind that all surgeries can have potential complications during and after the procedure, and the gastric bypass is not exempt from this. Some complications that may arise include infection, hemorrhages, hernias, and ulceration.
Our team at LIMARP®, led by Dr. Liza María Pompa González, takes care of you on each step of the surgical process so that any arising complication can be treated effectively and safely. We also like to keep our patients well-informed and the present article mainly focuses on the ulceration that may happen after the gastric bypass surgery, what causes it, and how to treat it.
Learn More About Weight Loss Surgery
Weight loss surgery has myriad benefits to your health and overall sense of wellbeing. The team at Tijuana Bariatric Center knows this firsthand, having improved the lives of countless people through state-of-the-art bariatric surgery.
For more information about weight loss surgery, including the risk of ulcers after bariatric surgery, how it can benefit you, and what complications you may face, contact Tijuana Bariatric Center today at 800-970-0577 to schedule a virtual consultation. We will work closely with you to ensure your health and wellness after losing weight by surgical means.
Tijuana Bariatric Center is a facilitator company providing scheduling and marketing services. It is not a medical facility or healthcare provider. Tijuana Bariatric Centershall not be liable to anyone for any decision made or action taken in reliance on this information. This information does not constitute medical advice, results are not guaranteed, may not be permanent, and can vary per individual and does not establish any physician-patient relationship. The correct venue for claims regarding the actual medical services provided either by the medical facilities or surgeons or medical staff will be Mexico. Any claims against Tijuana Bariatric Center must be asserted within 90 days of the event.
*Disclaimer: results are not guaranteed, may not be permanent, and can vary per individual. Some images are of models, not actual patients.
You May Like: Possible Causes Of Ulcerative Colitis
Working On A Manuscript
Laparoscopic Gastric Bypass is a safe and effective treatment for obesity and its comorbidities . It is one of the most common bariatric surgeries worldwide and thus, permanent improvement of the surgical technique is necessary to reduce the number of intra- and postoperative complications. In long-term studies, we still observe postoperative complications that require revisional surgery, such as internal herniation, chronic reflux, malnutrition, anastomotic leakage, strictures and anastomotic ulcerations . The latter is reported in up to 16%, but the incidence may be even higher when AU are subclinical and remain undetected . AU can cause chronic epigastric pain, reflux or digestive disorders and is primarily treated conservatively. When conservative treatment fails, a revision of the gastrojejunostomy is necessary and patients sometimes even require emergency surgery when perforation occurs .
To this point, surgical technique , chronic gastric disease , comorbidities , hypertension ), demographic factors and the prophylactic use of proton pump inhibitors are still a matter of discussion for the development of AU .