Symptom No : Irregular Periods
Solution: Treating your ulcerative colitis will often help correct an irregular menstrual cycle. Active colitis and anemia, for example, could lead to irregular periods, he says. Stress can also throw off your cycle.
Dr. Vaughn recommends talking with your gynecologist first to make sure there arent any underlying issues.
Articles On Ulcerative Colitis Overview
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
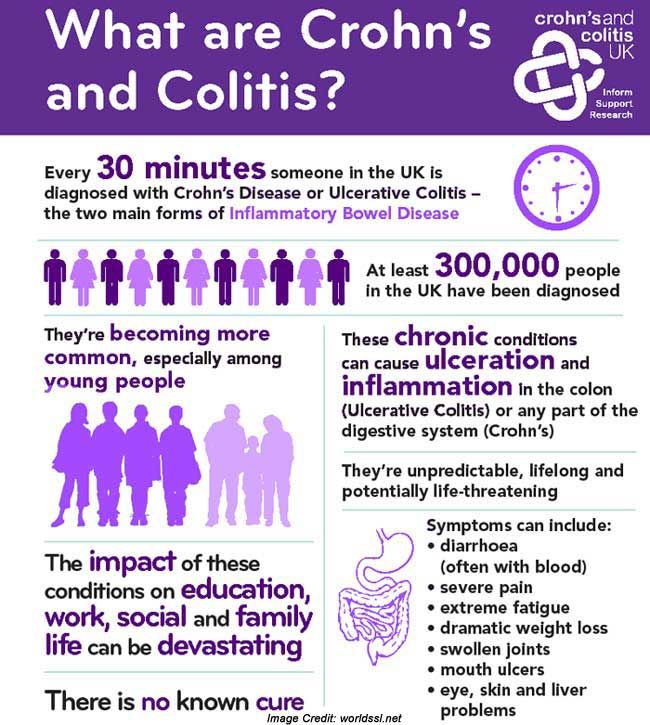
Basics Of Inflammatory Bowel Disease
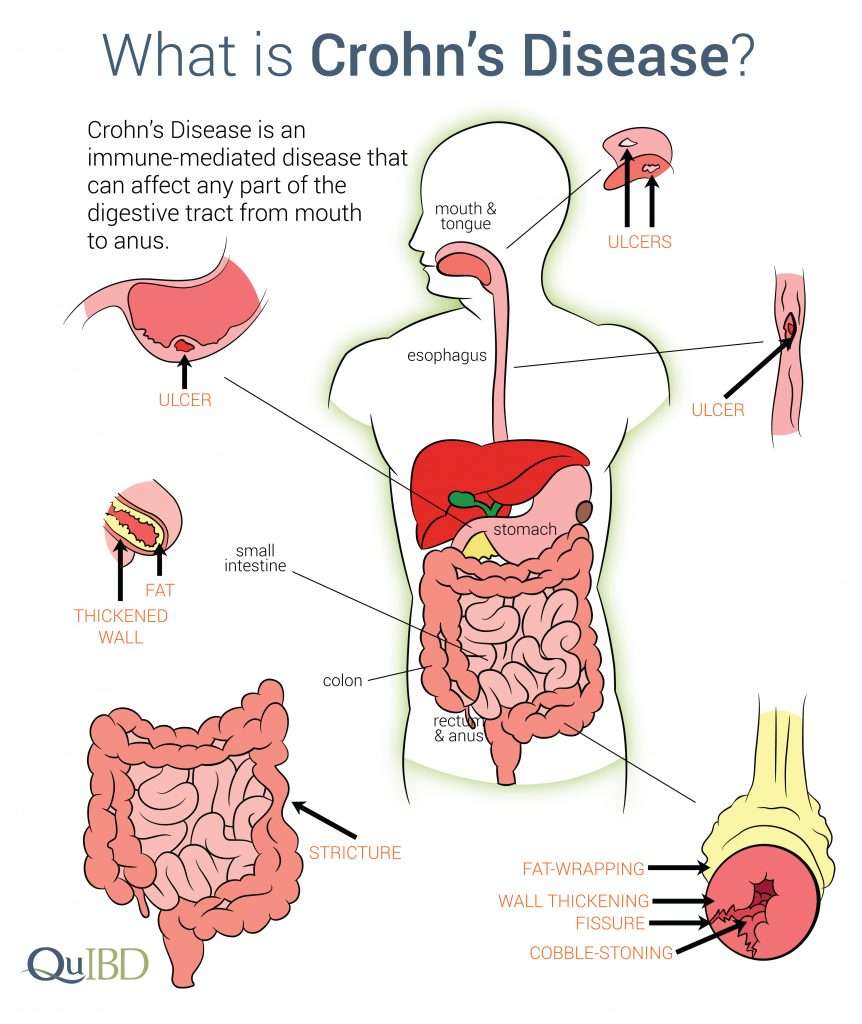
Arthritis means inflammation of joints. Inflammation is a body process that can result in pain, swelling, warmth, redness and stiffness. Sometimes inflammation can also affect the bowel. When it does that process is called inflammatory bowel disease . IBD is actually two separate diseases: Crohns disease and ulcerative colitis.
Recommended Reading: Low Fodmap Diet Ulcerative Colitis
How Do You Get An Ulcerative Colitis Diagnosis
One important thing to note is that people with more severe cases of ulcerative colitis are at an increased risk of developing colon cancer and other serious health conditions, like liver disease, Rudolph Bedford, M.D., a gastroenterologist at Providence Saint John’s Health Center in Santa Monica, California, tells SELF. Thats why its important to reach out to a medical professional if you do have any of the above symptoms.
However, an ulcerative colitis diagnosis can be challenging because other conditions can mimic symptoms of IBD, like infections or even hemorrhoids, Dr. Sinha says. In terms of differentiating between Crohns and ulcerative colitis, he says, Theres no single test that we have that 100% distinguishes between the two. We rely on the patient history and other information such as radiographic imaging and endoscopy. Doing a colonoscopy, for example, can be one of the most reliable ways to identify IBD and to then distinguish between Crohns and ulcerative colitis.
While a colonoscopy is an effective tool, Dr. Sinha clarifies that its not the only way. Rather, theres an entire constellation of tests and data that can be considered, including imaging, lab tests, and a detailed intake of the patients symptoms and presentation.
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I cant bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I cant fully stand upright sometimes for a minute or so. Its frustrating.
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Also Check: How To Prevent A Pressure Ulcer
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Living With Ulcerative Colitis Symptoms
Your ulcerative colitis symptoms will likely come and go, with longer periods in between flares when you may not experience any discomfort at all. Those periods are called remission, and they can span months or even years. Because there is not yet a cure for ulcerative colitis, your symptoms will eventually return.
Ulcerative colitis is an unpredictable disease, and the length of periods of remission between flares can make it difficult for doctors to evaluate whether your course of treatment has been effective or not.
Also Check: Can You Take Imodium If You Have Ulcerative Colitis
Is Pain Normal In Ulcerative Colitis
While less of a central feature than in Crohns disease, a common symptom of this condition is abdominal pain. While there may be specific triggers for the onset of this pain or stomachache, it is often resolved by a bowel movement.
It is more common for the abdominal pain in Ulcerative Colitis to be more extreme in those with a type of Colitis termed pancolitis. This is where the entire large intestine is inflamed.
If this pain becomes more acute in nature and the individual has a raised temperature testing may be required. A CT scan of the stomach/ abdomen may be used to rule out any of the complications of this disease.
Ulcerative Colitis can be classified into 3 main groups. Mild, moderate and severe. This is based on the Truelove-Witts criteria.
- Phase 1 Soft, well-cooked or cooked then pureed foods, no seeds
- Phase 2 Soft Textures: well-cooked or pureed foods, no seeds, choose floppy or tender foods
- Phase 3 May still need to avoid stems, choose floppy greens or other greens depending on individual tolerance
- Phase 4 If in remission with no strictures
Once inflamed, the gut lining becomes very sensitive. This leads to high fibre foods being too rough for the gut. This dietary approach takes this into consideration. Phase 1 is low in fibre with all foods pureed and as symptoms calm the stages are worked through, gradually relaxing and expanding the diet .
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
Read Also: Is Pepcid Good For Ulcers
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Recommended Reading: How Do You Treat A Foot Ulcer
What Are The Complications Of Ulcerative Colitis
Colon Cancer
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Other Complications
If You Have Moderate To Severe Ulcerative Colitis

In 2020, the American Gastroenterological Association released updated treatment guidelines for adults with moderate to severe UC.
The AGA suggested that people whove never received biologics before should only receive tofacitinib if theyre a part of a clinical study or registry study.
The organization also recommended that people whove never received biologics before choose infliximab or vedolizumab instead of adalimumab .
Adalimumab isnt as effective as the other two biologics. However, people with UC can administer adalimumab to themselves, while healthcare professionals have to administer infliximab and vedolizumab. If youre looking for convenience over efficacy, its fine to choose adalimumab instead.
Recommended Reading: Can Ulcerative Colitis Cause Body Aches
Ulcerative Colitis And Joint Pain
When you have ulcerative colitis , its normal to have pain in your abdomen, along with diarrhea and other gastrointestinal symptoms.
Up to 30 percent of people with UC also have arthritis, which is characterized by swollen, painful joints.
Heres a look at the connection between UC and joint pain, as well as what you can do to protect your joints if you have UC.
When You’re In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Don’t Miss: What Can Cause Ulcerative Colitis Flare Ups
How Does Ibd Affect Other Parts Of The Body
IBD can also cause problems outside the gut. Some people with IBD develop conditions affecting the joints, eyes or skin. These can be known as extraintestinal manifestations and often occur during active disease, but they can develop before any signs of bowel disease or during times of remission. Many of these are not very common.
JOINTS
Inflammation of the joints, often known as arthritis, is a common complication of IBD.
It is most common in those with Crohns Colitis and also affects about one out of 10 people with UC.
The inflammation usually affects the large joints of the arms and legs, including the elbows, wrists, knees and ankles. Fluid collects in the joint space, causing painful swelling, although pain may occur without obvious swelling. Symptoms usually improve with treatment of intestinal symptoms, and there is generally no lasting damage to the joints. A few people develop swelling and pain in the smaller joints of the hands or feet. This may be longer lasting and persist even when the IBD is in remission.
Sometimes, the joints in the spine and pelvis become inflamed a condition called ankylosing spondylitis . This can flare-up independently of IBD. It often causes pain over the sacroiliac joints, on either side of the lower part of the spine. Stiffness and pain in the spine itself may eventually lead to loss of flexibility.
SKIN
Some complications are related to the liver and its function.
BLOOD CIRCULATION
Dietary Modifications For Uc Pain
There is no single diet that will work for everyone with UC. Thats why its important to have a very clear conversation with your doctor about what foods you seem to tolerate, especially during a flare of your symptoms. There are some foods that may make your symptoms worse, according to the Crohns and Colitis Foundation. These include foods that are hard to digest such as seeds, nuts, broccoli, and cauliflower. You may also want to experiment by reducing your intake of high lactose foods such as milk and cheese to see if these are making your pain worse. Eliminating foods high in sugar and fat may also provide some relief.
Don’t Miss: Hind Gut Ulcers In Horses Treatment
When Should You Call Your Doctor
If youre experiencing certain symptoms, chances are, your current treatment is not working and its time to consider a change in therapy, says Ha. Call your doctor if:
- Cramping is severe
- Youre experiencing a significant amount of abdominal pain that requires medication
- You have a fever that lasts longer than a couple of days
- You experience nausea or vomiting
- You have ongoing diarrhea or blood in your stool
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
You May Like: Stage Iv Sacral Decubitus Ulcer
Back Pain And Ulcerative Colitis
| | |
Research indicates that nearly 25 percent of people with inflammatory bowel disease including ulcerative colitis and Crohns disease experience chronic lower back pain. Ankylosing spondylitis and axial arthritis both of which can cause back pain are two common causes of back pain for people with UC.
That said, a doctor may not suspect that a person with back pain has UC unless they also experience gastrointestinal symptoms. If you do experience back pain, its important to let your doctor know even if you dont suspect its related to UC. They will be able to determine the cause of your pain and work with you to find the best way of managing it.
A person having backaches may not realize theyre related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
Whats The Connection Between Ibd And Joint Pain
IBD and inflammatory arthritis are both thought to be autoimmune conditions, in which the bodys immune system mistakenly mounts an attack on its own healthy tissues. Its common for two or more autoimmune diseases to occur at the same time. For instance, rheumatoid arthritis is a typical comorbidity for people with IBD. Other types of arthritis, such as enteropathic spondylitis, are also associated with gastrointestinal disease.
Recommended Reading: Best Treatment For Stage 3 Pressure Ulcer
Read Also: What Kind Of Doctor Treats Ulcerative Colitis