How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
During surgery, your small intestine will either be diverted out of an opening in your abdomen or be used to create an internal pouch that’s connected to your anus called an ileoanal pouch.
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Ulcerative Colitis And Thyroid Disease Whats The Link
Ulcerative Colitis and Thyroid Disease Ulcerative colitis and thyroid diseases are different diseases that affect different parts of the body. Ulcerative colitis is a disease of the large intestine, while thyroid diseases are abnormalities in the thyroid gland. The use of clinical trials can be used by researchers to find …
Also Check: Natural Ways To Heal Ulcerative Colitis
Ulcerative Colitis In Children: Symptoms Diagnosis And Treatment
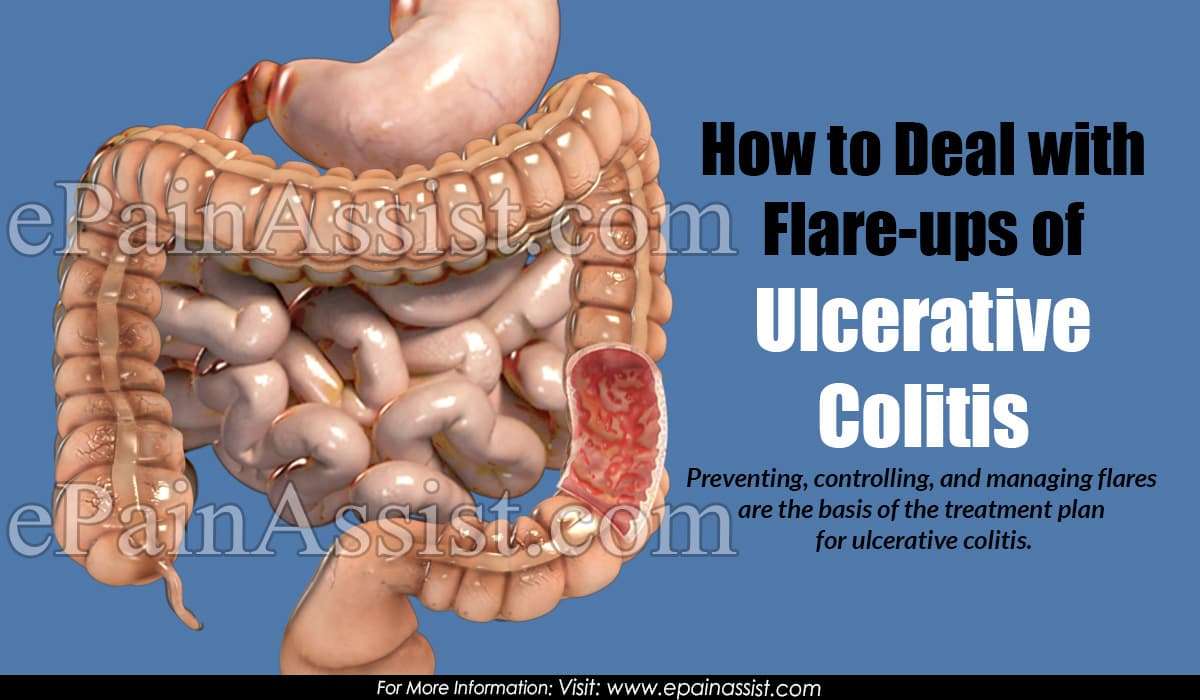
Inflammatory bowel diseases, which are chronic inflammatory conditions that affect the gastrointestinal tract, include ulcerative colitis and Crohns disease . While Crohns disease can affect any area of the GI tract, ulcerative colitis involves only the colon, also known as the large intestine. Inflammation associated with UC begins in the rectum and can involve the entire colon.
Nearly 25 percent of patients with IBD are diagnosed as children and about one-third of children with IBD have ulcerative colitis. Over the past several decades, IBD has become increasingly common.
Drinking In Moderation Is Fine If You Have Uc
If you like to have a glass of wine or beer with family and friends over a heated fall football match or a festive holiday dinner, you probably dont need to worry about your UC symptoms flaring. Theres no evidence that alcohol increases UC flares, Dr. Hong says . If boozing is a trigger for you, stick to alcohol-free versions of your top tipples.
Also Check: Ulcerative Colitis And Renal Failure
Your Uc Flare Management Plan
Your doctor may help you deal with a flare by changing your medications or offering new ones. Treatment of flares can include mesalamine products and usually a steroid, such as prednisone,” says Desi.
There are also some things you can do at home to temper a flare. These include:
During an ulcerative colitis flare, its recommended that you schedule regular visits to see your doctor, at least once every three months until the symptoms go away. After the flare has subsided, physicians recommend one or two checkups a year to manage the disease.
When an ulcerative colitis flare strikes, you have options for getting your life back on track. Its important to learn what you can about maintaining your health and work with your doctor to find the best ways to safely control UC. And remember to always let your doctor know when new or persistent symptoms arise.
When To See A Doctor
Maybe its food poisoning or a stomach bug.
I really dont want to bother the doctor.
Sound familiar? While its totally normal to want to talk yourself out of going to see your doctor, this is probably not the best approach.
Honestly, I prefer that patients tell me right away when they start having symptoms, so we can treat the flare early and often with simpler measures before it becomes more severe and more complicated or requires hospitalization, Dr. Charabaty says.
If you any ulcerative colitis symptoms flare up, call your doctor so you both can work to see whats going on and keep your symptoms from worsening. If you have severe abdominal pain and a high fever, its best to head to the emergency room, according to the Crohns and Colitis Foundation.
When you do see a doctor, this isnt a time to shy away from talking about how ulcerative colitis is affecting more than your belly, if thats the case for you.
It is really important for women with ulcerative colitis to talk about their mental health with their treating physicians and it is crucial to treat depression and anxiety as a part of a comprehensive care of IBD, Dr. Charabaty says. The mental health affects the physical health and vice versa, and both components need to be addressed to keep ulcerative colitis in remission and improve quality of life.
Read Also: Bed To Prevent Pressure Ulcers
How Crohns Disease Affects Your Body
What Is Crohns Disease? Crohns disease is an autoimmune disorder that affects ones entire gastrointestinal tract . Crohns disease can be quite chronic and because it is an inflammatory condition, it tends to lead to more severe problems and complications in the body. Crohns disease is a type of inflammatory …
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Recommended Reading: Can You Have An Ulcer In Your Colon
When To Call Your Doctor
If youre having any of the above UC symptoms, especially bloody stool, endless diarrhea, or severe pain, make an appointment with your primary-care doctor. It could always be something other than UC, but its important to get it checked out.
The sooner you treat UC and work to stop the damage to your intestinal lining and overall health, the better. If your GP suspects UC, they will likely refer you to a gastroenterologist, which is a type of physician specializing in digestive health care. This doc can further evaluate your symptoms, run any necessary tests, and get you a diagnosis.
If youve already been diagnosed with UC, call your gastro if youre experiencing any increase in symptoms like bloody stools, diarrhea, and pain, along with weight loss, fatigue, and fever.
And we totally get it. Talking about UC symptoms with your doctoror anyone!can feel awkward or embarrassing . But its hugely important that youre honest about whats going on so your doctor can get you the best treatment possible.
Many Disease Activity Indices Exist For Ulcerative Colitis But None Have Been Developed With Formal Patient Input
There is no consensus gold standard for the evaluation of disease activity in ulcerative colitis. This is illustrated in numerous recent clinical trials, in which investigators measured several different indices of disease activity, as no one index is considered sufficient. There are many indices for the measurement of ulcerative colitis disease activity, including Truelove and Witts classification of mild, moderate, and severe disease the St Marks Index, which empirically added endoscopy in 1978 simplified versions of the St Marks Index, including the Ulcerative Colitis Disease Activity Index and the Mayo Score and noninvasive versions, including the Seo Index and the Simple Clinical Colitis Activity Index .
The diversity of indices suggests that none of these has proven satisfactory, and none was developed with patient input. In addition, it has never been established that any of these indices actually measures all of the important symptoms of ulcerative colitis.
Ulcerative colitis lacks a validated measurement instrument such as the Crohns Disease Activity Index in Crohns disease . Furthermore, the indices that do exist for ulcerative colitis were not constructed in a patient-centered manner to attempt to capture the symptoms experienced by patients. Therefore, our study group aimed to investigate through focus groups that what symptoms does patients with ulcerative colitis experience during their disease process.
Read Also: How To Ease Stomach Ulcer Pain
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
How Will Ulcerative Colitis Affect Your Life

People who have ulcerative colitis for 8 years or longer also have a greater chance of getting colon cancer. The longer you have had ulcerative colitis, the greater your risk.footnote 2 Talk to your doctor about your need for cancer screening. These tests help find cancer early, when it is easier to treat.footnote 3
Ulcerative colitis can be hard to live with. During a flare-up, it may seem like you are always running to the bathroom. This can be embarrassing. And it can take a toll on how you feel about yourself. Not knowing when the disease will strike next can be stressful.
If you are having a hard time, seek support from family, friends, or a counsellor. Or look for a support group. It can be a big help to talk to others who are coping with this disease.
You May Like: How Do I Know If I Have A Peptic Ulcer
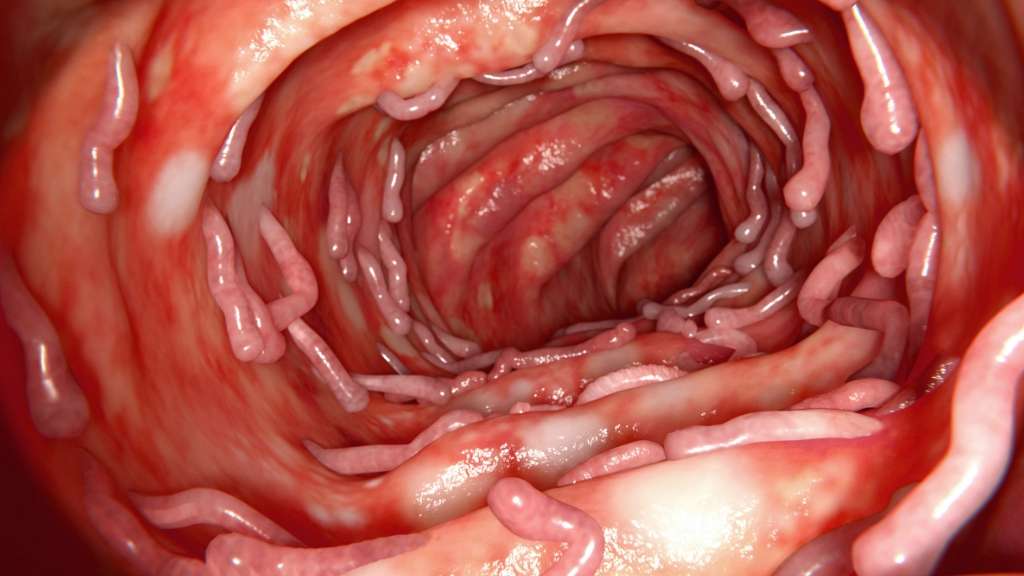
Correlation Between Disease Activity And Endoscopic Findings
There was a consensus that endoscopic findings would usually affirm patients own assessment of their level of disease activity.
Testing has always been pretty much a confirmation of how Im feeling at the time.
The colonoscopy reports and photos are basically, well, heres what this looks like and this looks like and heres the issue. So, theyre pretty in synch.
Types Of Ulcerative Colitis Remission
The best outcome you can hope for when struggling with UC is being in remission. Here are five distinct types of ulcerative remission:
Clinical Remission: This type of remission occurs when you are not experiencing UC symptoms and may feel better. However, you can still experience some of the symptoms such as bloating, constipation, and diarrhea.
Biochemical Remission: Biochemical remission occurs when no signs of inflammation are shown on blood and stool tests.
Endoscopic Remission: Intestinal lining tests show no signs of inflammation.
Histologic Remission: Both endoscopic and clinical remission come back negative for Ulcerative Colitis.
Surgical Remission: This type of remission occurs after surgery.
Also Check: How To Determine Stomach Ulcer
What Can You Do About Flare
Your situation will depend on your triggers and how your flare-ups present themselves. But first off, its crucial to listen to your docs advice and take any medication as prescribed. This can help reduce your symptoms and the risk of potentially serious complications.
To make those flare-ups feel less sh*tty, here are a few options you can try:
- taking over-the-counter pain relievers
- using a heated pad to reduce pain in your belly
- using antibacterial wet wipes on your butt to reduce your risk of infection and prevent irritation
- taking antidiarrheal meds to, well, put a pause on diarrhea
- taking a warm salt or sitz bath if your butt hurts due to an anal fistula or fissure
- using a medicinal mouthwash to manage sores
- using perianal cleaning products when you shower
- engaging in regular self-care, including exercising, getting enough sleep, and giving yourself time to de-stress
You May Like: What Happens In Ulcerative Colitis
What Are The Signs And Symptoms Of Ulcerative Colitis
First, lets review: What isulcerative colitis, anyway? This condition occurs when your large intestinethat includes your colon and your rectumis chronically inflamed. Somehow, your immune systems signals got scrambled, so the body ends up attacking healthy cells as if theyre foreign invaders. The resulting inflammation is the root cause of most of its symptoms, too.
While most people associate the digestive system and intestinal issues with UC, not all UC symptoms stem from the large intestine. Because the inflammation of UC is systemic, it can affect your entire body, leading to problems like joint pain, extreme fatigue, and morenot to mention the stress and anxiety that can come with dealing with a serious chronic disease.
Heres a quick list of the main symptoms:
-
Blood or pus in your stool
-
Frequent diarrhea
-
Tenesmus, or when you have a sudden and constant feeling that you need to have a bowel movement
-
Abdominal pain or discomfort
Recommended Reading: Is Milk Good For Ulcers
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Crohns Flare Up: Symptoms Causes Treatment And More
Flare-ups happen when there is a sudden activation of symptoms for people with crohns disease. You must frequently take drugs prescribed by your doctor as recommended. Doctors will help create treatment plans to help haste improvements. Studies show that treatment is very efficient when targeted on certain symptoms and seriousness of …
Don’t Miss: How To Treat Mouth Ulcers
What Are The Most Common Ulcerative Colitis Symptoms
Early ulcerative colitis symptoms usually include things that could easily be overlooked. Dont be afraid to talk to a doctor if youre having any worries though, even if your symptoms seem mild. If symptoms are ongoing and start to feel more severe, like persistent pain in your abdomen or unintentional weight loss, you should seek medical treatment as soon as possible.
Here are some of the most common symptoms of ulcerative colitis to watch out for, per the NIDDK:
Okay, so this isnt the most pleasant one to start with, but it is actually the most common ulcerative colitis symptomits also a pretty good tip-off that something isnt quite right and that you should schedule an appointment with your doctor. Remember those ulcers we talked about earlier? Yeah, thats where the blood in your stool comes from, and you might also see mucus in there as well.
This is another pretty common symptom, and contrary to popular belief, those ulcers in the colon are not actually what causes the pain. Instead, its a combination of abdominal cramping and bowel distension that occurs due to the inflammation in the intestines, according to a 2013 study published in Inflammatory Bowel Diseases.1
With all thats going on in the digestive tract with ulcerative colitis, nausea can sometimes be an issue. This occurs more often when symptoms are severe, or if the inflammation affects more of the large intestine, according to the NIDDK.
Anxiety And Control Over Activities
Participants acknowledged a large amount of anxiety resulting from a pattern of their symptoms controlling their lives and the resulting effects of their disease on their quality of life.
Ive got a full-blown flareup, and uh, I try and schedule things around when Ive got to go to the bathroom in a half hour, so lets not start this meeting or lets get this meeting over, um, excuse me, Ive gotta go.
if I dont go in the morning, then its in the back of my head, Ok, whens it going to hit? But if I go in the morning, right after I get up, I have no worries the rest of the day.
You end up planning your whole life around what your gut is doing.
I mean, you plan your life around it .
When it started, I just had to stay home because so often I couldnt handle it and it had absolutely no control, and when you teach, you cannot have that in the classroom.
Read Also: Can Ulcers Cause Chest Pain And Shortness Of Breath
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Moderate To Severe Symptoms
These symptoms usually require steroid medicines to control inflammation. The dose you need may be higher than that needed to treat mild symptoms. When inflammation goes away, you will take aminosalicylates to keep the condition in remission.
Severe symptoms also may be treated with:
- Immunomodulator medicines or cyclosporine. These strong medicines suppress the immune system to prevent inflammation.
- Biologics. They block the inflammatory response in your body and help reduce the inflammation in your colon. They may be used if other medicines don’t control your symptoms.
- Surgery. Removal of the large intestine cures ulcerative colitis. But surgery may not cure all of the problems that the condition can cause in other areas of the body, such as the liver and joints. Surgery also is done to treat problems such as bleeding or toxic megacolon.
Also Check: Pepto Bismol And Ulcerative Colitis