Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
Read Also: What Foods To Eat For Ulcerative Colitis
Diet Progression Following Flares For Ulcerative Colitis And Crohns Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
What About A Low Fodmap Or Other Diets
FODMAP stands for fermentable oligosaccharides, di-saccharides, mono-saccharides, and polyols. They are the carbohydrates found in foods and they draw water into the colon, which can make you feel bloated and uncomfortable. FODMAPs also dont pass through your gut quickly but can ferment and hang around for a time, which can cause colitis symptoms.
FODMAPs include:
- Any foods with lactose, or dairy ingredients
- Foods with fructose, including natural fruits, honey, or processed high-fructose corn syrup
- Fructans like garlic, onions, or wheat
- Galactans, which are beans, lentils, or soybeans
- Polyols such as fruits with seeds like apples, avocados, cherries, figs, and peaches
There are other types of diets such as a specific carbohydrate diet that cuts starchy potatoes and grains. Some people have found relief on a Mediterranean diet that includes vegetables, whole grains, fruits, fish, and poultry. A gluten-free diet could also lessen your symptoms.
Also Check: Dakin’s Solution For Pressure Ulcers
What Should I Eat If I Have Ulcerative Colitis
If you have ulcerative colitis, you should eat a healthy, well-balanced diet. Talk with your doctor about a healthy eating plan.
Ulcerative colitis symptoms may cause some people to lose their appetite and eat less, and they may not get enough nutrients. In children, a lack of nutrients may play a role in problems with growth and development.
Researchers have not found that specific foods cause ulcerative colitis symptoms, although healthier diets appear to be associated with less risk of developing IBD. Researchers have not found that specific foods worsen ulcerative colitis. Talk with your doctor about any foods that seem to be related to your symptoms. Your doctor may suggest keeping a food diary to help identify foods that seem to make your symptoms worse.
Depending on your symptoms and the medicines you take, your doctor may recommend changes to your diet. Your doctor may also recommend dietary supplements.
Read Also: Ulcerative Colitis Lower Back Pain
When Ibd Is Active It May Help To:
-
Limit dairy that is high in lactose.
-
You might be able to handle yogurt with live active cultures or Greek-style yogurts.
-
You might be able to handle hard cheeses like cheddar and Swiss.
-
Try almond or coconut milk, lactose free milk or use lactase pills.
Limit fructose.
Limit high fat foods like butter, cream, red meats, chocolate, fried or fast foods.
Limit high fiber foods like whole grains, beans, and fruits and vegetables with skin.
You might be able to handle fruits and vegetable with skins peeled off.
Lower fiber fruits include cantaloupe, honey dew, mandarin oranges, fruit cocktail, and applesauce. For veggies, try zucchini, yellow squash, and bell peppers.
Try well cooked vegetables and vegetable juice.
Try low fiber grain products like white bread, white rice and pasta and low fiber cereal and crackers.
Caffeine, acidic foods, and alcohol may make flares worse.
It may help to keep a food log. Your dietitian can review your food log with you and help figure out food triggers as well as foods that may improve your symptoms.
Recommended Reading: What To Eat To Help Stomach Ulcers
Read Also: Ulcerative Colitis Long Term Prognosis
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohns disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
What Should I Eat And Drink
Eat a high-calorie, high-protein diet. Strive for a balanced diet with foods from all food groups .
The food you eat should be based on what you like and what your body can handle.
Lactose intolerance is common in people with Crohns disease, but some people do not have issues when eating dairy products.
Try eating smaller, more frequent meals and snacks
If it is painful to eat or you are losing weight, try supplements like Boost, Ensure, and Breakfast Essentials .
Your fluid needs are increased with chronic diarrhea and acute flares. Drink more fluids during flares .
When your disease is active, a low-fiber, low-fat diet may reduce symptoms.
Don’t Miss: How Is Ulcerative Colitis Causes
Ulcerative Colitis Diet: What To Eat In A Flare Up
A low residue diet is often recommended to manage symptoms of ulcerative colitis. The Canadian Society of Intestinal Research outlines residue as the solid contents that stay in the bowel after digestion, with the goal of reducing the number of bowel movements that happen in a day. Residue includes fiber, which is limited to 10-15g per day, but the low residue diet differs from the low fiber diet by including foods that may stimulate frequent bowel movement, such as dairy, caffeine, alcohol and gristly or fatty meat.
Dr Deborah Lee, of Dr Fox Online Pharmacy, recommends the following foods for a low residue diet:
- Low fiber fruit and veg such as melon and bananas, as well as stewed fruit
- Lean protein such as white meat, eggs and tofu
- Refined grains such as white bread, white pasta and oatmeal
- Cooked seedless and skinless vegetables such as cucumber, potato and squash.
Cooking your food may also break down some of the dietary fiber to make it more digestible, as seen in a study in the journal of Plant Foods for Human Nutrition , which indicates that the process of cooking decreases the amount of insoluble dietary fiber in some vegetables.
- Related: 4 dairy free diet benefits
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Read Also: Ulcerated Nodular Basal Cell Carcinoma
Quick Tips For Nausea
If youre really having trouble keeping things down, here are a few of my tips:
- Be cautious about how much volume youre putting in and what ingredients you may be substituting. If youâre youâre questioning if youâll be able to keep it down at the rate that its dissolving, or wondering if it may just come right back up and leave you back to where you started ⦠consider this.
- Iâve heard of others using cupcake wrappers to poke through and hold the contents that melt if not consumed quickly enough. Cool, huh? But, eating faster doesnât mean better if youâre vomiting. If you find this to be true, consider putting less in each cube.
- Major nausea hack: In the past, Iâve taken a couple of tablespoons of the purée and placed pureed contents into one corner of a few small Ziploc bags. Freeze that, then cut off a very small tip of the corner of the bag, so when youâre ready to eat one, you can consume it at a slower rate.
Dont Miss: Early Symptoms Of Stomach Ulcer
What Is Ulcerative Colitis
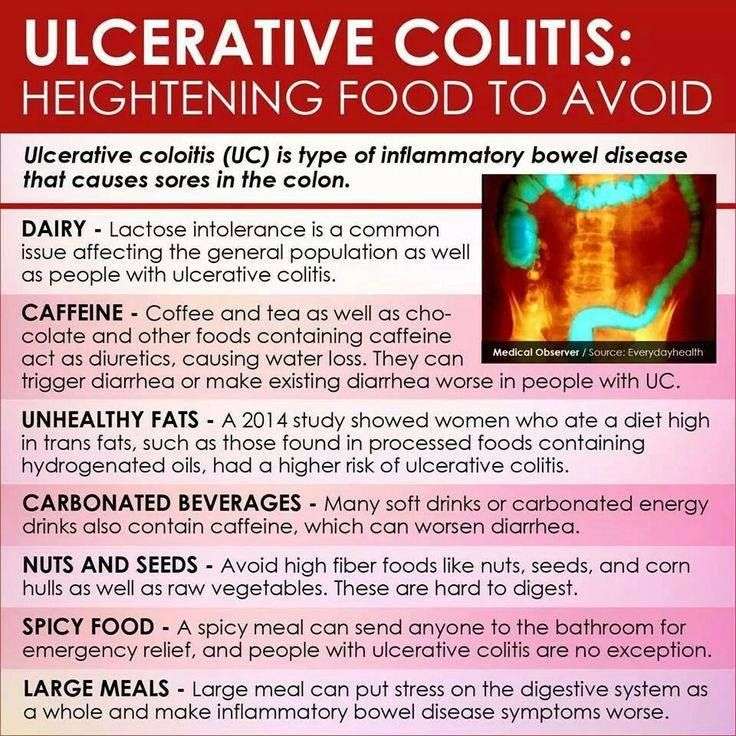
Ulcerative colitis is a condition that causes inflammation and sores on the inner lining of your large intestine and rectum. The exact cause of this medical condition is not known but it is thought to be linked to certain environmental factors such as diet and lifestyle as well as genetic factors. A possible cause is your immune system attacking your digestive system.
Ulcerative colitis can cause symptoms such as abdominal pain, cramping, tiredness, and nausea. Your symptoms can be managed with what you eat, and by not eating certain foods you can reduce your flare-ups.
Even though no eating plan will completely prevent flare-ups, a good diet will help you manage your symptoms. You should be aware that as we are all unique and different, what changes in food and diet work for one individual may not work for another. Your diet plan will need to be tailored to your own unique needs.
Read Also: Lower Left Back Pain Ulcerative Colitis
Inflammatory Bowel Disease Management
Inflammatory bowel disease is not caused, nor can it be cured, by what you eat. Doctors and dietitians agree, however, that food may play some role in the underlying inflammatory process that causes IBD symptoms.
Certain foods may aggravate symptoms, while others may calm them and promote healing. Therefore, paying attention to what you eat and how your body responds to different foods is an important component of a total treatment plan for IBD.
A diet plan can supplement but should never replace medical treatment for IBD. Always take your medications exactly as prescribed by your doctor.
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient.
Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high-calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAP stands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have an intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Dietary choices do not cause ulcerative colitis, but certain foods can trigger and worsen symptoms. Learning to identify trigger foods can help reduce the frequency and severity of ulcerative colitis symptoms.
Don’t Miss: Is Green Tea Good For Ulcers
What To Eat And Avoid To Manage Ulcerative Colitis
To control Ulcerative Colitis, you can start making some simple changes in your lifestyles and food habits which are mentioned below, along with the diet plan for Ulcerative Colitis patients mentioned above:
Dos:
Donts:
Carbonated Beverages May Increase Abdominal Pain
Fizzy drinks may cause gas or bloating in some people, possibly leading to increased abdominal discomfort. Many soft drinks or carbonated energy drinks also contain caffeine, which can stimulate the intestines and worsen diarrhea, according to Mayo Clinic. Drinking sugary soft drinks can contribute to obesity as well, which raises the risk of heart disease and other health problems.
An analysis of drinks published in May 2019 in the journal Medicine found that a high intake of soft drinks was associated with an increased risk of developing Crohns disease, while a high intake of tea was associated with a lower risk of the inflammatory bowel disease. For a refreshing beverage, choose fruit-infused water or herbal iced teas.
Also Check: Classic Features Of Ulcerative Colitis
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
Food Prep And Meal Planning
Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
You May Like: Clinical Manifestations Of Ulcerative Colitis
What Foods Can I Eat
People who are diagnosed with ulcerative colitis are at an increased risk of having deficiencies in their diet because they may not be able to consume certain foods. Difficulty absorbing nutrients from food may also add to this problem. Individuals with ulcerative colitis are therefore advised to eat foods high in vitamins and minerals, calcium, iron, and vitamin A. Foods you may eat include:
- Omega-3-rich foods that are high in omega-3 fatty acids such as sea food. This includes mussels, scallops, anchovies, mackerel, and sardines
- Some probiotic foods yogurts containing active probiotics have been shown to help reduce ulcerative colitis flare-ups and symptoms
- Low-fiber fruits bananas, cantaloupes, and cooked fruits
- Refined grains potato, white pasta, gluten-free bread, white rice, and oatmeal
- Lean protein fish, chicken, eggs, and firm tofu
- Cooked vegetables cucumbers, squash, and asparagus tips
- Water, as diarrhea can lead to dehydration
- Dietary supplements to make sure you get enough nutrients. Consult your dietitian before initiating supplements
- A Low-residue diet or low-fiber diet white bread, refined breakfast cereals, such as cornflakes, white rice, refined pasta and noodles