Differences Between Ulcerative Colitis And Crohns Disease
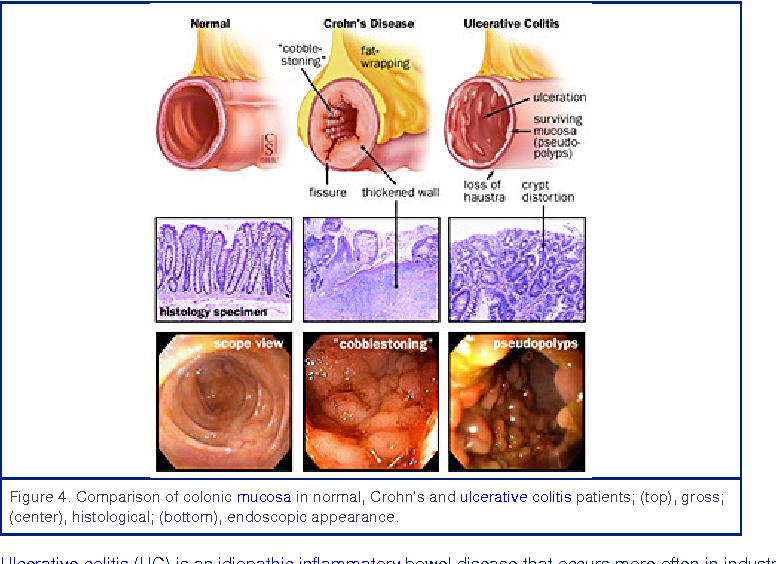
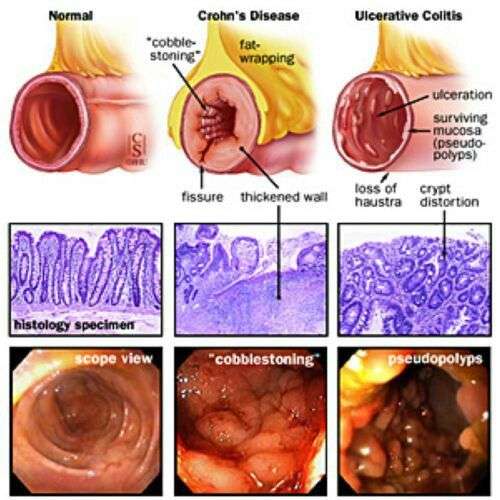
The differences between ulcerative colitis and Crohns disease are:
- Ulcerative colitis is limited to the colon while Crohns disease can occur anywhere between the mouth and the anus
- In Crohns disease, there are healthy parts of the intestine mixed in between inflamed areas. Ulcerative colitis, on the other hand, is continuous inflammation of the colon
- Ulcerative colitis only affects the inner most lining of the colon while Crohns disease can occur in all the layers of the bowel walls
Dont Miss: Budesonide Vs Prednisone For Ulcerative Colitis
When Is A Colectomy Recommended For Ulcerative Colitis
Many people with ulcerative colitis are prescribed medications, such as corticosteroids or biologics, to eliminate symptoms and treat inflammation. These medications successfully treat about 70 percent of people with UC. About one-third to one-quarter of people living with UC will need surgery to help manage their condition, however.
People with ulcerative colitis may need a colectomy if they have:
- Severe symptoms, such as extreme bleeding, perforations , or toxic megacolon
- Symptoms that dont get better with medication
- Cancer or precancerous changes in the intestine
Setting Your Browser To Accept Cookies
There are many reasons why a cookie could not be set correctly. Below are the most common reasons:
- You have cookies disabled in your browser. You need to reset your browser to accept cookies or to ask you if you want to accept cookies.
- Your browser asks you whether you want to accept cookies and you declined. To accept cookies from this site, use the Back button and accept the cookie.
- Your browser does not support cookies. Try a different browser if you suspect this.
- The date on your computer is in the past. If your computer’s clock shows a date before 1 Jan 1970, the browser will automatically forget the cookie. To fix this, set the correct time and date on your computer.
- You have installed an application that monitors or blocks cookies from being set. You must disable the application while logging in or check with your system administrator.
Recommended Reading: Natural Cure For Peptic Ulcer
Crohns Disease And Ulcerative Colitis And Diet
Diet and food allergies do not cause IBD, and long-term special diets are not effective in treating IBD. However, adjusting your diet can help manage some of your symptoms, and can help IBD medications work better. A person with IBD has to pay close attention to their diet, since they may have malnutrition.
What Is The Difference Between Collagenous Colitis And Lymphocytic Colitis
Microscopic colitis is an inflammatory bowel disease that usually starts in the colon or rectum, although it is not the same condition as Crohns disease or ulcerative colitis. It gets its name from the fact that inflammation can only be seen under a microscope during an endoscopy.
There are two forms of microscopic colitis: collagenous colitis and lymphocytic colitis. Although the two forms share many similarities under the umbrella of microscopic colitis, there are a few key differences.
Read Also: Ulcerative Colitis Abdominal Pain Relief
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Also Check: Pressure Ulcers Are Most Likely To Develop
Mild To Moderately Active Disease
Am J Gastroenterol.J Crohn’s Colitis.Gut.Cochrane Database Syst Rev.Am J Gastroenterol.J Crohn’s Colitis.Cochrane Database Syst Rev.Gut.
- Sninsky C
- et al.
Am J Gastroenterol.
- Lindgren S
- et al.
Gut.
- Dallaire C
- et al.
Can J Gastroenterol.
- Feagan BG
- et al.
Gastroenterology.Cochrane Database Syst Rev.World J Gastroenterol.J Crohn’s Colitis.Gastroenterology.BMJ.
Gut.Dig Dis Sci.N Engl J Med.
- Hommes DW
- et al.
Gut.
- Middleton S
- et al.
J Crohn’s Colitis.Am J Gastroenterol.
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
You May Like: Vsl 3 For Ulcerative Colitis
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Infectious Colitis And Cord Colitis
Infectious colitisdue to a variety of agentsmay clinically mimic UC. However, most cases of infectious colitis demonstrate a histological pattern of acute colitis, which may be diffuse, patchy, or focal, without evidence of chronicity, as evidenced by architectural distortion . Less commonly, chronic infectious colitis may produce a histological pattern of chronic active colitis resembling IBD. Most cases of infectious colitis with the chronic active colitis pattern have no specific diagnostic features on histological examination in such cases, knowledge of the clinical history and correlation with serologic studies or stool cultures are required for diagnosis. However, an important exception is amoebic colitis, in which trophozoites of entamoeba histolytica may be observed in biopsy material showing features of chronic active colitis . Amoebae should always be excluded in biopsies of suspected IBD, as these organisms may not be identified by routine stool studies and because immunosuppressive therapy for presumed IBD may result in fulminant amoebic colitis with perforation .
Amoebic colitis may mimic ulcerative colitis by a manifestation of chronic active colitis with crypt distortion, mild basal lymphoplasmatocysis , and epithelial injury . However, trophozoites of entamoeba histolytica are evident on high magnification .
Read Also: Symptoms Of Crohn’s Vs Ulcerative Colitis
Discontinuous Disease In Colectomy Specimens
In colectomy specimens, there are several circumstances in which UC may manifest a discontinuous pattern of disease, leading to a mis-diagnosis of Crohn’s disease. These include: mucosal healing in cases under treatment with either topical or oral agents, cecal and/or ascending colitis in patients with left-sided UC, appendiceal inflammation in patients with subtotal or left-sided colitis, patients with primary sclerosing cholangitis, and fulminant colitis.
Mild To Moderate Disease
First-line therapy in mild to moderate disease is the 5-ASA drugs, which can be administered as suppositories, enemas, or oral formulations . There does not appear to be any difference in efficacy or safety between different 5-ASA formulations. Sulfasalazine, which is metabolised to 5-ASA, appears to have similar efficacy to 5-ASA drugs, but tends to be less well tolerated. Patients with proctitis should be treated initially with 5-ASA suppositories since they directly target the site of inflammation and appear to be more effective than oral 5-ASA.,, In left-sided colitis, 5-ASA should be administered as an enema instead of a suppository in order to reach the splenic flexure. For patients with left-sided or extensive disease, it is recommended that oral 5-ASA be used in combination with topical 5-ASA to induce remission., Oral 5-ASA doses of 2 g or higher per day are more effective than lower doses at inducing and maintaining remission. 5-ASA can be started at a dose of 2.02.4 g per day and increased up to 4.8 g, if needed., Dosing of 5-ASA once a day has similar efficacy to divided doses and could increase adherence., Patients typically see a response within 14 days, but this response might take up to 8 weeks for symptomatic remission. 5-ASA drugs have also been shown to be effective at maintaining remission, and patients who achieve remission with 5-ASA should continue on the same medication.
You May Like: What Makes Ulcerative Colitis Worse
More Information About Ulcerative Colitis
The following are some English-language resources that may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
-
Crohn’s and Colitis Foundation of America: General information on Crohn disease and ulcerative colitis, including access to support services
-
United Ostomy Associations of America : Information and support resources for people who live with an ostomy
Treatment Of Ibd Complications
Treatment depends on the particular complication, but may include:
- complications caused by nutritional deficiencies vitamin and mineral supplements , changes to diet or a liquid diet in severe cases
- inflammation in other body areas usually ease when the bowel inflammation is controlled with medication
- fistulas small openings that often heal by themselves, with treatment to ease the inflammation. A person may need surgery to close a larger fistula. Abscesses may need antibiotics and surgical drainage
- intestinal obstruction in some cases, medical treatment to ease the inflammation will clear the obstruction. In severe cases, the person will need surgery
- toxic megacolon the person goes to hospital, and receives fluids and nutrients intravenously instead of by mouth, plus antibiotics and steroids to reduce inflammation. Sometimes, the doctor will remove the contents of the persons stomach with a slender tube . A ruptured bowel needs surgical repair or removal. In severe cases, the whole of the large bowel may need to be surgically removed.
You May Like: Snack Ideas For Ulcerative Colitis
Feeling Comfortable With Your Doctor
Its not always easy to talk about your bowel habits. Talking about poop can be embarrassing, and many people may not be ready to open up to their doctor about it.
Others may ignore the changes to their stool or think that nothing is wrong. However, ignoring symptoms will only make things worse.
Your doctor has studied the gastrointestinal tract along with all that it does and produces. They have seen and heard it all. Nothing you say about your bowel symptoms is going to offend or shock them.
Its part of their job to know about any changes in your symptoms. Your doctor is there to help you, not to judge you.
You dont have to know any fancy medical terms when talking with your doctor about your symptoms. Share your concerns and any changes in your bowel habits you have noticed. Talking with them about changes in your stool can only help get you closer to resolving the problem.
What Is Ulcerative Colitis
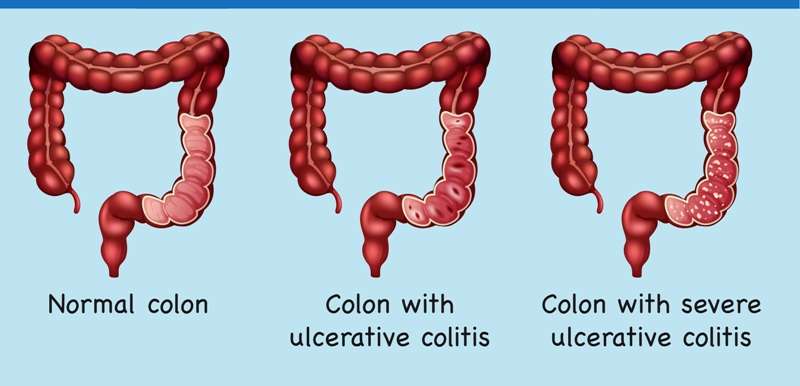
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
Also Check: What Is Best Medicine For Ulcer
Fulminant Uc In Colectomy Specimens
Fulminant colitis is defined as severe, acute inflammation of the colon with associated systemic toxicity . Most cases of fulminant colitis represent IBD, with the remainder relating to ischemia or infection, among other etiologies . Macroscopic features such as dilation, skip lesions, rectal sparing, linear ulcers, terminal ileal disease, pseudopolyps, and creeping fat are poor discriminators of UC and Crohn’s disease in setting of fulminant colitis. In particular, linear and/or fissuring ulcers and focal transmural inflammation near deeply ulcerated areas are commonly seen in the setting of fulminant UC and should not be considered to be diagnostic of Crohn’s disease or indeterminate’ colitis. Granulomas and transmural lymphoid aggregates are the two most specific indicators of Crohn’s disease in this setting .
Histological features of fulminant colitis. Fissuring ulceration and focal transmural inflammation near deeply ulcerated areas are common findings.
Difficulties In Diagnosis Of Uc
As UC-associated dysplasia may occur in endoscopically normal mucosa, extensive biopsy sampling is necessary to confidently exclude the possibility of dysplasia. In order to exclude dysplasia with 90% confidence, a minimum of 33 well-oriented jumbo forceps biopsies are required 56 such biopsies are required to achieve a 95% level of confidence . This is the rationale for surveillance programs including periodic colonoscopic examination with protocol biopsies to detect dysplasia, which has now become the standard of care for surveillance in IBD patients .
In addition to sampling error, histological evaluation of dysplasia suffers from problems of diagnostic reproducibility. Few studies have evaluated inter-observer agreement in the diagnosis of UC-associated dysplasia , none of which assessed inter-observer agreement in the context of clinical outcome, the ultimate standard of diagnosis.
You May Like: How Do They Treat Stomach Ulcers
Tips For Healthy Ulcerative Colitis Poop
There are several different approaches to UC treatment. Medications, diet, and other lifestyle changes can all help improve bowel symptoms in UC.
The foremost treatment for ulcerative colitis inflammation and related stool changes is medication. These include:
- Aminosalicylates such as Asacol or Azulfidine , to reduce inflammation
- Corticosteroids such as prednisone and Entocort EC , to reduce inflammation
- Immunomodulators such as Imuran or cyclosporine, to reduce your immune system response
- Biologic therapies such as Remicade or Simponi , to neutralize proteins made by the immune system and reduce inflammation
Your diet also plays a role in your bowel habits. After all, what goes in, must go through and come out. The following diet modifications may help reduce bowel symptoms:
- Avoid your individual trigger foods.
- Limit dairy products.
- Drink plenty of water throughout the day.
- Eat small meals.
Stress is another factor that can contribute to changes in the stool. The brain-gut connection may play a role in inflammation of the GI tract. Managing your stress levels might be able to decrease diarrhea and other changes in your stool.
In addition, participating in regular physical activity is healthy for the GI tract. Exercise helps with the movement of stools, which can be especially helpful for constipation.
Crohns Disease And Ulcerative Colitis And Digesting Food
Your mouth and stomach break down food by mechanical and chemical means. When the food has reached a pulp-like consistency, it is slowly released into the first part of the small intestine . The food is then massaged along the length of the small intestine. Organs like the pancreas and the gall bladder make digestive enzymes to further break down the food into its simpler components.
The small intestine is lined with microscopic , finger-like projections that lie close to tiny blood vessels . Nutrients pass into the bloodstream through these villi. The rest of the food is pushed into the large bowel, which absorbs excess water. The waste is then temporarily stored in the colon before it is eliminated from the anus.The two ways in which Crohns disease and ulcerative colitis disturb the digestion and absorption processes are:
- Crohns disease an inflamed ileum impairs absorption of vitamin B12 and bile salts. Inflammation along the length of the small intestine impairs absorption of all food nutrients. Inflammation of the large bowel impairs water absorption, causing diarrhoea.
- Ulcerative colitis digestion and absorption are generally not affected. Inflammation of the large bowel impairs water absorption, causing diarrhoea.
Other factors that may affect your nutritional status include:
Also Check: Stelara Dosing For Ulcerative Colitis
What Happens After You Get A Colectomy
Healing time and the long-term effects of a colectomy vary based on how much of the colon had to be removed. Some people who have only had part of the colon removed will still be able to go to the bathroom normally. Others who had larger sections removed may have to follow a new diet, avoid certain foods, or adapt to new bathroom habits.
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
You May Like: Icd 10 Stage 4 Sacral Ulcer