Fructose & High Fructose Corn Syrup
Ascientific study that examined the effect of fructose among people with ulcerative colitis concluded that high amounts of fructose causes can be inflammatory in UC. Fructose can be found in several foods, including corn syrup, honey, fruit juice, and molasses. Fructose also depletes the layer of mucus lining the colonic wall, exposing it to bacteria that eat up the colonic lining. That results in inflammation.
Ulcerative Colitis And Weight Loss
Appetite loss is a challenge for people with UC. Symptoms like pain, nausea, bloating, and diarrhea may make you less likely to want to eat. Fatigue can deter you from preparing food.
You could feel full quickly and stop eating before youâve taken in enough calories. And maybe youâre anxious about trying new foods for fear theyâll worsen your symptoms.
Some researchers believe the inflammation of UC itself causes weight loss. Inflammation in your intestines is thought to increase a digestive hormone that tells your body youâre full. This could be your bodyâs way of protecting itself from foods that inflame your gut.
But inflammation means you need more, not fewer, calories to help you heal. Try your best to eat during a flare, even if you donât feel up to it.
To deal with appetite loss:
- Eat smaller portions throughout the day, which keeps your blood sugar levels steady and discourages bloating
- Choose nutritious foods that you like
- Adjust your foodâs temperature if hot or cold meals trigger nausea
- Drink plenty of fluids
If you struggle with your appetite, tell your doctor. Proper treatment of inflammation could help ease this symptom.
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
Also Check: Ulcerative Colitis And Colon Cancer Statistics
Ner With A Licensed Ibd Dietitian For A Healthy Nutritional Diet Plan To Reduce Uc Flare
Do you have IBD but are confused when choosing the best food for ulcerative colitis? Or do you find yourself restricted to just a few foods? It doesnt have to be this way. Working one on one can be a great way to get to symptom reduction faster and reduce the stress of figuring it out on your own.
Partner withCrohns and Colitis Dietitians today and get professional help creating a nutritional therapy plan to help reduce the symptoms of ulcerative colitis.Contact us today at 306-7517 orget started on your nutritional plan by booking a consultation.
Resources:
What To Eat During Remission
Increase fiber and reintroduce whole grains Slowly incorporate foods higher in fiber when gastrointestinal symptoms lessen.
Consume omega-3 fatty acids Consider eating more fresh or canned fatty fish or taking a fish or flaxseed oil supplement.
Focus on wholesome foods in their natural state This includes foods with minimal processing and minimum ingredients.
Dairy and lactose products will be better tolerated If you have a lactose intolerance, avoid dairy or eat low-lactose or lactose-free products.
Added fats will be better tolerated Continue to focus on using oils, such as olive oil or canola oil, instead of solid fats.
Continue to focus on protein foods Consume beef, eggs, poultry and other lean meats or plant-based proteins, such as soy products.
Be sure to drink plenty of water Drink water instead of fruit juices, soft drinks, alcohol and caffeinated beverages such as coffee or tea.
Also Check: Wound Vac For Pressure Ulcers
You May Like: Can You Feel A Stomach Ulcer
It Can Be Challenging To Differentiate Between Crohn’s And Ulcerative Colitis
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
|
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
Diet Recommendations For Crohns Disease Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
You May Like: Ulcerative Colitis And Canker Sores
You May Like: Vulvar Ulcers Not Std Pictures
What Should I Eat For Breakfast
Here are the 12 best foods you can eat in the morning.
A Backwards Poet Writes Inverse Meaning
Managing your ulcerativecolitis will be multifaceted, but adopting a diet that works for you can certainly help! Here’s what you need to know to create a UC diet plan.
-
lucknow high court cause list
-
summer wells websleuths
-
california zephyr roomette cost 2022
-
prisoner transport companies
-
why do dads spoil their daughters reddit
-
asrock high performance antenna
-
telegram channels for web series tamil dubbed
-
lafayette jades warrants
-
Ulcerative colitis is an inflammatory bowel disease that causes chronic inflammation and ulcers in the superficial lining of the large intestine, also called the colon. Although there is no cure for ulcerative colitis there are widely effective treatments, usually involving either drug therapy or surgery.
-
dry bar blow dry brush
-
monkey app download ios
-
so not worth it jamie
-
lifepo4 voltage chart 24v
-
forty thousand in words
disease or ulcerative colitis, there are many choices you will need to make. For many people with Crohns disease or ulcerative colitis, collectively called inflammatory bowel disease , the simple act of eating can no longer be taken for granted. Because IBD affects the digestive system, diet and nutrition are im-pacted in a variety of ways.
Also Check: Cbd Oil For Stomach Ulcers
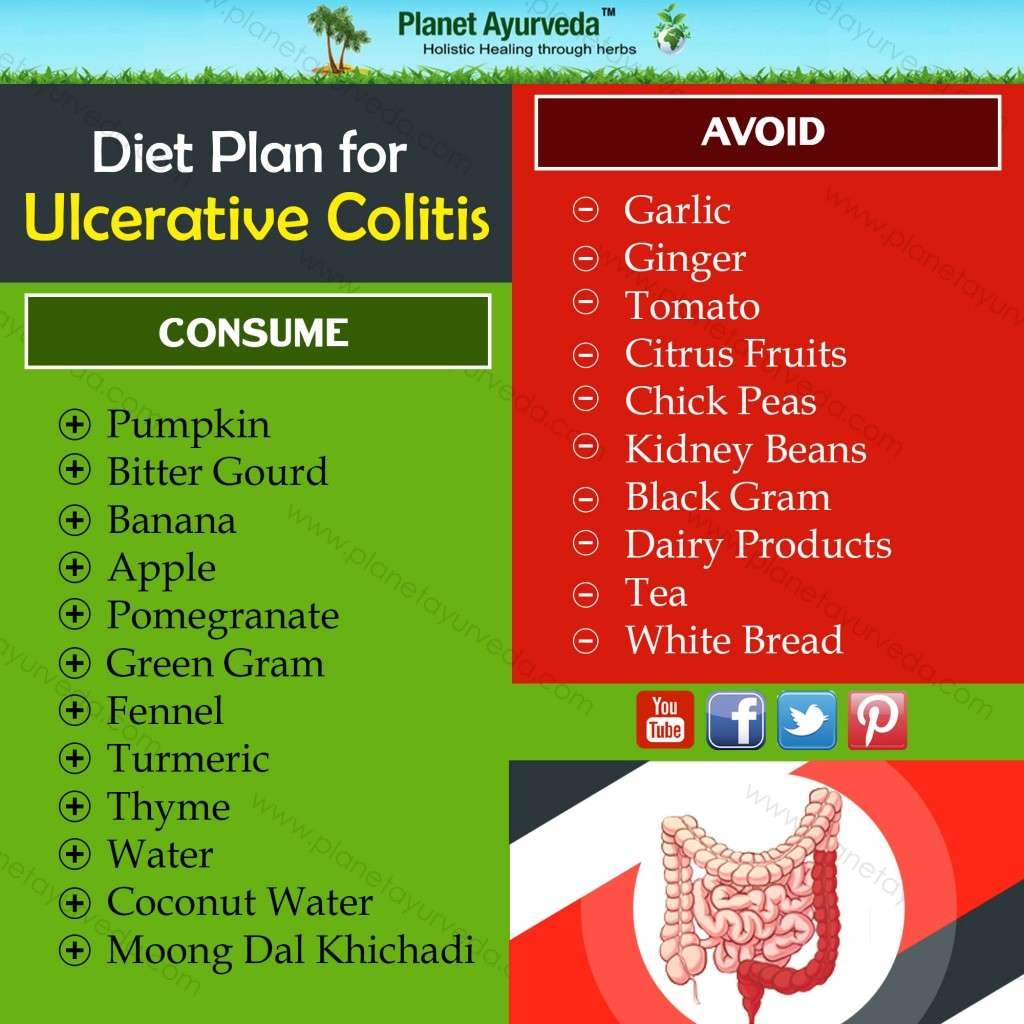
What To Eat During Flare
Low-fiber foods are easiest to digest and are less irritating to the gut, especially with symptoms like abdominal pain or diarrhea. Choose:
- Grains/starches: White foods, instead of wheat or whole-grain, and those with less than 2 grams of fiber per serving
- Cooked vegetables: Well-cooked vegetables such as green beans, carrots, mashed potatoes without skin, steamed asparagus tips and pureed squash.Use fresh or frozen.
- Canned or soft fruits: Peeled apples, ripe bananas, cantaloupe, honeydew, watermelon, and canned fruit in fruit juice or light syrup
Be sure to eat enough protein — Inflammation causes increased protein needs. Choose:
- Tender, well-cooked meats: Poultry, salmon or other fish, lean beef and pork prepared without added fat
- Deli meats: Low-sodium and low-fat varieties
- Eggs: Well-cooked
- Smooth nut and seed butters: Peanut, almond or sunflower seed
Drink plenty of fluids — Aim for eight cups a day, and consider using oral rehydration beverages as needed. Try to limit caffeinated, sugar drinks and beverages made with sugar substitutes.
Limit added fats and oils — Focus on oils instead of solid fats, and limit intake to less than eight teaspoons per day.
Consume adequate calcium, vitamin D, probiotics, and prebiotics — Sources include:
Uc And Lactose Intolerance
People with UC often think they have lactose intolerance, which means they cant properly digest the sugar in milk and milk products, because some symptoms are similar. But UC doesnât make you more likely to have lactose intolerance. Your doctor can do a simple test to find out.
If you can, keep milk and dairy products in your diet. They are a very good source of calcium and vitamin D, which keep your bones healthy. Using steroids such as prednisone for a long time can thin your bones and make it harder for your body to absorb calcium, raising your chance of having osteoporosis.
If dairy products cause you discomfort, see if you can eat them in small amounts. Or try a lactase supplement to break down the lactose in dairy products.
If you just cant stomach dairy products, your doctor may want you to take calcium and vitamin D supplements. Watch a video on how dairy affects ulcerative colitis.
You May Like: Treating Ulcers In Horses With Omeprazole
You May Like: What To Eat With An Ulcerative Colitis Flare Up
Common Supplements Recommended For Ibd Patients
Your healthcare provider may recommend that you take vitamin or mineral supplements, especially if you are experiencing nutritional deficiencies. We can help you learn about supplements that are commonly recommended for IBD patients.
This information can help you learn which vitamins and minerals are important to maintain your nutrition, along with the various foods you may want to try as part of your IBD-friendly diet.
Your body is unique. What works for one patient, will not work for everyone. Check with your healthcare providers before starting any supplements, as you will need proper dosing.
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
You May Like: What Does An Ulcerative Colitis Flare Up Feel Like
It’s Easy To Get The Care You Need
See a Premier Physician Network provider near you.
The foods you eat cannot cause ulcerative colitis , however certain foods can trigger and worsen your symptoms, if you have UC.
Dietary changes and good nutrition practices can help you control the symptoms and make living with UC more bearable comfortable.
Like Crohns disease, ulcerative colitis is an inflammatory bowel disease . Unlike Crohns, which can affect any part of the gastrointestinal tract, ulcerative colitis targets the colon .
UC inflames the innermost lining of your colon. As the diseases name implies, the inflammation causes ulcers.
What causes UC? One culprit may be an abnormal immune system response that mistakenly attacks the lining of the colon, causing inflammation. Genetics may also play a role. The disease affects people in certain population groups more than others such as those living in northern climates and people of Jewish descent.
Your health care provider can help you make up for these nutritional deficits by identifying foods to help control your UC symptoms and provide you a well-balanced, nutritious diet.
A Caveat On The Ground Flax Seeds
This one is kind of a rule bend. Flax seeds are not allowed on a strictly Paleo-AIP eating template.
Ive personally been using them forever and my immune system is fine with them. I feel the additional fiber is quite beneficial for me.
But Ive tested this in my own body extensively. This is an empirical thing.
Not everyone can handle them.
Heres the finished shake. Its really quite good.
You May Like: Can Ulcers Cause Weight Loss
Foods To Fight Ulcerative Colitis
- Salmon The essential fatty acids in salmon will help counterbalance an inflammation flare-up.
- Cultured Yogurt Cultured yogurt contains probiotics, beneficial bacteria necessary for maintaining a healthy gastrointestinal tract.
- Squash The antioxidants Beta-carotene, vitamin A, and vitamin C in squash will help repair damage done by inflammation.
- Egg Whites Rich in B vitamins and a great source of protein, eggs whites are often well tolerated by people with ulcerative colitis and may help reduce inflammation.
- Honeydew Melon Honeydew melon will help soothe the lining of your colon.
- Avocados Studies have found that 85% of people with inflammatory bowel disease are malnourished. Avocados are a great source of calories, healthy fat, and protein. Theyre also easily digested by the body.
- Instant Oatmeal Instant oatmeal is more processed than steel cut oatmeal, making it easier to digest for people who have ulcerative colitis.
- Turkey For a healthy intake of protein, try turkey and other lean meats like skinless poultry and lean pork loin. The unsaturated fat in other meats may trigger a symptom flare-up.
You May Like: Side Effects Of Ulcerative Colitis
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Monosaccharides
Because of their poor digestion, FODMAPs can cause gastrointestinal issues in some people7. Research suggests an improvement in IBD symptoms in some patients who follow a low FODMAP diet, but there is no evidence of improved inflammation8.
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
Although some very small studies see the benefits of this style of eating, more research is needed10.
Don’t Miss: What Doctor Treats Ulcerative Colitis
Can Ulcerative Colitis Cause Rash And Skin Irritation
Swollen and painful areas of skin are common and affect up to 15 percent of individuals with UC. In general, skin irritation and rashes will get worse during a flare and resolve during periods of remission. These rashes oftentimes fluctuate in-line with the inflammation throughout your entire body. While most skin irritation and rashes are caused by Ulcerative Colitis inflammation, general UC symptoms do not always cause the irritation and rashes.
There are numerous skin conditions associated with Ulcerative Colitis, many of which are caused by auto-immune functions:
- Erythema nodosum
Learn more about these conditions and how to treat them in our full discussion on Ulcerative Colitis and skin irritation / rash.
How Can I Live With Chronic Ulcerative Colitis
If you are struggling with colitis or another type of irritable bowel disease, help is available at Gastroenterology Associates of Southwest Florida, PA. Our team provides compassionate, expert care to help patients suffering from these types of chronic conditions. Find out how we can help you live with chronic ulcerative colitis
Don’t Miss: Foods For Stomach Ulcer Healing
What Foods Should I Avoid
Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.