Dietary Advice For Ulcerative Colitis
Please note, this page is printable by selecting the normal print options on your computer.
What is Ulcerative Colitis?
Ulcerative Colitis is a form of Inflammatory Bowel Disease . IBD is a term used to cover a number of inflammatory conditions of the gastrointestinal tract. UC causes inflammation in the large bowel and can affect the rectum, part of, or the entire colon. If you have UC this diet sheet may help you.
Can diet help?
Diet is not a cause of UC however diet can help to relieve symptoms such as diarrhoea during a flare up and maintain good health including healthy bones. You may find as time goes by you begin to notice that certain foods aggravate your symptoms of UC and so they are best avoided. However, do not remove whole food groups as this could mean you lose some vital nutrients. The main food groups are demonstrated below in the Eatwell Guide.
What foods are beneficial for UC during a flare up?
Soluble FibreDietary fibre can be categorised into two forms, soluble and insoluble. Soluble fibre is partially digested in the large intestine to form a glue like substance, which helps to produce soft/formed stools, without causing inflammation. Examples of foods rich in soluble fibre are:
- Oats e.g. Porridge oats/Ready Brek ®, oatcakes
- The body of fruits and vegetables e.g. peeled apples and pears, tinned fruit, peeled root vegetables such as carrots, parsnips, turnip
What foods may worsen UC during a flare up?
Dairy foods
Spicy foods and fatty foods
Avocado And Hummus Spreads: Superfood Crohns Snack Options
Avocado is known as one of the best superfoods for people with Crohn’s disease and other IBDs. It’s loaded with healthy unsaturated fats and numerous nutrients like potassium, magnesium, vitamin C, and vitamin E. They’re one of the few fruits that are easy to digest and tolerate. Besides, avocados are super versatile, and you can have them in many ways: pure, spread, guacamole, smoothie, etc.
Hummus is another great snack idea recommended by the Crohns Colitis Foundation itself. This chickpea spread is highly nutritious and generally well-tolerated by people with IBDs. Just make sure you choose the right crackers under your spreads. If you’re going through a flare, avoid high-fiber bread and prefer options like melba toasts, rice crackers, or plain pretzels for example.
Omelet Cups Pack A Protein Punch
Protein is one of the key nutrients that someone with UC needs. For this grab-and-go snack, simply add a few cooked veggies to the bottom of a muffin tin and top with whisked eggs. Bake in the oven at 350 degrees until theyre set and stick them in the refrigerator or freezer so that you can grab one on the way out the door. This is a quick-and-easy way to get in some much needed protein, fiber, vitamins, and minerals.
Don’t Miss: Humira Treatment For Ulcerative Colitis
Snack Ideas For Ulcerative Colitis Healthline
- Highest rating: 5
- Lowest rating: 1
- Summary: 10 Snack Ideas for Ulcerative Colitis · 1. Greek yogurt topped with cantaloupe or honeydew melon. Yogurt is a good source of probiotics. · 2.
- Match the search results: 10 Snacks for Ulcerative Colitis That Are Safe and HealthyEating can be tricky when you have ulcerative colitis. Some foods can trigger symptoms. You also have to be mindful that
Food Journaling And Different Diets
After they told me to find out for myself, I started writing a food journal.
Every day, I’d write down in detail what I ate during the day. Every meal, every snack, every drink. It is time-consuming but it is the perfect way when you have absolutely no idea what exactly it is that triggers your intestins.
I googled a lot of stuff too and bought different books regarding diets for that specific disease on Amazon.
And I found this one : eating healthy with Crohn & Ulcerative Colitis
I would not recommend it if it were bad. It really helped me a lot! I bought this back in 2014 and I still use it sometimes to try some of the recipes.
Sure, there are probably lots of them on the market now as the IBDs get more and more attention but back then, this was one of the few I could find.
Yes, this is an affiliate link. So yes, I do earn a tiny percentage if you buy it through the link.
I could also just put an ad here with random Crohn& Colitis cookbooks in English to have a farther reach and more earnings on Amazon.
But I won’t as I really just want to link stuff on this blog that I personally find useful.
This book contains detailed information about both diseases, why we have them and how they develop. Apparently that particular book got an update already as there are more and more studies on IBDs.
The general tips regarding food rules still apply, though.
- You’re having a major flare-up
- You’re flaring but it is calming down
- You’re not having symptoms or are in remission
You May Like: What Are The Symptoms Of Having An Ulcer
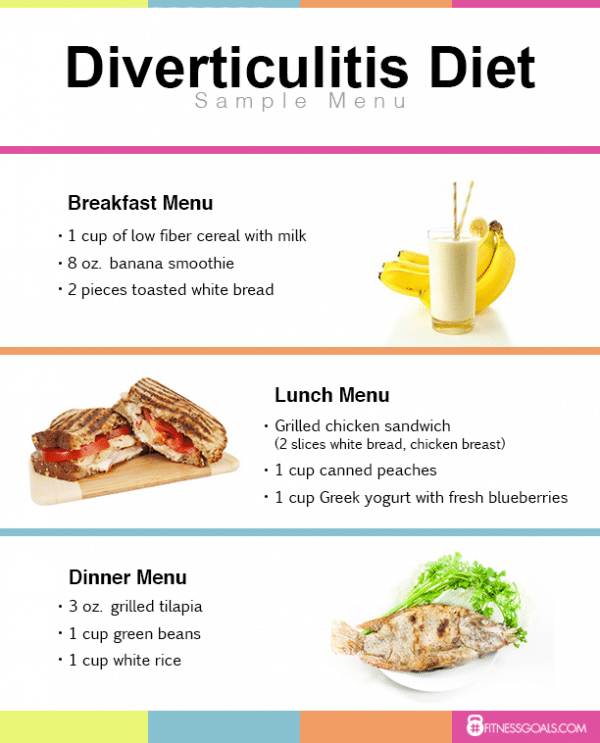
Cereal With Low Fat Milk
High fiber bran and wheat cereals could set off a bout of diarrhea and other ulcerative colitis symptoms. But you dont have to cross cereal off the snack list. Its still a good source of vitamins and minerals.
You do want to choose your cereal wisely, though. Lower fiber options like corn flakes and rice puffs are easier on your gut.
Yogurt is often easier on your gut if lactose causes ulcerative colitis symptoms. Or opt for a dairy alternative like soy or rice milk. Top your bowl of cereal with sliced bananas to ramp up the nutrition.
Toasted Potato Bread With Scrambled Eggs And Spinach
Whole-grain foods are a good source of fiber, which normally helps reduce constipation and supports overall health. The high levels of fiber in whole grains may be hard to digest during an ulcerative colitis flare.
Potato or sourdough bread is usually easier to tolerate for people with ulcerative colitis. Top with scrambled eggs for a good source of protein.
Add sautéed spinach for a healthy dose of iron.
Don’t Miss: Venous Stasis Ulcer Signs And Symptoms
The 3 Key Goals Of Uc Treatment
There are treatments available that can help control excess inflammation in order to help you:
Controlling inflammation can help relieve UC symptoms such as frequent and urgent bowel movements, bloody stools, and abdominal pain.
Controlling inflammation can also help you achieve and maintain remission. This means you have achieved ongoing symptom relief and are able to prevent flares.
Controlling inflammation over time allows the lining of the colon to heal and can help you maintain remission.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
Recommended Reading: What Causes Ulcers In Your Stomach
Don’t Miss: Suggested Diet For Ulcerative Colitis
What Is The Best Medicine For Ulcerative Colitis
Treatment strategies for ulcerative colitis vary from person to person. Your doctor will base recommendations for medication on the intensity of your symptoms and severity of the disease. Drugs may be given as combination therapy or single drug therapy.
There are 6 types of medication used to treat UC.
Table: Medications for ulcerative colitis
| Drug | |
|---|---|
|
Oral and rectal |
|
Prescribed when previous medications are not effective |
|
| FDA-approved to treat moderate to severe | Oral |
| Monthly shot or intravenous in a hospital setting | |
|
If your body stops responding to medications or if you have emergency complications, you may need to undergo a surgical procedure to remove the affected part of the colon.
Read Also: Sacral Decubitus Ulcer Icd 10
Foods To Avoid During A Flare
Now that you know the best foods to eat for colitis, it is also good to know what foods you need to avoid, especially when you are experiencing a flare. Many people go into remission and do not experience any flare-ups in several months, or even years. But flare-ups can still happen anytime so it is important to know how to manage your condition.
Some of the symptoms you may experience during a flare include diarrhea and abdominal pain. While the best thing to do during a flare is to follow your doctor’s’ instructions, there are still some things you can do.
One of the foods you should not eat during a flare-up is fiber-rich foods. Normally, we think of fiber-rich foods as healthy, but in the case of those suffering from colitis, it is not advisable.
A high-fiber diet will assure that your bowel movement will increase. If this happens, it can actually trigger a flare-up. Some of the foods that are rich in fiber include bread, pasta, and cereals.
Spicy foods should also be avoided, along with dairy, especially if you are lactose intolerant. Nuts and fruits are also not recommended unless they have been peeled , or the canned variety.
What you can actually do is to keep a food diary. Doing this will help you identify the foods that are actually triggering your flares. You can them make changes to that there is less chance of a relapse.
Read Also: Is Ulcerative Colitis Caused By Stress
Food Prep And Meal Planning
Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
Ulcerative Colitis Nutrition Must

Nutrition is vital in managing ulcerative colitis symptoms, andpeople with this condition must follow a balanced diet and consume enough nutrients.
Foods to eat if you have ulcerative colitisinclude the following.
#1: Protein
Inflammation caused by ulcerative colitis increases your body’s protein requirements. Protein deficiency can damage your body’s ability to heal and may lead to muscle loss.
There are many foods rich in protein, including:
Following are some tips for identifying food triggers and staying on track.
You May Like: Early Symptoms Of Ulcerative Colitis
Great Snacks For Crohns Disease Ibd And Ulcerative Colitis
Snaking and eating on the go can be challenging when you live with an inflammatory bowel condition like Crohns disease. While you dont always have what you need on you, youre often scared of trying new foods that may cause pain.
Each individual living with IBDs has his or her own particular tastes and food tolerances. Whether you’re craving sweet or salty, weve gathered here 10 Crohns snack ideas that work well for most people.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Recommended Reading: Where Do You Feel Stomach Ulcer Pain
Cabbage Celery And Brussels Sprouts
Avoid eating cabbage, celery, and Brussels sprouts because they are high in fiber and potential colon lining irritants. Instead, have sweet potato, potato, carrots, and squash.
NOTE: Dairy is not mentioned in this list because a few people do not get ulcerative colitis flare-ups while others do. So, check with your doctor to find out if you can consume dairy products.
It may seem like you have run out of options to eat, but thats not the case. Here is the list of foods that you can eat.
Dont Miss: Is Alcohol Bad For Ulcerative Colitis
Apple Sauce: A Safe Food To Eat After A Flare
While raw fruits are not recommended for people with inflammatory bowel conditions, cooked fruits without peel are fine most of the time. Apple sauce is easy to digest and is a safe food to have after a flare-up. On the nutritional level, its packed with nutrients including potassium and vitamin C.
If youre at home, cooking your own apple sauce is the healthiest thing you can do. For travelers, workers, and adventurers, apple sauce pouches are super convenient, and you can find them in literally any store!
Read Also: Best Alcohol To Drink With Ulcerative Colitis
Bananas: The Best Crohns Disease Fruit Snack For Outdoor Adventurers
Fresh and raw fruits are loaded with fibers. Despite their high nutritional value, most people with Crohn’s disease have no choice but to eliminate them from their diet. Raw fruits are known to aggravate symptoms during a flare and often cause diarrhea.
Bananas make the exception in most cases. Theyre one of the rare fruits people with Crohns disease and IBDs report as easily digestible. And theyre just great for travels and outdoor adventures as you just pop one or two in your bag and go. Banana smoothies are a great alternative.
From One ‘specialist’ To The Next: Starting The Journey
When the first bad symptoms of the disease appeared, I went to see a specialist who diagnosed ‘Irritable bowel syndrome‘.
So he told me to just ‘pay attention to what you eat’. Well, okay then.. let the food odyssey begin.
I went to see another doctor who told me to cut out meat.
The next one told me to eat lots of sauerkraut. Seriously!!
That last one was the funniest one. Especially since sauerkraut makes me bloated and causes cramps – any kind of cabbage does that .
Also Check: Stomach Ulcer And Chest Pain
How Is Treatment The Same And Different
In both conditions, treatments usually involve medications or, sometimes, surgery. In severe cases, your doctor may recommend a combination of the two to bring your symptoms under control. Certain over-the-counter medications may ease some of your pain-related symptoms. These include:
- Anti-diarrheal medications
- Iron supplements, especially if youâre bleeding
UC treatments may include:
Anti-inflammatory drugs. This is usually the first line of treatment. This can include drugs like 5-aminosalicylates and corticosteroids. Some newer drugs like sulfasalazine and 5-ASAs , which are called âsteroid-sparing,â can be safely taken long-term. Your doctor may not want you to take steroids long-term because of their side effects.
Immunosuppressant drugs. This helps to reduce inflammation in your colon and cut down the immune response that might attack your digestive cells.
Biologics. This targets the proteins made by your immune system.
Surgery. About 30% of people who have UC need surgery. Itâs sometimes the only cure, especially if medications donât ease your symptoms or they become too difficult to manage. Your doctor may consider a surgery called proctocolectomy.
In this procedure, your entire colon and rectum are removed. Most surgeries also involve a procedure in which your doctor will attach a pouch at the end of the small intestine or outside your body to pass poop directly into it.
Diverticulitis treatments may include:
Uc And Lactose Intolerance
People with UC often think they have lactose intolerance, which means they can’t properly digest the sugar in milk and milk products, because some symptoms are similar. But UC doesnât make you more likely to have lactose intolerance. Your doctor can do a simple test to find out.
If you can, keep milk and dairy products in your diet. They are a very good source of calcium and vitamin D, which keep your bones healthy. Using steroids such as prednisone for a long time can thin your bones and make it harder for your body to absorb calcium, raising your chance of having osteoporosis.
If dairy products cause you discomfort, see if you can eat them in small amounts. Or try a lactase supplement to break down the lactose in dairy products.
If you just can’t stomach dairy products, your doctor may want you to take calcium and vitamin D supplements. Watch a video on how dairy affects ulcerative colitis.
Also Check: Topical Treatment For Decubitus Ulcer